Abstract
Background
Minimally invasive (laparoscopic and robotic) surgery (MIS) for colorectal cancer is associated with improved outcomes. We sought to characterize possible disparities in surgical approach and outcomes.
Patients and Methods
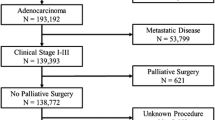
In this cross-sectional study, colorectal adenocarcinoma cases among non-Hispanic white (NHW), non-Hispanic Black (NHB), and Hispanic patients were identified using the National Cancer Database (2010–2017). Logistic and Poisson regressions, generalized logit models, and Cox proportional hazards were used to assess outcomes, with reclassification of surgery type if converted to open.
Results
NHB patients were less likely to undergo robotic surgery. After multivariable analysis, NHB patients were 6% less likely, while Hispanic patients were 12% more likely to undergo a MIS approach. Lymph node retrieval was higher (> 1.3% more, p < 0.0001) and length of stay was shorter (> 17% shorter, p < 0.0001) for MIS approaches. Unplanned readmission was lower for MIS colon cancer operations compared with open operations, but not for rectal cancer. Race/ethnicity-adjusted risk of death was lower with MIS approaches for colon as well as rectal cancer. After adjusting for surgery type, risk of death was 12% lower for NHB and 35% lower for Hispanic patients compared with NHW patients. Hispanic patients had 21% lower risk of death, while NHB patients had 12% higher risk of death than NHW patients with rectal cancer, after adjusting for surgery type.
Conclusions
Racial/ethnic disparities exist in utilization of MIS for colorectal cancer treatment, disproportionately affecting NHB patients. Since MIS has the potential to improve outcomes, suboptimal access may contribute to harmful and thus unacceptable disparities in survivorship.

Similar content being viewed by others
References
Aibuedefe B, Hamilton KS, Yong V, Kling SM, Zhao H, Poggio JL. It’s not about the money: continued treatment and survival outcome disparities in minority rectal cancer patients after controlling for socioeconomic factors. Ann Surg Oncol. 2022;29(8):5056–62. https://doi.org/10.1245/s10434-022-11474-8.
Azin A, Guidolin K, Chadi SA, Quereshy FA. Racial disparities in colon cancer survival: a propensity score matched analysis in the United States. Surgery. 2022;171(4):873–81.
Grunvald MW, Underhill JM, Skertich NJ, et al. Mediating factors between race and time to treatment in colorectal cancer. Dis Colon Rectum. 2021.
Lee L, Wong-Chong N, Kelly JJ, Nassif GJ, Albert MR, Monson JRT. Minimally invasive surgery for stage III colon adenocarcinoma is associated with less delay to initiation of adjuvant systemic therapy and improved survival. Surg Endosc. 2019;33(2):460–70.
Lee MG, Chiu CC, Wang CC, et al. Trends and outcomes of surgical treatment for colorectal cancer between 2004 and 2012- an analysis using national inpatient database. Sci Rep. 2017;7(1):2006.
Alnasser M, Schneider EB, Gearhart SL, et al. National disparities in laparoscopic colorectal procedures for colon cancer. Surg Endosc. 2014;28(1):49–57.
Cairns AL, Schlottmann F, Strassle PD, Di Corpo M, Patti MG. Racial and socioeconomic disparities in the surgical management and outcomes of patients with colorectal carcinoma. World J Surg. 2019;43(5):1342–50.
Economic, Research, Service. USDA ERS - Rural classifications. https://www.ers.usda.gov/topics/rural-economy-population/rural-classifications/. Accessed April 11, 2023.
von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–9.
Turner M, Adam MA, Sun Z, et al. Insurance status, not race, is associated with use of minimally invasive surgical approach for rectal cancer. Ann Surg. 2017;265(4):774–81.
Guller U, Jain N, Curtis LH, Oertli D, Heberer M, Pietrobon R. Insurance status and race represent independent predictors of undergoing laparoscopic surgery for appendicitis: secondary data analysis of 145,546 patients. J Am Coll Surg. 2004;199(4):567–75. https://doi.org/10.1016/j.jamcollsurg.2004.06.023.
Pieracci FM, Eachempati SR, Christos PJ, Barie PS, Mushlin AI. Explaining insurance-related and racial disparities in the surgical management of patients with acute appendicitis. Am J Surg. 2007;194(1):57–62.
Lassiter RL, Talukder A, Abrams MM, Adam BL, Albo D, White CQ. Racial disparities in the use of laparoscopic surgery to treat colonic diverticulitis Are not fully explained by socioeconomics or disease complexity. Am J Surg. 2017;213(4):673–7.
Simon HL, Reif de Paula T, Spigel ZA, Keller DS. National disparities in use of minimally invasive surgery for rectal cancer in older adults. J Am Geriatr Soc. 2022;70(1):126–35.
Gabriel E, Thirunavukarasu P, Al-Sukhni E, Attwood K, Nurkin SJ. National disparities in minimally invasive surgery for rectal cancer. Surg Endosc. 2016;30(3):1060–7.
Lo BD, Zhang GQ, Stem M, et al. Do specific operative approaches and insurance status impact timely access to colorectal cancer care? Surg Endosc. 2021;35(7):3774–86.
Patel R, Pant K, Patel KS, Merchant AM, Alvarez-Downing MM. Association of hospital factors and socioeconomic status with the utilization of minimally invasive surgery for colorectal cancer over a decade. Surg Endosc. 2022;36(6):3750–62.
Horsey ML, Lai D, Sparks AD, Herur-Raman A, Borum M, Rao S, Ng M, Obias VJ. Disparities in utilization of robotic surgery for colon cancer: an evaluation of the U.S. national cancer database. J Robotic Surg. 2022;16(6):1299–306. https://doi.org/10.1007/s11701-022-01371-3.
Acknowledgement
Services and products in support of the research project were generated by the VCU Massey Cancer Center Biostatistics Shared Resource, supported in part with funding from NIH-NCI Cancer Center Support Grant P30 CA016059. Authors are supported by the National Human Genome Research Institute (T32 HG008958 to ANR, KMH) and National Cancer Institute (R01 CA242003 to JGT, U54 CA233444 to JGT, U54 CA233444-03S1 to ANR, and JGT) of the National Institutes of Health and the Joseph and Ann Matella Fund for Pancreatic Cancer Research (JGT).
Funding
This study was not sponsored.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Riner, A.N., Herremans, K.M., Deng, X. et al. Racial/Ethnic Disparities in the Era of Minimally Invasive Surgery for Treatment of Colorectal Cancer. Ann Surg Oncol 30, 6748–6759 (2023). https://doi.org/10.1245/s10434-023-13693-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-13693-z