Abstract
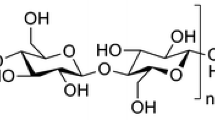
This study reports the formulation of mupirocin-loaded chitosan microspheres embedded in Piper betle extract containing collagen scaffold as combinational drug delivery for improved wound healing. Selection of chitosan type (molecular weight and degree of deacetylation) was carried out based on their antibacterial efficacy. The low molecular weight chitosan was selected owing to the highest antibacterial action against gram-positive as well as gram-negative bacteria. Low molecular weight chitosan-microspheres showed spherical shape with largely smooth surface morphology, 11.81% of mupirocin loading, and its controlled release profile. The XRD, DSC thermograms, and FT-IR spectral analysis revealed the mupirocin loaded in molecularly dispersed or in amorphous form, and having no chemical interactions with the chitosan matrix, respectively. The in vivo study indicates potential effect of the mupirocin, Piper betle, and chitosan in the collagen scaffold in the wound healing efficiency with approximately 90% wound healing observed at the end of 15 days of study for combinational drug-loaded chitosan microspheres-collagen scaffold-treated group. The histopathology examination further revealed tissue lined by stratified squamous epithelium, collagen deposition, fibroblastic proliferation, and absence of inflammation indicating relatively efficient wound healing once treated with combinational drug-loaded chitosan microspheres containing scaffold.










Similar content being viewed by others
References
Lo ZJ, Lim X, Eng D, Car J, Hong Q, Yong E, Zhang L, Chandrasekar S, Tan GW, Chan YM. Clinical and economic burden of wound care in the tropics: a 5-year institutional population health review. Int Wound J. 2020;17:790–803.
Rodrigues M, Kosaric N, Bonham CA, Gurtner GC. Wound healing: a cellular perspective. Physiol Rev. 2019;99:665–706. https://doi.org/10.1152/physrev.00067.2017.
Kim HS, Sun X, Lee J-H, Kim H-W, Fu X, Leong KW. Advanced drug delivery systems and artificial skin grafts for skin wound healing. Adv Drug Deliv Rev. 2019;146:209–39.
Hasan N, Cao J, Lee J, Hlaing SP, Oshi MA, Naeem M, Ki M-H, Lee BL, Jung Y, Yoo J-W. Bacteria-targeted clindamycin loaded polymeric nanoparticles: effect of surface charge on nanoparticle adhesion to MRSA, antibacterial activity, and wound healing. Pharmaceutics. 2019;11:236. https://doi.org/10.3390/pharmaceutics11050236.
Okur NÜ, Hökenek N, Okur ME, Ayla Ş, Yoltaş A, Siafaka PI, Cevher E. An alternative approach to wound healing field; new composite films from natural polymers for mupirocin dermal delivery. Saudi Pharm J. 2019;27:738–52.
Golmohammadi R, Najar-Peerayeh S, Tohidi Moghadam T, Hosseini SMJ. Synergistic antibacterial activity and wound healing properties of selenium-chitosan-mupirocin nanohybrid system: an in vivo study on rat diabetic Staphylococcus aureus wound infection model. Sci Rep. 2020;10:2854. https://doi.org/10.1038/s41598-020-59510-5.
Goldmann O, Cern A, Müsken M, Rohde M, Weiss W, Barenholz Y, Medina E. Liposomal mupirocin holds promise for systemic treatment of invasive Staphylococcus aureus infections. J Control Release. 2019;316:292–301. https://doi.org/10.1016/j.jconrel.2019.11.007.
Amrutiya N, Bajaj A, Madan M. Development of microsponges for topical delivery of mupirocin. AAPS PharmSciTech. 2009;10:402–9. https://doi.org/10.1208/s12249-009-9220-7.
Yasasvini S, Anusa R, VedhaHari B, Prabhu P, RamyaDevi D. Topical hydrogel matrix loaded with Simvastatin microparticles for enhanced wound healing activity. Mater Sci Eng C. 2017;72:160–7. https://doi.org/10.1016/j.msec.2016.11.038.
Lengyel M, Kállai-Szabó N, Antal V, Laki AJ, Antal I. Microparticles, microspheres, and microcapsules for advanced drug delivery. Sci Pharm. 2019;87:20. https://doi.org/10.3390/scipharm87030020.
Midha K, Nagpal M, Arora S. Microspheres: a recent update. Int J Recent Sci Res. 2015;8:5859–67.
Berthold A, Cremer K, Kreuter J. Preparation and characterization of chitosan microspheres as drug carrier for prednisolone sodium phosphate as model for anti-inflammatory drugs. J Control Release. 1996;39:17–25. https://doi.org/10.1016/0168-3659(95)00129-8.
Lv B, Wang Y, Chen W. Preparation, Characterization, and bioactivity of chitosan microspheres containing basic fibroblast growth factor. J Nanomater. 2014;2014:1–7. https://doi.org/10.1155/2014/534287.
Shanmuganathan S, Shanumugasundaram N, Adhirajan N, Lakshmi TR, Babu M. Preparation and characterization of chitosan microspheres for doxycycline delivery. Carbohydr Polym. 2008;73:201–11.
Sinha VR, Singla AK, Wadhawan S, Kaushik R, Kumria R, Bansal K, Dhawan S. Chitosan microspheres as a potential carrier for drugs. Int J Pharm. 2004;274:1–33. https://doi.org/10.1016/j.ijpharm.2003.12.026.
Varshosaz J. The promise of chitosan microspheres in drug delivery systems. Expert Opin Drug Deliv. 2007;4:263–73.
Perinelli DR, Fagioli L, Campana R, Lam JK, Baffone W, Palmieri GF, Casettari L, Bonacucina G. Chitosan-based nanosystems and their exploited antimicrobial activity. Eur J Pharm Sci. 2018;117:8–20.
Zheng L-Y, Zhu J-F. Study on antimicrobial activity of chitosan with different molecular weights. Carbohydr Polym. 2003;54:527–30.
Zhu Q, Teng J, Liu X, Lan Y, Guo R. Preparation and characterization of gentamycin sulfate-impregnated gelatin microspheres/collagen–cellulose/nanocrystal scaffolds. Polym Bull. 2018;75:77–91.
Mahmoud AA, Salama AH. Norfloxacin-loaded collagen/chitosan scaffolds for skin reconstruction: preparation, evaluation and in-vivo wound healing assessment. Eur J Pharm Sci. 2016;83:155–65. https://doi.org/10.1016/j.ejps.2015.12.026.
Lee JE, Kim KE, Kwon IC, Ahn HJ, Lee S-H, Cho H, Kim HJ, Seong SC, Lee MC. Effects of the controlled-released TGF-β1 from chitosan microspheres on chondrocytes cultured in a collagen/chitosan/glycosaminoglycan scaffold. Biomaterials. 2004;25:4163–73.
Denkbaş EB, Öztürk E, N. Özdem&unknown;r, K. Keçec&unknown;, C. Agalar, Norfloxacin-loaded chitosan sponges as wound dressing material, J Biomater Appl 18 (2004) 291–303. https://doi.org/10.1177/0885328204041510
Keat EC, Razak SS, Fadil NM, Yusof FM, Chan LH, Chyi FK, Teoh SL, Das S, Latiff AA, Mazlan M. The effect of Piper betel extract on the wound healing process in experimentally induced diabetic rats. Clin Ter. 2010;161:117–20.
Lien LT, Tho NT, Ha DM, Hang PL, Nghia PT, Thang ND. Influence of phytochemicals in Piper betle linn leaf extract on wound healing. Burns Trauma. 2015;3:s41038–015-0023–7. https://doi.org/10.1186/s41038-015-0023-7.
Ghazali NA, Elmy A, Yuen LC, Sani NZ, Das S, Suhaimi F, Yusof R, Yusoff NH, Thent ZC. Piper betel leaves induces wound healing activity via proliferation of fibroblasts and reducing 11β hydroxysteriod dehydrogenase-1 expression in diabetic rat. J Ayurveda Integr Med. 2016;7:198–208. https://doi.org/10.1016/j.jaim.2016.08.008.
Balouiri M, Sadiki M, Ibnsouda SK. Methods for in vitro evaluating antimicrobial activity: a review. J Pharm Anal. 2016;6:71–9.
Ko JA, Park HJ, Hwang SJ, Park JB, Lee JS. Preparation and characterization of chitosan microparticles intended for controlled drug delivery. Int J Pharm. 2002;249:165–74. https://doi.org/10.1016/S0378-5173(02)00487-8.
Ali A, Lim XY, Chong CH, Mah SH, Chua BL. Optimization of ultrasound-assisted extraction of natural antioxidants from Piper betle using response surface methodology. LWT. 2018;89:681–8. https://doi.org/10.1016/j.lwt.2017.11.033.
Perumal S, Ramadass SK, Madhan B. Sol–gel processed mupirocin silica microspheres loaded collagen scaffold: a synergistic bio-composite for wound healing. Eur J Pharm Sci. 2014;52:26–33. https://doi.org/10.1016/j.ejps.2013.10.006.
Karri VVSR, Kuppusamy G, Talluri SV, Mannemala SS, Kollipara R, Wadhwani AD, Mulukutla S, Raju KRS, Malayandi R. Curcumin-loaded chitosan nanoparticles impregnated into collagen-alginate scaffolds for diabetic wound healing. Int J Biol Macromol. 2016;93:1519–29. https://doi.org/10.1016/j.ijbiomac.2016.05.038.
Anal AK, Stevens WF, Remuñán-López C. Ionotropic cross-linked chitosan microspheres for controlled release of ampicillin. Int J Pharm. 2006;312:166–73. https://doi.org/10.1016/j.ijpharm.2006.01.043.
Kim S. Competitive biological activities of chitosan and its derivatives: antimicrobial, antioxidant, anticancer, and anti-inflammatory activities. Int J Polym Sci. 2018;2018:1–13. https://doi.org/10.1155/2018/1708172.
Fei Liu X, Lin Guan Y, Zhi Yang D, Li Z, De Yao K. Antibacterial action of chitosan and carboxymethylated chitosan. J Appl Polym Sci. 2001;79:1324–35.
Chung Y-C, Chen C-Y. Antibacterial characteristics and activity of acid-soluble chitosan. Bioresour Technol. 2008;99:2806–14. https://doi.org/10.1016/j.biortech.2007.06.044.
Chifiriuc CM, Grumezescu AM, Saviuc C, Croitoru C, Mihaiescu DE, Lazar V. Improved antibacterial activity of cephalosporins loaded in magnetic chitosan microspheres. Int J Pharm. 2012;436:201–5. https://doi.org/10.1016/j.ijpharm.2012.06.031.
Desai KGH, Park HJ, Encapsulation of vitamin C in tripolyphosphate cross-linked chitosan microspheres by spray drying, 2004
Duraipandy N, Lakra R, Vinjimur Srivatsan K, Ramamoorthy U, Korrapati PS, Kiran MS. Plumbagin caged silver nanoparticle stabilized collagen scaffold for wound dressing. J Mater Chem B. 2015;3:1415–25. https://doi.org/10.1039/C4TB01791A.
Jones V, Grey JE, Harding KG. Wound dressings. BMJ. 2006;332:777–80.
Hussain MR, Devi RR, Maji TK. Controlled release of urea from chitosan microspheres prepared by emulsification and cross-linking method. Iran Polym J. 2012;21:473–9.
Kulkarni PV, Keshavayya J, Kulkarni VH. Effect of method of preparation and process variables on controlled release of insoluble drug from chitosan microspheres. Polym Adv Technol. 2007;18:814–21. https://doi.org/10.1002/pat.940.
Ochiuz L, Popa G, Stoleriu I, Tomoiagă AM, Popa M. Microencapsulation of metoprolol tartrate into chitosan for improved oral administration and patient compliance. Ind Eng Chem Res. 2013;52:17432–41. https://doi.org/10.1021/ie402625h.
Dai T, Tanaka M, Huang Y-Y, Hamblin MR. Chitosan preparations for wounds and burns: antimicrobial and wound-healing effects. Expert Rev Anti-Infect Ther. 2011;9:857–79. https://doi.org/10.1586/eri.11.59.
Funding
The support for this study is provided by Taif University Researchers Supporting Project Number (TURSP-2020/33), Taif University, Saudi Arabia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Budhiraja, M., Zafar, S., Akhter, S. et al. Mupirocin-Loaded Chitosan Microspheres Embedded in Piper betle Extract Containing Collagen Scaffold Accelerate Wound Healing Activity. AAPS PharmSciTech 23, 77 (2022). https://doi.org/10.1208/s12249-022-02233-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-022-02233-9