Abstract
Background
Colorectal neuroendocrine tumors are a rare malignancy, yet their incidence appears to be increasing. The optimal treatment for the high-grade subset of these tumors remains unclear. We aimed to examine the relationship between different treatment modalities and outcomes for patients with high-grade neuroendocrine carcinomas (HGNECs) of the colon and rectum.
Methods
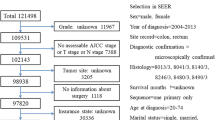
The National Cancer Database (2004–2015) was used to identify patients diagnosed with colorectal HGNECs. The primary outcome was overall survival. A Cox Proportional hazard model was used to identify risk factors for survival.
Results
Overall, 1208 patients had HGNECs; 452 (37.4%) patients had primary tumors of the rectum, and 756 (62.5%) patients had primary tumors of the colon. A total of 564 (46.7%) patients presented with stage IV disease. The median survival was 9.0 months [95% confidence interval (CI) 8.2–9.8]. In multivariable analysis, surgical resection [hazard ratio (HR) 0.54, 95% CI 0.44–0.66; p < 0.001], chemotherapy (HR 0.74, 95% CI 0.69–0.79; p < 0.001), and rectum as the primary site of tumor (HR 0.62, 95% CI 0.51–0.76; p < 0.001) were associated with better overall survival, while older age (HR 1.01, 95% CI 1.00–1.01; p = 0.02) and the presence of metastatic disease (HR 3.34, 95% CI 2.69–4.15; p < 0.001) were associated with worse survival.
Conclusions
Patients with colorectal HGNECs selected for chemotherapy and surgical resection of the primary tumor demonstrated better overall survival than those managed without resection. Patients who were able to undergo systemic chemotherapy may benefit from potentially curative resection of the primary tumor.




Similar content being viewed by others
References
Leoncini E, Boffetta P, Shafir M, Aleksovska K, Boccia S, Rindi G. Increased incidence trend of low-grade and high-grade neuroendocrine neoplasms. Endocrine. 2017;58(2):368–79.
Shafqat H, Ali S, Salhab M, Olszewski AJ. Survival of patients with neuroendocrine carcinoma of the colon and rectum: a population-based analysis. Dis Colon Rectum 2015;58(3):294–03.
Sorbye H, Strosberg J, Baudin E, Klimstra DS, Yao JC. Gastroenteropancreatic high-grade neuroendocrine carcinoma. Cancer. 2014;120(18):2814–23.
Kim JY, Hong SM, Ro JY. Recent updates on grading and classification of neuroendocrine tumors. Ann Diagn Pathol. 2017;29:11–16.
Shia J, Tang LH, Weiser MR, et al. Is nonsmall cell type high-grade neuroendocrine carcinoma of the tubular gastrointestinal tract a distinct disease entity? Am J Surg Pathol. 2008;32(5):719–31.
Bernick PE, Klimstra DS, Shia J, et al. Neuroendocrine carcinomas of the colon and rectum. Dis Colon Rectum. 2004;47(2):163–69.
Sorbye H, Welin S, Langer SW, et al. Predictive and prognostic factors for treatment and survival in 305 patients with advanced gastrointestinal neuroendocrine carcinoma (WHO G3): the NORDIC NEC study. Ann Oncol. 2013;24(1):152–60.
Brenner B, Shah MA, Gonen M, Klimstra DS, Shia J, Kelsen DP. Small-cell carcinoma of the gastrointestinal tract: a retrospective study of 64 cases. Br J Cancer. 2004;90(9):1720–26.
Walenkamp AM, Sonke GS, Sleijfer DT. Clinical and therapeutic aspects of extrapulmonary small cell carcinoma. Cancer Treat Rev. 2009;35(3):228–36.
Garcia-Carbonero R, Sorbye H, Baudin E, et al. ENETS Consensus guidelines for high-grade gastroenteropancreatic neuroendocrine tumors and neuroendocrine carcinomas. Neuroendocrinology. 2016;103(2):186–94.
Smith JD, Reidy DL, Goodman KA, Shia J, Nash GM. A retrospective review of 126 high-grade neuroendocrine carcinomas of the colon and rectum. Ann Surg Oncol. 2014;21(9):2956–62.
Chung TP, Hunt SR. Carcinoid and neuroendocrine tumors of the colon and rectum. Clin Colon Rectal Surg. 2006;19(2):45–8.
Conte B, George B, Overman M, et al. High-grade neuroendocrine colorectal carcinomas: a retrospective study of 100 patients. Clin Colorectal Cancer. 2016;15(2):e1–e7.
Aytac E, Ozdemir Y, Ozuner G. Long term outcomes of neuroendocrine carcinomas (high-grade neuroendocrine tumors) of the colon, rectum, and anal canal. J Visc Surg. 2014;151(1):3–7.
Winchester DP, Stewart AK, Phillips JL, Ward EE. The national cancer data base: past, present, and future. Ann Surg Oncol. 2010;17(1):4–7.
Ahlman H, Nilsson O, McNicol AM, et al. Poorly-differentiated endocrine carcinomas of midgut and hindgut origin. Neuroendocrinology. 2008;87(1):40–46.
Balasubramanyam S, O’Donnell BP, Musher BL, Jhaveri PM, Ludwig MS. Evaluating treatment patterns for small cell carcinoma of the colon using the national cancer database (NCDB). J Gastrointest Cancer. 2018. https://doi.org/10.1007/s12029-018-0054-y.
Kunz PL, Reidy-Lagunes D, Anthony LB, et al. Consensus guidelines for the management and treatment of neuroendocrine tumors. Pancreas. 2013;42(4):557–77.
Yamaguchi T, Machida N, Morizane C, et al. Multicenter retrospective analysis of systemic chemotherapy for advanced neuroendocrine carcinoma of the digestive system. Cancer Sci. 2014;105(9):1176–81.
Hung SS. Small cell carcinoma of the colon. A case report and literature review. J Clin Gastroenterol. 1989;11(3):335–39.
Arnold R. Endocrine tumours of the gastrointestinal tract Introduction: definition, historical aspects, classification, staging, prognosis and therapeutic options. Best Pract Res Clin Gastroenterol. 2005;19(4):491–05.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the design of the work, drafted the work, approved the final version submitted for publication, and agreed to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
None. No grant support or financial relationships were received for this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Adam C. Fields and Pamela Lu MD were co-first authors on this work.
Rights and permissions
About this article
Cite this article
Fields, A.C., Lu, P., Vierra, B.M. et al. Survival in Patients with High-Grade Colorectal Neuroendocrine Carcinomas: The Role of Surgery and Chemotherapy. Ann Surg Oncol 26, 1127–1133 (2019). https://doi.org/10.1245/s10434-019-07203-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07203-3