Abstract
Background
Approximately 35% of patients with midgut neuroendocrine tumors (MNET) present with distant metastases. Although successful resection of these metastatic foci improves overall survival (OS), the role of primary tumor resection (PTR) in patients with unresectable metastatic disease is unclear. The aim of this study is to evaluate prevalence and survival impact of PTR in patients with unresectable metastatic MNET.
Patients and Methods
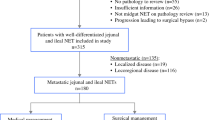
A retrospective cohort study of patients with metastatic MNET was performed using the National Cancer Database (2004–2014). Demographic and clinicopathologic variables were compared between patients who did and did not undergo PTR. Survival analysis was performed using Kaplan–Meier and log-rank tests. Multivariable regression analysis was used to assess factors associated with PTR and all-cause mortality.
Results
The cohort included 4076 patients; 2520 (61.8%) underwent PTR. Patients more likely to undergo PTR were younger and diagnosed earlier, underwent treatment at a nonacademic facility, lived on the West Coast or in the Central USA, and presented with smaller lower-grade small bowel primary tumors. Median OS was improved for patients who underwent PTR compared with those who did not (71 vs. 29 months, p < 0.001). On multivariable analysis, younger age, Black race, higher income, later year of diagnosis, treatment at an academic facility, private insurance, fewer comorbidities, small bowel primary, lower grade, and PTR (hazard ratio 0.63, 95% confidence interval 0.51–0.78, p < 0.001) were associated with lower mortality.
Conclusions
PTR was associated with improved OS. Further study is needed to understand how clinicians select patients for PTR.

Similar content being viewed by others
References
Yao JC, Hassan M, Phan A, Dagohoy C, Leary C, Mares JE, et al. One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol. 2008;26(18):3063–72.
Caplin ME, Pavel M, Ćwikła JB, Phan AT, Raderer M, Sedláčková E, et al. Lanreotide in metastatic enteropancreatic neuroendocrine tumors. N Engl J Med. 2014;371(3):224–33.
Rinke A, Muller HH, Schade-Brittinger C, Klose KJ, Barth P, Wied M, et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: a report from the PROMID Study Group. J Clin Oncol. 2009;27(28):4656–63.
Strosberg JR, Halfdanarson TR, Bellizzi AM, Chan JA, Dillon J, Heaney AP, et al. The North American Neuroendocrine Tumor Society consensus guidelines for surveillance and medical management of midgut neuroendocrine tumors. Pancreas 2017;46(6):707–14.
Kvols LK, Moertel CG, O’Connell MJ, Schutt AJ, Rubin J, Hahn RG. Treatment of the malignant carcinoid syndrome. Evaluation of a long-acting somatostatin analogue. N Engl J Med. 1986;315(11):663–6.
Mayo SC, De Jong MC, Pulitano C, Clary BM, Reddy SK, Gamblin TC, et al. Surgical management of hepatic neuroendocrine tumor metastasis: results from an international multi-institutional analysis. Ann Surg Oncol. 2010;17(12):3129–36.
Maxwell JE, Sherman SK, O’Dorisio TM, Bellizzi AM, Howe JR. Liver-directed surgery of neuroendocrine metastases: what is the optimal strategy? Surgery 2016;159(1):320–33.
Graff-Baker AN, Sauer DA, Pommier SJ, Pommier RF. Expanded criteria for carcinoid liver debulking: maintaining survival and increasing the number of eligible patients. Surgery 2014;156(6):1369–76; discussion 1376-7.
Glazer ES, Tseng JF, Al‐Refaie W, Solorzano CC, Liu P, Willborn KA, et al. Long-term survival after surgical management of neuroendocrine hepatic metastases. HPB (Oxford) 2010;12(6):427–33.
Sarmiento JM, Heywood G, Rubin J, Ilstrup DM, Nagorney DM, Que FG. Surgical treatment of neuroendocrine metastases to the liver: a plea for resection to increase survival. J Am Coll Surg. 2003;197(1):29–37.
Hellman P, Lundström T, Öhrvall U, Eriksson B, Skogseid B, Öberg K, et al. Effect of surgery on the outcome of midgut carcinoid disease with lymph node and liver metastases. World J Surg. 2002;26(8):991–7.
Citterio D, Pusceddu S, Facciorusso A, Coppa J, Milione M, Buzzoni R, et al. Primary tumour resection may improve survival in functional well-differentiated neuroendocrine tumours metastatic to the liver. Eur J Surg Oncol. 2017;43(2):380–7.
Givi B, Pommier SJ, Thompson AK, Diggs BS, Pommier RF. Operative resection of primary carcinoid neoplasms in patients with liver metastases yields significantly better survival. Surgery 2006;140(6):891–7; discussion 897-8.
Ahmed A, Turner GF, King BF, Jones L, Culliford D, McCance D, et al. Midgut neuroendocrine tumours with liver metastases: results of the UKINETS study. Endocr Relat Cancer 2009;16(3):885–94.
Capurso G, Rinzivillo M, Bettini R, Boninsegna L, Fave GD, Falconi M. Systematic review of resection of primary midgut carcinoid tumour in patients with unresectable liver metastases. Br J Surg. 2012;99(11):1480–6.
Pokuri VK, Fong MK, Iyer R. Octreotide and lanreotide in gastroenteropancreatic neuroendocrine tumors. Curr Oncol Rep. 2016;18(1):7.
Tierney JF, Chivukula SV, Wang X, Pappas SG, Schadde E, Hertl M, et al. Resection of primary tumor may prolong survival in metastatic gastroenteropancreatic neuroendocrine tumors. Surgery 2019;165(3):644–51.
Williams ED, Sandler M. The classification of carcinoid tum ours. Lancet 1963;1(7275):238–9.
Daskalakis K, Karakatsanis A, Hessman O, Stuart HC, Welin S, Janson ET, et al. Association of a prophylactic surgical approach to stage IV small intestinal neuroendocrine tumors with survival. JAMA Oncol. 2018;4(2):183–9.
Acknowledgement
The data used in the study are derived from a deidentified NCDB file. The American College of Surgeons and the Commission on Cancer have not verified and are not responsible for the analytic or statistical methodology employed or the conclusions drawn from these data by the investigator. Dr. Fei Wang is a visiting postdoctoral fellow supported by the program of China Scholarship Council.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
No authors have any potential conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Polcz, M., Schlegel, C., Edwards, G.C. et al. Primary Tumor Resection Offers Survival Benefit in Patients with Metastatic Midgut Neuroendocrine Tumors. Ann Surg Oncol 27, 2795–2803 (2020). https://doi.org/10.1245/s10434-020-08602-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08602-7