Abstract
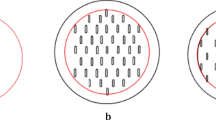
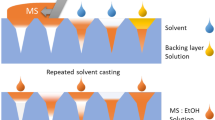
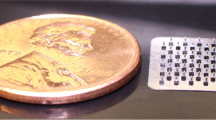
Suspension-based matrix transdermal delivery systems (TDSs) are specialized systems that maintain a continuous driving force for drug delivery over prolonged wear. The pressure-sensitive adhesive (PSA) is the most critical constituent of such systems. Our study aimed to determine the effect of different mixing methods on the performance of silicone PSA-based suspension TDSs. Lidocaine suspension TDSs were prepared using conventional slow rotary mixing, high-speed homogenization, bead-mill homogenization, vortex shaking, and by an unguator. Resultant TDSs were tested for tack, shear, and peel properties and correlated to coat weight, content uniformity, microstructure, and in vitro permeation across dermatomed human skin. Every mixing method tested caused a significant reduction in peel. However, bead-mill homogenization resulted in significant loss of all adhesive properties tested, while unguator-mixed TDSs retained most properties. Good linear correlation (R2 = 1.000) between the shear properties of the TDSs with the average cumulative amount of lidocaine permeated after 24 h was observed, with no significant difference between percutaneous delivery from slow rotary-mixed systems (1334 ± 59.21 μg/cm2) and unguator-mixed systems (1147 ± 108.3 μg/cm2). However, significantly lower delivery from bead-mill homogenized systems (821.1 ± 28.00 μg/cm2) was noted. While many factors affect TDS performance, careful consideration must also be given to the processing parameters during development as they have been shown to affect the resultant system’s therapeutic efficacy. Extensive mixing with bead-mill homogenization demonstrated crystallization of drug, loss in adhesive properties, coat weight, and film thickness, with reduced transdermal delivery of lidocaine from the prepared system.







Similar content being viewed by others
References
Wiedersberg S, Guy RH. Transdermal drug delivery: 30+ years of war and still fighting! J Control Release. 2014;190:150–6.
Prausnitz MR, Mitragotri S, Langer R. Current status and future potential of transdermal drug delivery. Nat Rev Drug Discov. 2004;3(2):115–24.
Parivesh S, Sumeet D, Abhishek D. Design, Evaluation, Parameters and Marketed Products of transdermal patches: A Review. J Pharm Res. 2010;3(2):235–40.
Tan HS, Pfister WR. Pressure-sensitive adhesives for transdermal drug delivery systems. Pharm Sci Technolo Today. 1999;2(2):60–9.
U.S. Food & Drug Administration. Transdermal and topical delivery systems - product development and quality considerations guidance for industry (Draft Guidance). 2019.
Deepthi V, Khan AB. Role of adhesives in transdermal drug delivery: a review. Int J Pharm Sci Res. 2012;3(10):3559–64.
Kandavilli S, Nair V, Panchagnula R. Polymers in transdermal drug delivery systems. Pharm Technol. 2002;(May):62–80.
Lobo S, Sachdeva S, Goswami T. Role of pressure-sensitive adhesives in transdermal drug delivery systems. Ther Deliv. 2016;7(1):33–48.
Kokubo T, Sugibayashi K, Morimoto Y. Interaction between drugs and pressure-sensitive adhesives in transdermal therapeutic systems. Pharm Res. 1994;11(1):104–7.
Takemasa K, Kenji S, Yasunori M. Diffusion of drug in acrylic-type pressure-sensitive adhesive matrices. I. Influence of physical property of the matrices on the drug diffusion. J Control Release. 1991;17(1):69–77.
Kim J-H, Cho Y-J, Choi H-K. Effect of vehicles and pressure sensitive adhesives on the permeation of tacrine across hairless mouse skin. Int J Pharm. 2000;196(1):105–13.
Couto A, Fernandes R, Cordeiro MNS, Reis SS, Ribeiro RT, Pessoa AM. Dermic diffusion and stratum corneum: a state of the art review of mathematical models. J Control Release. 2014;177(1):74–83.
Benson H. Transdermal Drug Delivery: Penetration Enhancement Techniques. Curr Drug Deliv. 2005;2(1):23–33.
Higuchi T. Physical chemical analysis of percutaneous absorption process from creams and ointments. J Soc Cosmet Chem. 1960;11:85–97.
Ravula R, Herwadkar AK, Abla MJ, Little J, Banga AK. Formulation optimization of a drug in adhesive transdermal analgesic patch. Drug Dev Ind Pharm. 2016;42(6):862–70.
Hadgraft J. Passive enhancement strategies in topical and transdermal drug delivery. Int J Pharm. 1999;184(1):1–6.
Pastore MN, Kalia YN, Horstmann M, Roberts MS. Transdermal patches: history, development and pharmacology. Br J Pharmacol. 2015;172(9):2179–209.
Miller KJ II, Govil SK, Bhatia KS. Fentanyl suspension-based silicone adhesive formulations and devices for transdermal delivery of fentanyl. United States. 2004;7:556,823.
Allen L, Ansel HC. Ansel’s pharmaceutical dosage forms and drug delivery systems. Lippincott Williams & Wilkins; 2013.
European Medicines Agency. Draft guideline on quality and equivalence of topical products. 2018;Vol. 44, Ema/Chmp/Qwp/708282/2018.
U.S. Food and Drug Administration. Assessing adhesion with transdermal delivery systems and topical patches for ANDAs draft guidance for industry. 2018.
Strasinger C, Raney SG, Tran DC, Ghosh P, Newman B, Bashaw ED, et al. Navigating sticky areas in transdermal product development. J Control Release. 2016;233:1–9.
Puri A, Bhattaccharjee SA, Zhang W, Clark M, Singh ON, Doncel GF, et al. Development of a transdermal delivery system for tenofovir alafenamide, a prodrug of tenofovir with potent antiviral activity against HIV and HBV. Pharmaceutics. 2019;11(4):173.
Dasht Bozorg B, Banga AK. Effect of Different Pressure-Sensitive Adhesives on Performance Parameters of Matrix-Type Transdermal Delivery Systems. Pharmaceutics. 2020;12(3):209.
Bhattaccharjee S, Beck-Broichsitter M, Banga AK. In Situ Gel Formation in Microporated Skin for Enhanced Topical Delivery of Niacinamide. Pharmaceutics. 2020;12(5):472.
Bhattaccharjee SA, Murnane KS, Banga AK. Transdermal delivery of breakthrough therapeutics for the management of treatment-resistant and post-partum depression. Int J Pharm. 2020;120007.
Dasht BozorgB Transdermal and Dermatological Formulations for delivery of Pharma- and Cosmeceutical Actives into Healthy and Diseased Skin. Mercer University; 2020.
PubChem. Lidocaine | C14H22N2O - PubChem [Internet]. 2020 [cited 2020 Oct 10]. Available from: https://pubchem.ncbi.nlm.nih.gov/compound/Lidocaine#section=Melting-Point.
Oktay AN, Ilbasmis-Tamer S, Celebi N. The effect of critical process parameters of the high pressure homogenization technique on the critical quality attributes of flurbiprofen nanosuspensions. Pharm Dev Technol. 2019;24(10):1278–86.
OMNI International. Bead Ruptor Elite [Internet]. 2020 [cited 2020 Oct 10]. Available from: https://www.omni-inc.com/omni-bead-ruptor-elite-bead-mill-homogenizer.html.
Sugimoto M, Kondo M, Horiguchi M. Uniform suspension of the clustered triamcinolone acetonide particle. J Ophthalmol. 2013;2013.
Ma X, Taw J, Chiang CM. Control of drug crystallization in transdermal matrix system. Int J Pharm. 1996;142(1):115–9.
Jain P, Banga AK. Induction and inhibition of crystallization in drug-in-adhesive-type transdermal patches. Pharm Res. 2013;30(2):562–71.
Jain P, Banga AK. Inhibition of crystallization in drug-in-adhesive-type transdermal patches. Int J Pharm. 2010;394(1–2):68–74.
Wolff HM. Irsan, Dodou K. Investigations on the viscoelastic performance of pressure sensitive adhesives in drug-in-adhesive type transdermal films. Pharm Res. 2014;31(8):2186–202.
Minghetti P, Cilurzo F, Casiraghi A. Measuring adhesive performance in transdermal delivery systems. Am J Drug Deliv. 2004;2(3):193–206.
Agile Therapeutics Inc. Weekly Birth Control Patch | Twirla ® [Internet]. 2020 [cited 2020 Oct 10]. Available from: https://twirla.com/.
Author information
Authors and Affiliations
Contributions
Sonalika Arup Bhattaccharjee—conceptualization, data curation, formal analysis, investigation, methodology, writing (original draft preparation, review and editing), and visualization. Madhura Kale—investigation. Ngan Le—investigation. Ajay K. Banga—conceptualization, resources, supervision, and writing (review and editing).
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bhattaccharjee, S.A., Kale, M., Le, N. et al. Impact of Different Mixing Methods on the Performance of Suspension-Based Transdermal Delivery Systems. AAPS PharmSciTech 22, 150 (2021). https://doi.org/10.1208/s12249-021-02022-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-021-02022-w