Abstract
Background
Optimal outcomes in pseudomyxoma peritonei (PMP) require complete macroscopic tumor removal by cytoreductive surgery (CRS) combined with hyperthermic intraperitoneal chemotherapy (HIPEC). Partial or complete gastrectomy may be required with ongoing debate as to the risks and benefits of gastrectomy in what is often a low-grade malignancy.
Methods
Retrospective single-center analysis of 1014 patients undergoing CRS and HIPEC for PMP of appendiceal origin. Complications and survival were compared in patients who had gastrectomy versus the nongastrectomy cohort.
Results
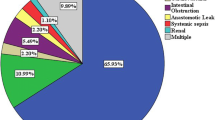
Of 1014 patients, 747 (74 %) had CRS and HIPEC with complete cytoreduction. Overall, 86 (12 %) of 747 had partial (n = 80) or total (n = 6) gastrectomy. Median age was 55 years for gastrectomy patients and 56 for nongastrectomy patients (p = 0.591). Preoperative tumor markers [carcinoembryonic antigen, carbohydrate antigen (CA) 125 and CA19-9] were elevated more frequently in the gastrectomy group compared to the nongastrectomy group [81, 61 and 81 % compared to 41 % (p = 0.001), 20 % (p = 0.001) and 39 % (p = 0.001), respectively]. The proportion of high-grade histology was similar in the two groups (gastrectomy 19 % vs. nongastrectomy 18 %, p = 0.882). Postoperative complications (Clavien–Dindo III–IV) were 31 % for the gastrectomy group and 13 % for the nongastrectomy group (p = 0.001). The 30-day postoperative mortality was 3 (0.5 %) of 661 for the nongastrectomy group and 1 (1.2 %) of 86 for the gastrectomy group (p = 0.387). Three- and 5-year overall survival were 96 and 88 % in the nongastrectomy group and 87 and 77 % in the gastrectomy group (p = 0.018). Three- and 5-year disease-free survival were 89 and 77 % in the nongastrectomy group versus 66 and 48 % in the gastrectomy group (p = 0.001).
Conclusions
Gastrectomy is an essential component of complete cytoreduction in advanced PMP and was required in 12 % of patients with good long-term survival.



Similar content being viewed by others
References
Smeenk RM, van Velthuysen ML, Verwaal VJ, Zoetmulder FA. Appendiceal neoplasm sans pseudomyxoma peritonei: a population based study. Eur J Surg Oncol. 2008;34:196–201.
Sugarbaker PH. Cytoreductive surgery and perioperative intraperitoneal chemotherapy: a new standard of care for appendiceal mucinous tumors with peritoneal dissemination. Clin Colon Rectal Surg. 2005;18:204–14.
Moran BJ, Cecil TD. The etiology, clinical presentation and management of pseudomyxoma peritonei. Surg Oncol Clin N Am. 2003;12:585–603.
Moran B, Cecil T, Chandrakumaran K, Arnold S, Mohamed F, Venkatasubramaniam A. The results of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy in 1200 patients with peritoneal malignancy. Colorectal Dis. 2015;17:772–8.
Kusamura S, Moran BJ, Sugarbaker PH, et al. Multicentre study of the learning curve and surgical performance of cytoreductive surgery with intraperitoneal chemotherapy for pseudomyxoma peritonei. Br J Surg. 2014;101:1758–65.
Smeenk RM, Verwaal VJ, Zoetmulder FA. Pseudomyxoma peritonei. Cancer Treat Rev. 2007;33:138–45.
Sugarbaker PH. New standard of care for appendiceal epithelial neoplasms and pseudomyxoma peritonei syndrome? Lancet Oncol. 2006;7:69–76.
Carr NJ, Cecil TD, Mohamed F, et al. A consensus for classification and pathologic reporting of pseudomyxoma peritonei and associated appendiceal neoplasia: the results of the Peritoneal Surface Oncology Group International (PSOGI) modified Delphi process. Am J Surg Pathol. 2016;40:14–26.
Taflampas P, Dayal S, Chandakumaran K, Mohamed F, Cecil TD, Moran BJ. Pre-operative tumour marker status predicts recurrence and survival after complete cytoreduction and hyperthermic intraperitoneal chemotherapy for appendiceal pseudomyxoma peritonei: analysis on 519 patients. Eur J Surg Oncol. 2014;40:515–20.
Kusamura S, Hutanu I, Baratti D, Deraco M. Circulating tumour markers: predictors of incomplete cytoreduction and powerful determinants of outcome in pseudomyxoma peritonei. J Surg Oncol. 2013;108:1–8.
Koh J, Liauw W, Chua T, Morris DL. Carbohydrate antigen 19-9 (CA19-9) is an independent prognostic indicator in pseudomyxoma peritonei post cytoreductive surgery and perioperative intraperitoneal chemotherapy. J Gastrointest Oncol. 2013;4:173–81.
Alexander-Sefre F, Chandrakumaran K, Banerjee S, Sexton R, Thomas JM, Moran B. Elevated tumour markers prior to complete tumour removal in patients with pseudomyxoma peritonei predict early recurrence. Colorectal Dis. 2005;7:382–6.
Di Fabio F, Aston W, Mohamed F, Chandrakumaran K, Cecil T, Moran B. Elevated tumour markers are normalized in most patients with pseudomyxoma peritonei one week after complete tumour removal. Colorectal Dis. 2015;17:698–703.
Lord AC, Shihab O, Chandrakumaran K, Mohamed F, Cecil TD, Moran BJ. Recurrence and outcome after complete tumour removal and hyperthermic intraperitoneal chemotherapy in 512 patients with pseudomyxoma peritonei from perforated appendiceal mucinous tumours. Eur J Surg Oncol. 2015;41:396–9.
Sugarbaker PH. Cytoreduction including total gastrectomy for pseudomyxoma peritonei. Br J Surg. 2002;89:208–12.
Piso P, Slowik P, Popp F, Dahlke MH, Glockzin G, Schlitt HJ. Safety of gastric resections during cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for peritoneal carcinomatosis. Ann Surg Oncol. 2009;16:2188–94.
Sugarbaker PH, editor. Peritoneal carcinomatosis: principles of management. Boston: Kluwer; 1996. p. 368.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Delhorme JB, Elias D, Varatharajah S, et al. Can a benefit be expected from surgical debulking of unresectable pseudomyxoma peritonei? Ann Surg Oncol. 2016;23:1618–24.
Dayal S, Taflampas P, Riss S, et al. Complete cytoreduction for pseudomyxoma peritonei is optimal but maximal tumor debulking may be beneficial in patients in whom complete tumor removal cannot be achieved. Dis Colon Rectum. 2013;56:1366–72.
Disclosure
The authors have no conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Francesco Di Fabio and Akash Mehta have contributed equally to this article.
Rights and permissions
About this article
Cite this article
Di Fabio, F., Mehta, A., Chandrakumaran, K. et al. Advanced Pseudomyxoma Peritonei Requiring Gastrectomy to Achieve Complete Cytoreduction Results in Good Long-Term Oncologic Outcomes. Ann Surg Oncol 23, 4316–4321 (2016). https://doi.org/10.1245/s10434-016-5389-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5389-7