Abstract
Background
The current tumor-node-metastasis staging system for the pancreas does not incorporate the number of lymph nodes (LNs) with metastasis.
Methods
Among 1649 pancreaticoduodenectomies, 227 stringently defined pancreatic ductal adenocarcinomas (PDACs) that had undergone a specific approach of LN harvesting were analyzed for the prognostic value of LN substaging protocols used for other gastrointestinal (GI) organs.
Results
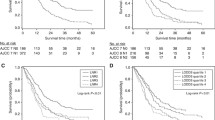
The median number of LNs harvested was 18, and the median number of LNs with metastasis was 3. Lymph node metastasis was detected in 175 cases (77 %). The number of LNs involved correlated significantly with clinical outcome. When cases were substaged with the protocol already in use for the upper GI organs (N0: no metastasis, N1: metastasis to 1–2 LNs; N2: metastasis to ≥3 LNs), the median overall survival times were 35, 21, and 18 months, and the respective 3-year survival rates were 46, 34, and 20 % (p = 0.004). Analysis of the Surveillance, Epidemiology and End Results (SEER) database also confirmed the survival differences between these substages (median overall survival times of 23, 15, and 14 months and respective 3-year survival rates of 37, 22, and 18 %; p < 0.0001). The substaging protocol for the lower GI organs (N0: no metastasis; N1: metastasis to 1–3 LNs; N2: metastasis to ≥4 LNs) also was significant, with median overall survival times of 35, 21, 18 months and respective 3-year survival rates of 46, 26, and 23 %; p = 0.009). The association between higher N stage and shorter survival persisted with multivariate modeling for both protocols, although the prognostic value of the upper GI protocol appeared to be slightly stronger according to the Akaike Information Criterion method.
Conclusion
In conclusion, with proper LN harvesting, the LN metastasis rate in PDACs is very high (77 %). Substaging of LN metastasis has significant prognostic value and needs to be considered in the N staging of PDACs. The protocol already in use for other upper GI tract organs, which currently also is proven significant for ampulla, would be preferable, although the lower GI tract protocol also is applicable.


Similar content being viewed by others
References
Edge S, Byrd DR, Campton CC, Fritz AG, Greene FL, Trotti A. AJCC Cancer Staging Manual. 7 ed. Springer, New York, 2010.
Kang HJ, Eo SH, Kim SC, et al. Increased number of metastatic lymph nodes in adenocarcinoma of the ampulla of Vater as a prognostic factor: a proposal of new nodal classification. Surgery. 2014;155:74–84.
Falconi M, Crippa S, Dominguez I, et al. Prognostic relevance of lymph node ratio and number of resected nodes after curative resection of ampulla of Vater carcinoma. Ann Surg Oncol. 2008;15:3178–86.
Roland CL, Katz MH, Gonzalez GM, et al. A high positive lymph node ratio is associated with distant recurrence after surgical resection of ampullary carcinoma. J Gastrointest Surg. 2012;16:2056–63.
Balci S, Basturk O, Saka B, et al. Substaging nodal status in ampullary carcinomas has significant prognostic value: proposed revised staging based on an analysis of 313 well-characterized cases. Ann Surg Oncol. 2015.
Strobel O, Hinz U, Gluth A, et al. Pancreatic adenocarcinoma: number of positive nodes allows to distinguish several N categories. Ann Surg. 2015;261:961–9.
Fouquet T, Germain A, Brunaud L, Bresler L, Ayav A. Is perineural invasion more accurate than other factors to predict early recurrence after pancreatoduodenectomy for pancreatic head adenocarcinoma? World J Surg. 2014;38:2132–7.
Jamieson NB, Denley SM, Logue J, et al. A prospective comparison of the prognostic value of tumor- and patient-related factors in patients undergoing potentially curative surgery for pancreatic ductal adenocarcinoma. Ann Surg Oncol. 2011;18:2318–28.
Moghanaki D, Mick R, Furth EE, et al. Resection status, age, and nodal involvement determine survival among patients receiving adjuvant chemoradiotherapy in pancreatic adenocarcinoma. Jop. 2011;12:438–44.
Kanda M, Fujii T, Nagai S, et al. Pattern of lymph node metastasis spread in pancreatic cancer. Pancreas. 2011;40:951–5.
Nakagohri T, Kinoshita T, Konishi M, Takahashi S, Gotohda N. Nodal involvement is strongest predictor of poor survival in patients with invasive adenocarcinoma of the head of the pancreas. Hepatogastroenterology. 2006;53:447–51.
House MG, Gonen M, Jarnagin WR, et al. Prognostic significance of pathologic nodal status in patients with resected pancreatic cancer. J Gastrointest Surg. 2007;11:1549–55.
Pai RK, Beck AH, Mitchem J, et al. Pattern of lymph node involvement and prognosis in pancreatic adenocarcinoma: direct lymph node invasion has similar survival to node-negative disease. Am J Surg Pathol. 2011;35:228–34.
Winter JM, Cameron JL, Campbell KA, et al. 1423 pancreaticoduodenectomies for pancreatic cancer: a single-institution experience. J Gastrointest Surg. 2006;10:1199–210; discussion 1210–191.
Richter A, Niedergethmann M, Sturm JW, Lorenz D, Post S, Trede M. Long-term results of partial pancreaticoduodenectomy for ductal adenocarcinoma of the pancreatic head: 25-year experience. World J Surg. 2003;27:324–9.
Kang MJ, Jang JY, Chang YR, Kwon W, Jung W, Kim SW. Revisiting the concept of lymph node metastases of pancreatic head cancer: number of metastatic lymph nodes and lymph node ratio according to N stage. Ann Surg Oncol. 2014;21:1545–51.
Konstantinidis IT, Deshpande V, Zheng H, et al. Does the mechanism of lymph node invasion affect survival in patients with pancreatic ductal adenocarcinoma? J Gastrointest Surg. 2010;14:261–7.
Gleisner AL, Spolverato G, Ejaz A, Pawlik TM. Time-related changes in the prognostic significance of the total number of examined lymph nodes in node-negative pancreatic head cancer. J Surg Oncol. 2014;110(7):858–63.
Asiyanbola B, Gleisner A, Herman JM, et al. Determining pattern of recurrence following pancreaticoduodenectomy and adjuvant 5-flurouracil-based chemoradiation therapy: effect of number of metastatic lymph nodes and lymph node ratio. J Gastrointest Surg. 2009;13:752–759.
Sohn TA, Yeo CJ, Cameron JL, et al. Resected adenocarcinoma of the pancreas-616 patients: results, outcomes and prognostic indicators. J Gastrointest Surg.. 2000;4:567–79.
Clark EJ, Taylor MA, Connor S, et al. Validation of a prognostic nomogram in patients undergoing resection for pancreatic ductal adenocarcinoma in a UK tertiary referral centre. HPB Oxford. 2008;10:501–5.
Buc E, Couvelard A, Kwiatkowski F, et al. Adenocarcinoma of the pancreas: does prognosis depend on mode of lymph node invasion? Eur J Surg Oncol. 2014;40:1578–85.
Showalter TN, Winter KA, Berger AC, et al. The influence of total nodes examined, number of positive nodes, and lymph node ratio on survival after surgical resection and adjuvant chemoradiation for pancreatic cancer: a secondary analysis of RTOG 9704. Int J Radiat Oncol Biol Phys. 2011;81:1328–35.
Murakami Y, Uemura K, Sudo T, et al. Number of metastatic lymph nodes, but not lymph node ratio, is an independent prognostic factor after resection of pancreatic carcinoma. J Am Coll Surg. 2010;211:196–204.
Sergeant G, Ectors N, Fieuws S, Aerts R, Topal B. Prognostic relevance of extracapsular lymph node involvement in pancreatic ductal adenocarcinoma. Ann Surg Oncol. 2009;16:3070–9.
Riediger H, Keck T, Wellner U, et al. The lymph node ratio is the strongest prognostic factor after resection of pancreatic cancer. J Gastrointest Surg. 2009;13:1337–44.
Sierzega M, Popiela T, Kulig J, Nowak K. The ratio of metastatic/resected lymph nodes is an independent prognostic factor in patients with node-positive pancreatic head cancer. Pancreas. 2006;33:240–5.
Berger AC, Watson JC, Ross EA, Hoffman JP. The metastatic/examined lymph node ratio is an important prognostic factor after pancreaticoduodenectomy for pancreatic adenocarcinoma. Am Surg. 2004;70:235–40; discussion 240.
Dusch N, Weiss C, Strobel P, Kienle P, Post S, Niedergethmann M. Factors predicting long-term survival following pancreatic resection for ductal adenocarcinoma of the pancreas: 40 years of experience. J Gastrointest Surg. 2014;18:674–81.
Slidell MB, Chang DC, Cameron JL, et al. Impact of total lymph node count and lymph node ratio on staging and survival after pancreatectomy for pancreatic adenocarcinoma: a large, population-based analysis. Ann Surg Oncol. 2008;15:165–74.
Opfermann KJ, Wahlquist AE, Garrett-Mayer E, Shridhar R, Cannick L, Marshall DT. Adjuvant radiotherapy and lymph node status for pancreatic cancer: results of a study from the Surveillance, Epidemiology, and End Results (SEER) Registry data. Am J Clin Oncol. 2012;37(2):112-6.
He J, Ahuja N, Makary MA, et al. 2564 resected periampullary adenocarcinomas at a single institution: trends over three decades. HPB Oxford. 2014;16:83–90.
Winter JM, Brennan MF, Tang LH, et al. Survival after resection of pancreatic adenocarcinoma: results from a single institution over three decades. Ann Surg Oncol. 2012;19:169–75.
Tomlinson JS, Jain S, Bentrem DJ, et al. Accuracy of staging node-negative pancreas cancer: a potential quality measure. Arch Surg. 2007;142:767–723; discussion 773–764.
Schwarz RE, Smith DD. Extent of lymph node retrieval and pancreatic cancer survival: information from a large U.S. population database. Ann Surg Oncol. 2006;13:1189–200.
Verbeke CS, Leitch D, Menon KV, McMahon MJ, Guillou PJ, Anthoney A. Redefining the R1 resection in pancreatic cancer. Br J Surg. 2006;93:1232–7.
Verbeke CS, Menon KV. Redefining resection margin status in pancreatic cancer. HPB Oxford. 2009;11:282–9.
Maksymov V, Hogan M, Khalifa MA. An anatomical-based mapping analysis of the pancreaticoduodenectomy retroperitoneal margin highlights the urgent need for standardized assessment. HPB Oxford. 2013;15:218–23.
Adsay NV, Basturk O, Saka B, et al. Whipple made simple for surgical pathologists: orientation, dissection, and sampling of pancreaticoduodenectomy specimens for a more practical and accurate evaluation of pancreatic, distal common bile duct, and ampullary tumors. Am J Surg Pathol. 2014;38:480–93.
Adsay NV, Basturk O, Altinel D, et al. The number of lymph nodes identified in a simple pancreatoduodenectomy specimen: comparison of conventional vs orange-peeling approach in pathologic assessment. Mod Pathol. 2009;22:107–12.
Bilimoria KY, Bentrem DJ, Lillemoe KD, Talamonti MS, Ko CY, Pancreatic Cancer Quality Indicator Development Expert Panel ACoS: assessment of pancreatic cancer care in the United States based on formally developed quality indicators. J Natl Cancer Inst. 2009;101:848–59.
Gonzalez RS, Bagci P, Kong KT, et al. Distal common bile duct adenocarcinoma: analysis of 47 cases and comparison with pancreatic and ampullary ductal carcinomas (abstract). Mod Pathol. 2012;25:109A.
Saka B, Tajiri T, Ohike N, et al. Clinicopathologic comparison of ampullary versus pancreatic carcinoma: preinvasive component, size of invasion, stage, resectability and histologic phenotype are the factors for the significantly favorable outcome of ampullary carcinoma. Mod Pathol. 2013;26:429A–429A.
Gutierrez JC, Franceschi D, Koniaris LG. How many lymph nodes properly stage a periampullary malignancy? J Gastrointest Surg. 2008;12:77–85.
Valsangkar NP, Bush DM, Michaelson JS, et al. N0/N1, PNL, or LNR? The effect of lymph node number on accurate survival prediction in pancreatic ductal adenocarcinoma. J Gastrointest Surg. 2013;17:257–66.
Brennan MF, Kattan MW, Klimstra D, Conlon K. Prognostic nomogram for patients undergoing resection for adenocarcinoma of the pancreas. Ann Surg. 2004;240:293–8.
Pawlik TM, Gleisner AL, Cameron JL, et al. Prognostic relevance of lymph node ratio following pancreaticoduodenectomy for pancreatic cancer. Surgery. 2007;141:610–18.
Opfermann KJ, Wahlquist AE, Garrett-Mayer E, Shridhar R, Cannick L, Marshall DT. Adjuvant radiotherapy and lymph node status for pancreatic cancer: results of a study from the Surveillance, Epidemiology, and End Results (SEER) Registry data. Am J Clin Oncol. 2014;37:112–6.
Huebner M, Kendrick M, Reid-Lombardo KM, et al. Number of lymph nodes evaluated: prognostic value in pancreatic adenocarcinoma. J Gastrointest Surg. 2012;16:920–6.
Esposito I, Kleeff J, Bergmann F, et al. Most pancreatic cancer resections are R1 resections. Ann Surg Oncol. 2008;15:1651–60.
Hartwig W, Hackert T, Hinz U, et al. Pancreatic cancer surgery in the new millennium: better prediction of outcome. Ann Surg. 2011;254:311–9.
Lash TL, Cole SR. Immortal person-time in studies of cancer outcomes. J Clin Oncol. 2009;27:e55–6.
Ashfaq A, Pockaj BA, Gray RJ, Halfdanarson TR, Wasif N. Nodal counts and lymph node ratio impact survival after distal pancreatectomy for pancreatic adenocarcinoma. J Gastrointest Surg. 2014;18:1929–35.
Yamamoto Y, Ikoma H, Morimura R, et al. The clinical impact of the lymph node ratio as a prognostic factor after resection of pancreatic cancer. Anticancer Res. 2014;34:2389–94.
Wentz SC, Zhao ZG, Shyr Y, et al. Lymph node ratio and preoperative CA 19-9 levels predict overall survival and recurrence-free survival in patients with resected pancreatic adenocarcinoma. World J Gastrointest Oncol. 2012;4:207–15.
Robinson SM, Rahman A, Haugk B, et al. Metastatic lymph node ratio as an important prognostic factor in pancreatic ductal adenocarcinoma. Eur J Surg Oncol. 2012;38:333–9.
La Torre M, Cavallini M, Ramacciato G, et al. Role of the lymph node ratio in pancreatic ductal adenocarcinoma: impact on patient stratification and prognosis. J Surg Oncol. 2011;104:629–33.
Acknowledgments
This study was supported in part by a grant from National Institutes of Health (#5P50 CA62924) awarded to Volkan Adsay. Lauren M. Postlewait has received funding from the Katz Foundation. For the remaining authors, no support was declared.
Conflict of interest
There are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Basturk, O., Saka, B., Balci, S. et al. Substaging of Lymph Node Status in Resected Pancreatic Ductal Adenocarcinoma Has Strong Prognostic Correlations: Proposal for a Revised N Classification for TNM Staging. Ann Surg Oncol 22 (Suppl 3), 1187–1195 (2015). https://doi.org/10.1245/s10434-015-4861-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4861-0