Abstract
Background
Occult breast cancer (OBC) is rare and optimal local–regional (LR) management has not been defined. Using a patient registry database, we examine factors associated with treatment and outcomes in OBC.
Methods
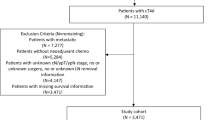
Female patients with cT0 N1/2 M0 BC were selected from the National Cancer Database (2004–2013) and categorized into four treatment groups: MAST = mastectomy with axillary lymph node dissection (ALND) ± radiation (RT); RT + ALND = RT with ALND, no breast surgery; ALND = ALND alone; OBS = no breast surgery, RT, or ALND. Patient characteristics and overall survival (OS) were compared between groups, and multivariable analysis was used to identify factors associated with treatment and OS.
Results
Among 2.03 million BC cases, 1853 females (0.09%) with cT0 N1/2 M0 disease were identified and 1231 patients were categorized into a treatment group: MAST = 592, RT + ALND = 342, ALND = 106, OBS = 191. On logistic regression, care at an academic center was associated with a higher likelihood of RT + ALND compared with MAST (odds ratio 2.03, 95% confidence interval [CI] 1.50–2.74, p < 0.001). Patients treated with RT + ALND had significantly better OS on univariate survival analysis compared with patients treated with MAST (hazard ratio [HR] 0.475, 95% CI 0.306–0.736, p = 0.001). RT + ALND was independently associated with OS on multivariable survival analysis (HR 0.509, 95% CI 0.321–0.808, p = 0.004), after adjusting for covariates.
Conclusions
Patients with OBC were more likely to undergo RT + ALND if they received care at an academic center. Patients treated with RT + ALND had significantly better OS compared with patients treated with MAST, after adjusting for covariates. This supports the use of RT + ALND as LR treatment for patients with OBC.

Similar content being viewed by others
References
Walker GV, Smith GL, Perkins GH, et al. Population-based analysis of occult primary breast cancer with axillary lymph node metastasis. Cancer. 2010;116(17):4000–4006.
Macedo FI, Eid JJ, Flynn J, Jacobs MJ, Mittal VK. Optimal surgical management for occult breast carcinoma: a meta-analysis. Ann Surgical Oncol. 2016;23(6):1838–1844.
National Comprehensive Cancer Network. NCCN Guidelines Version 1.2017 Invasive Breast Cancer. 2017. Available at: https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Accessed 26 Mar 2017.
American Society of Breast Surgeons. Performance and Practice Guidelines for Axillary Lymph Node Dissection in Breast Cancer Patients. 2014. Available at: https://www.breastsurgeons.org/statements/guidelines/PerformancePracticeGuidelines_ALND.pdf. Accessed Mar 26 2017.
Bilimoria KY, Stewart AK, Winchester DP, Ko CY. The National Cancer Data Base: a powerful initiative to improve cancer care in the United States. Ann Surg Oncol. 2008;15(3):683–690.
He M, Tang LC, Yu KD, et al. Treatment outcomes and unfavorable prognostic factors in patients with occult breast cancer. Eur J Surg Oncol. 2012;38(11):1022–1028.
Shannon C, Walsh G, Sapunar F, A’Hern R, Smith I. Occult primary breast carcinoma presenting as axillary lymphadenopathy. Breast. 2002;11(5):414–418.
Foroudi F, Tiver KW. Occult breast carcinoma presenting as axillary metastases. Int J Radiat Oncol Biol Phys. 2000;47(1):143–147.
Wang X, Zhao Y, Cao X. Clinical benefits of mastectomy on treatment of occult breast carcinoma presenting axillary metastases. Breast J. 2010;16(1):32–37.
Blanchard DK, Farley DR. Retrospective study of women presenting with axillary metastases from occult breast carcinoma. World J Surg. 2004;28(6):535–539.
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet. 2011;378(9804):1707–1716.
McGale P. Effect of radiotherapy after mastectomy and axillary surgery on 10-year recurrence and 20-year breast cancer mortality: meta-analysis of individual patient data for 8135 women in 22 randomised trials. Lancet. 2014;383(9935):2127–2135.
Khandelwal AK, Garguilo GA. Therapeutic options for occult breast cancer: a survey of the American Society of Breast Surgeons and review of the literature. Am J Surg. 2005;190(4):609–613.
Rosen PP, Kimmel M. Occult breast carcinoma presenting with axillary lymph node metastases: a follow-up study of 48 patients. Hum Pathol. 1990;21(5):518–523.
Olson JA Jr, Morris EA, Van Zee KJ, Linehan DC, Borgen PI. Magnetic resonance imaging facilitates breast conservation for occult breast cancer. Ann Surg Oncol. 2000;7(6):411–415.
Buchanan CL, Morris EA, Dorn PL, Borgen PI, Van Zee KJ. Utility of breast magnetic resonance imaging in patients with occult primary breast cancer. Ann Surg Oncol. 2005;12(12):1045–1053.
Morris EA, Schwartz LH, Dershaw DD, van Zee KJ, Abramson AF, Liberman L. MR imaging of the breast in patients with occult primary breast carcinoma. Radiology. 1997;205(2):437–440.
de Bresser J, de Vos B, van der Ent F, Hulsewe K. Breast MRI in clinically and mammographically occult breast cancer presenting with an axillary metastasis: a systematic review. Eur J Surg Oncol. 2010;36(2):114–119.
Diclosure
Lindsay K. Hessler, Jason K. Molitoris, Paula Y. Rosenblatt, Emily C. Bellavance, Elizabeth M. Nichols, Katherine H.R. Tkaczuk, Steven J. Feigenberg, Soren M. Bentzen, and Susan B. Kesmodel declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Drs. Lindsay Hessler and Jason Molitoris have contributed equally to this article.
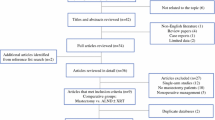
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hessler, L.K., Molitoris, J.K., Rosenblatt, P.Y. et al. Factors Influencing Management and Outcome in Patients with Occult Breast Cancer with Axillary Lymph Node Involvement: Analysis of the National Cancer Database. Ann Surg Oncol 24, 2907–2914 (2017). https://doi.org/10.1245/s10434-017-5928-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-017-5928-x