Abstract
Bronchopulmonary dysplasia (BPD) is a common adverse outcome of prematurity, causing severe morbidity and mortality. The cytokine macrophage migration inhibitory factor (MIF) has been recently shown to favor murine fetal lung development. In this prospective study, we evaluate the expression of MIF in the lung and in the serum of preterm infants (n = 50) and investigate whether the −173 G/C MIF promoter polymorphism is associated with the risk of BPD (n = 103). MIF was highly expressed in lung tissue from preterm infants. Serum MIF levels were measured by ELISA at d 1 after birth. MIF levels were increased [median (interquartile range), 71.01 (44.9–162.3) ng/mL], particularly in those infants with RDS [110.4 (59.4–239.2) ng/mL] compared with healthy adults [2.4 (1.2–5.0) ng/mL], (p < 0.001). The MIF −173*C allele, which predisposes to higher MIF production, was associated with a lower incidence of BPD (OR, 0.2; 95% CI, 0.04–0.93), independently from mechanical ventilation and oxygen exposure (p = 0.03). In conclusion, these data show that MIF expression is increased in lung and serum of preterm infants and suggest that the high producing MIF −173*C allele may be a protective factor for BPD.
Similar content being viewed by others
Main
RDS and bronchopulmonary dysplasia (BPD) are major causes of morbidity and mortality in preterm neonates. RDS is an acute condition that appears in the first hours of life and is caused by the lack of pulmonary surfactant, with progressive atelectasis and respiratory insufficiency. BPD is a chronic condition, which appears later in life and is characterized by an initial inflammatory component, followed by alveolar edema and fibrosis, resulting in impaired development of the immature lung (1,2). Prematurity, RDS, mechanical ventilation, lung disruption, and oxygen (O2) toxicity play a major role in BPD pathogenesis (3). The contribution of inflammation remains controversial (4). Chorioamnionitis and cytokine exposure in utero seem to protect from RDS, suggesting that inflammatory mediators and cytokines may promote lung maturation (5,6). Conversely, there is evidence that a postnatal exaggerated and/or prolonged inflammatory response may amplify lung damage, resulting in tissue autoinjury, structural changes, and ultimately BPD (7). In addition to environmental factors, heritability studies demonstrated that genetic factors also contribute to the susceptibility to BPD (8), and potential candidate genes have been identified (9–15).
Macrophage migration inhibitory factor (MIF) is a proinflammatory cytokine, which plays a critical role in immune and inflammatory responses. MIF induces macrophage production of cytokines and promotes T lymphocytes proliferation (16). It has been implicated in the pathogenesis of immune and inflammatory diseases, including sepsis, asthma, allergic neuritis, and rheumatoid arthritis (17,18). MIF has also been reported to be involved in angiogenesis (19,20). In lungs, MIF is expressed in alveolar macrophages, bronchial epithelial cells, and alveolar endothelium (21,22).
Animal data suggest a role for MIF in lung maturation. MIF-deficient mice delivered prematurely suffer more respiratory distress and show higher mortality than WT mice (23). In MIF-deficient mice, genes involved in lung maturation, including VEGF and surfactant proteins, are down-regulated. In vitro, MIF has been shown to increase VEGF and surfactant protein B mRNA expression in the human alveolar type II cell line H441 and to induce proliferation of alveolar epithelial type II cells (24). Interestingly, recent studies have also shown that MIF is an hypoxia-responsive gene (25,26). All together, these observations suggest that in preterm infants MIF plays a positive role in lung maturation, possibly acting as a protective factor for BPD.
The MIF promoter contains a functionally relevant single nucleotide polymorphism (SNP) G→C at position −173. This polymorphism has been shown to be functionally relevant in vitro, with the C allele associated with higher expression in a T lymphoblastoid cell line, whereas, in contrast, in A549 cells (human lung carcinoma cells), the G polymorphism was associated with higher MIF levels (27). In vivo data in humans showed that the carriage of the C allele was associated with increased serum levels in healthy controls and increased synovial fluid levels in patients with Juvenile idiopathic arthritis (27–29).
In this study, we evaluated the expression of MIF in lungs and measured circulating MIF levels in a cohort of preterm neonates with and without RDS. Moreover, to test the hypothesis that genetic predisposition to higher MIF expression may decrease the probability to develop BPD, we also investigated whether the MIF −173 SNP was associated with BPD.
METHODS
Patients.
Two groups of preterm neonates (GA ≥24 and ≤34 wk), in whom the presence of infections in the first 48 h (vertical infections) was excluded, were included in the study:
Group 1.
Fifty infants, in whom a serum sample at d 1 of life was available for MIF measurement, were studied for the association of MIF blood levels with RDS. The clinical characteristics of the infants of the group 1 of infants are shown in Table 1.
Group 2.
Hundred and three infants with a diagnosis of RDS, consecutively admitted to our NICU, in whom complete clinical data on respiratory outcomes was obtained and genomic DNA was available, were studied for the association of the MIF genotype with BPD. Infants with congenital cardiac disease, gastroschisis, or diaphragmatic hernia were excluded. Diagnosis of RDS was based on the reported classical clinical signs (grunting, retraction, flaring, need for supplementary O2 for 48 h, or need for exogenous surfactant therapy) associated with the typical radiological findings (diffuse reticulogranular pattern and air bronchograms). The following data were collected: demographic and clinical characteristics on admission to the NICU, gender, birth weight, GA, antenatal steroids therapy, days on mechanical ventilation, days on O2 supplementation, maximal inspired O2 concentration, and presence of patent ductus arteriosus. BPD was defined as the requirement of O2 supplementation beyond 36 wk of postconceptional age (PCA) and abnormal radiologic findings. Among infants observed, 12 infants died before 36 wk PCA. The main characteristics of the group 2 of infants are shown in Table 2. The study was approved by the Institutional Review Board of the Ospedale Pediatrico Bambino Gesù, and informed consent was obtained from the parents.
Measurement of serum MIF levels.
Serum MIF levels were measured by ELISA with a MAb to MIF for coating (R&D Systems, Minneapolis, MN) and a biotinylated antibody to MIF for detection (R&D Systems) as described (29,30).
MIF immunohistochemistry.
Immunohistochemical analysis was performed on autoptic specimens of lung tissue from two neonates (GA 26 and 27 wk), who died in the first day of life, and from one asphyxiated fresh still birth neonate (GA 28 wk). Autoptic specimens of healthy lung tissue from a 10-y-old child were used as control. Lung tissue was fixed in neutral buffered formalin and embedded in paraffin. After moist heat-induced antigen retrieval with 1 mm EDTA at pH 9.0, 3 μm sections were incubated with a mouse MAb to human MIF (R&D Systems) for 1 h at room temperature or with an irrelevant mouse IgG1. After washing, the presence of MIF was revealed with the Labeled Streptavidin-Biotin2 System (DakoCytomation, Inc., Carpinteria, CA), based on the use of a biotinylated secondary antibody and peroxidase-conjugated streptavidin. The procedure was performed according to the instructions provided by the manufacturer. The 3-3′diaminobenzidine was used as a chromogen, and counterstaining was with hematoxylin (DakoCytomation, Inc.).
MIF −173 G/C genotyping.
Genomic DNA from blood was obtained using QIAmp DNA Mini Kits (Quiagen), according to the manufacturer's specifications. A 365-bp fragment of MIF promoter was amplified using specific primers (forward: ACTAAGAAAGACCCGAGC; reverse GGGGCACGTTGGTGTTTAC; E1) and analyzed by denaturing HPLC (DHPLC) analysis (Transgenomic, San Jose, CA), using the software WaveMaker 2.0, and by enzymatic digestion with AluI (New England Biolabs), as described (31).
Statistical analysis.
Statistical analyses were performed using the Statistical Package for Social Science (SPSS) and STATA (STATAcorp). Statistical significance was set at p < 0.05. Quantitative data were expressed as median and interquartile range (IQR). As the number of patients carrying the CC genotype was low, as expected (27), for genetic analysis, patients were classified in two groups: those carrying at least one MIF −173*C allele and those carrying the GG genotype. The main outcome of the analysis was the development of BPD. The relative contribution of each variable to the risk of developing BPD was expressed as the OR with 95% CIs. A multivariate logistic regression analysis was also performed including MIF genotypes and clinical and procedural variables significantly associated with BPD at univariate analysis. Probabilities of developing BPD, according to different combinations of covariates, were estimated on the basis of the minimal logistic model.
RESULTS
MIF lung expression and serum levels in preterm infants at d 1 after birth.
Immunohistochemical analysis on lung tissues from one asphyxiated fresh still born infant (Fig. 1A and B) and from two preterm infants, deceased in the first day of life (Fig. 1C and D), showed staining for MIF in alveolar macrophages, bronchial epithelial cells, and alveolar endothelial cells. Negligible staining was observed in the normal lung tissue from a 10-y-old child (Fig. 1E and F). Serum levels of MIF were measured in a group of preterm infants (group 1, n = 50) at d 1 after birth. Circulating MIF levels at d 1 after birth (median, 71.01 ng/mL; IQR, 44.9–162.3) were markedly higher (p < 0.001) compared with levels in adults (median, 2.4 ng/mL; IQR, 1.2–5.0; Fig. 1G). No significant differences were found when preterm neonates were divided according to the mode of delivery (cesarean: median, 72.47 ng/mL; IQR, 49.31–175.85; vaginal: median, 57.92; IQR, 34.69–134.16) or by antenatal steroid exposure (yes: median, 75.8 ng/mL; IQR, 43.4–196.1; no: median, 73.9; IQR, 52.0–79.7). No correlation was found with GA (r2 = 0.09, not shown). When patients were divided according to the presence or absence of RDS at admission, we found that serum MIF levels at d 1 after birth were significantly higher (p = 0.004) in infants with RDS (median, 110.4 ng/mL; IQR, 59.4–239.2) compared with those without RDS (median, 51.7 ng/mL; IQR, 37.0–73.9; Fig. 1H).
MIF expression in preterm neonates. Increased MIF immunohistochemical staining in lung tissue from one asphyxiated fresh still born neonate (A and B) and from one of two preterm neonates deceased on d 1 after birth (C and D) compared with normal lung tissue from a 10-y-old child (perilesional tissue obtained during lung surgery; E and F). Staining is found in macrophages, bronchial epithelial cells, and alveolar endothelial cells. Scale bar = 60 μm in (A, C, E) and 220 μm in (B, D, F). Increased circulating MIF levels in preterm neonates at d 1 after birth: comparison with healthy adults (n = 54), *p < 0.001 (G) and preterm neonates with or without RDS (n = 50), **p = 0.004 (H). The limits of the boxes represent the 25 and 75 percentile values, the horizontal lines across the boxes are the median values, and the upper and lower limits of the vertical lines depict the maximum and minimum values, respectively. The p value was calculated using the Mann-Whitney U test.
Carriage of the MIF −173*C allele is a protective factor for the development of BPD.
Animal data suggest a role for MIF in lung maturation. In MIF-deficient mice delivered prematurely, genes involved in lung maturation, including VEGF and surfactant proteins, are down-regulated (23). Based on these data, it is possible to speculate that increased MIF expression in preterm neonates, particularly in those with RDS, may be part of a positive mechanism activated by hypoxia to promote lung maturation. As previously mentioned, the MIF promoter −173*C allele is associated with higher MIF expression in vitro and in vivo in humans (27–29). Therefore, we evaluated whether the MIF −173 G/C polymorphism was associated with development of BPD in 103 preterm infants with a diagnosis of RDS on admission (group 2): 12 of them died before 36 wk of PCA and 25 of them developed BPD (Table 2). The genotype distribution and allele frequency in the group of preterm neonates enrolled in our study did not show significant deviation from the Hardy-Weinberg equilibrium or significant difference from adult controls (Table 3).Moreover, in this study, the frequency of the C allele in non-Caucasian infants (South American and North African) is the same (4/18, 22.2%) as that in white Caucasian (19/85, 22.4%). The MIF −173 genotype distribution and alleles frequencies differed significantly between neonates with or without BPD (Table 3). The frequency of carriers of the high producing −173*C allele was significantly lower in neonates who developed BPD (2 of 25; 8.0%) compared with that of neonates who did not develop BPD (20 of 66; 30.3%; p = 0.04; Table 3). This difference remained significant when the composite outcome of BPD or death before 36 wk of PCA was considered (8.1 versus 30.3%; p = 0.04).
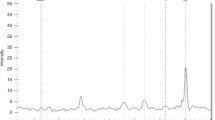
In univariate analysis, carriage of the high producing MIF −173*C allele conferred significant protection from the development of BPD (OR, 0.20; 95% CI, 0.04–0.93) and, conversely, carriage of the MIF −173 G/G genotype was associated with higher risk of BPD (OR, 5.0; 95% CI, 1.07–23.2). Similarly, when the outcome BPD or death before 36 wk PCA was considered, the high producing MIF −173*C allele was significantly associated with a lower risk (OR, 0.20; 95% CI, 0.05–0.74). When known risk factors for BPD were analyzed by univariate analysis, we found that, as expected, development of BPD was associated with gender, GA, infections, maximal inspired O2 concentration, days on mechanical ventilation, and days on O2 supplementation (Table 4). When these variables were included in a multivariate logistic regression analysis, the minimal model included the MIF −173 C/G and C/C genotypes, the days on O2 therapy, and the maximal inspired O2 concentration (r2 = 0.66; Table 5). Similarly, when we considered the outcome BPD or death before 36 wk PCA, the minimal model included the same variables and the GA variable (Table 5). Incidentally, the independent contribution of days on mechanical ventilation and days on O2 supplementation could not be analyzed because of the collinearity of the two variables. Using the variables included in the model shown in Table 5, we obtained probability curves for development of BPD as a function of days on O2 therapy and of maximal FiO2 >0.60 or <0.60 (Fig. 2). The probability of developing BPD as a function of the number of days on O2 therapy was markedly lower in preterm neonates carrying the MIF −173*C allele compared with the carriers of the high-risk MIF −173 G/G genotype. All together these results show that carriage of the MIF −173*C allele is significantly associated with a lower risk of BPD in preterm neonates independently from O2 therapy.
Probability curves for the development of BPD as a function of the number of days on O2 therapy and of maximal O2 inspired concentration >0.60 or <0.60 in neonates carrying the MIF −173*C allele compared with the carriers of the high-risk MIF −173 G/G genotype. —, Maximum O2 inspired concentration >0.60 and MIF −173 G/G;  , maximum O2 inspired concentration >0.60 and MIF −173 G/C or C/C;
, maximum O2 inspired concentration >0.60 and MIF −173 G/C or C/C;  , maximum O2 inspired concentration <0.60 and MIF −173 G/G;
, maximum O2 inspired concentration <0.60 and MIF −173 G/G;  , maximum O2 inspired concentration <0.60 and MIF −173 G/C or C/C.
, maximum O2 inspired concentration <0.60 and MIF −173 G/C or C/C.
DISCUSSION
Recent data in mice support a major role of MIF in lung maturation (23). In this study, we translated these findings into humans and report that MIF is highly expressed in lung tissues from preterm infants and that high circulating levels are present in preterm infants on d 1 after birth, particularly in those with RDS. We also found that in preterm infants a variant of the MIF promoter, which predisposes to high MIF protein expression, is associated with a lower risk to develop BPD.
MIF has been found in cord blood (32,33). However, to the best of our knowledge, no data are available in blood of term and preterm neonates. We found that circulating MIF was markedly increased (∼10 fold) in preterm neonates on d 1 after birth compared with healthy adults. Although no linear correlation was found between MIF levels and GA, median circulating levels of MIF in preterm neonates with GA <29 wk tended to be higher than those found in neonates with GA >29 ≤34 wk. However, because no samples were collected from healthy term infants, we cannot make any definitive conclusion whether increased MIF serum concentration is a characteristic limited to preterm neonates.
MIF may have multiple roles in neonates. It favors innate immune response and, for example, up-regulates TLR-4 expression (34); therefore, increased MIF levels may have a role in defense against infections. The above-mentioned data in mice suggest that MIF may also have a role in lung maturation (23). Although based on a limited number of samples, our observations on tissues suggest that MIF is highly expressed in lungs both before and after breathing. We also found that MIF levels were higher in preterm infants with RDS. Whether circulating levels reflect lung concentration remains to be established. However, increased levels in neonates with respiratory insufficiency may represent a generalized response to hypoxia. Indeed, MIF is induced by hypoxia in a hypoxia-inducible factor (HIF)-1 dependent manner (25,26). Moreover, supporting a positive loop between HIF and MIF, MIF itself is involved in HIF-1alpha protein stabilization and transactivation (35). HIFs are known to stimulate pulmonary vascular development, at least in part, through the induction of VEGF and VEGF-receptor expression (36). It is conceivable that MIF is part of a positive mechanism, maybe induced by a hypoxia condition, activated to promote lung maturation.
Although exposure of the immature lungs to environmental insults is thought to play a central role in the onset of BPD, heritability studies in monozygotic and dizygotic twins have shown that as much as 53% of the variance in the risk of BPD is accounted for by genetic factors (8). Genes regulating lung development, the balance between pro- and anti-inflammation, O2 toxicity, and tissue repair have been studied, and potential candidates have been identified (9). Given the animal data and our present results, also MIF emerges as a potential candidate. The MIF promoter contains a SNP in position −173 that is functionally relevant with the C allele associated with higher MIF expression in vitro and in vivo in healthy controls and in patients with juvenile idiopathic arthritis (27–29). The frequency of the −173 G/C and C/C genotypes together in the preterm infants studied (22.3%) was similar to that (26%) of a group (n = 96) of term infants with GA >37 wk (not shown), suggesting no association of this SNP with preterm birth. Evaluation of the MIF −173 genotype revealed that carriage of the high producing MIF −173*C allele conferred a significantly lower risk for the development of BPD. In the multivariate analysis, this decreased risk was independent from other known risk factor for BPD, including duration of O2 therapy and maximal inspired O2 concentration. Both in univariate and multivariate analysis, the association with the MIF allele was significant when a composite outcome (BPD or death before 36 wk PCA) was used. Using the variables included in the model shown in Table 5, the probability of developing BPD in preterm neonates mechanically ventilated for >10 d with a maximal O2 inspired concentration >0.60 was 38% in carriers of the MIF −173*C allele compared with 94.4% in carriers of the MIF −173 G/G genotype. It should be noted that, although data in mice and our data demonstrated that MIF is expressed in lung tissue, there are no data showing that the −173 SNP specifically impacts MIF protein expression in the lungs. In this respect, Kevill et al. (23) showed that, in patients who developed BPD, MIF levels in tracheal aspirates were lower than those of patients who did not develop BPD, further supporting the association between lung MIF expression and BPD.
Some of the studies that reported gene polymorphisms associated with BPD did not evaluate the independency from O2 exposure (10,13,14), making it rather difficult to evaluate the interaction of the associated polymorphisms with the main environmental causative factor of BPD. Interestingly, a recent report showed that a promoter polymorphism (−460 T/C) of the VEGF gene was associated with an increased risk of BPD, independently from the duration of O2 exposure (12). Given the fact that MIF has been shown to promote angiogenesis (19,20) and to induce VEGF production in the neonatal mouse lung (23), and that both genes are HIF-inducible, it is tempting to speculate that polymorphisms of the MIF and VEGF genes may affect the same maturational pathway in neonatal lung. Future studies on larger groups of preterm infants should investigate the interaction between these two genes in determining the susceptibility to BPD. It should also be mentioned that the stratification of MIF −173 alleles varies significantly in different ethnic groups (37), and therefore, future studies should also evaluate this association in different ethnicities.
In conclusion, our results in preterm neonates support the role of MIF in lung maturation and in lung repair. Our findings also suggest that, if confirmed by independent genetic investigation and supportive experimental evidence, genotyping for the MIF −173 polymorphism may prove to be helpful in identifying newborns at high risk for BPD. Possible adjustments in ventilation strategies may be used in these neonates and, in addition, therapeutic insufflations with MIF could be envisaged.
Abbreviations
- BPD:
-
bronchopulmonary dysplasia
- HIF:
-
hypoxia-inducible factor
- IQR:
-
interquartile range
- MIF:
-
macrophage migration inhibitory factor
- PCA:
-
postconceptional age
- SNP:
-
single nucleotide polymorphism
References
Bokodi G, Treszl A, Kovacs L, Tulassay T, Vasarhelyi B 2007 Dysplasia: a review. Pediatr Pulmonol 42: 952–961
Greenough A 2008 Long-term pulmonary outcome in the preterm infant. Neonatology 93: 324–327
Chess PR, D'Angio CT, Pryhuber GS, Maniscalco WM 2006 Pathogenesis of bronchopulmonary dysplasia. Semin Perinatol 30: 171–178
Ryan RM, Ahmed Q, Lakshminrusimha S 2008 Inflammatory mediators in the immunobiology of bronchopulmonary dysplasia. Clin Rev Allergy Immunol 34: 174–190
Bry K, Lappalainen U, Hallman M 1997 Intraamniotic interleukin-1 accelerates surfactant protein synthesis in fetal rabbits and improves lung stability after premature birth. J Clin Invest 99: 2992–2999
Shimoya K, Taniguchi T, Matsuzaki N, Moriyama A, Murata Y, Kitajima H, Fujimura M, Nakayama M 2000 Chorioamnionitis decreased incidence of respiratory distress syndrome by elevating fetal interleukin-6 serum concentration. Hum Reprod 15: 2234–2240
Kramer BW 2008 Antenatal inflammation and lung injury: prenatal origin of neonatal disease. J Perinatol 28: S21–S27
Bhandari V, Bizzarro MJ, Shetty A, Zhong X, Page GP, Zhang H, Ment LR, Gruen JR 2006 Familial and genetic susceptibility to major neonatal morbidities in preterm twins. Pediatrics 117: 1901–1906
Bhandari V, Gruen JR 2006 The genetics of bronchopulmonary dysplasia. Semin Perinatol 30: 185–191
Hadchouel A, Decobert F, Franco-Montoya ML, Halphen I, Jarreau PH, Boucherat O, Martin E, Benachi A, Amselem S, Bourbon J, Danan C, Delacourt C 2008 Matrix metalloproteinase gene polymorphisms and bronchopulmonary dysplasia: identification of MMP16 as a new player in lung development. PLoS ONE 3: e3188
Hallman M, Marttila R, Pertile R, Ojaniemi M, Haataja R 2007 Genes and environment in common neonatal lung disease. Neonatology 91: 298–302
Kwinta P, Bik-Multanowski M, Mitkowska Z, Tomasik T, Legutko M, Pietrzyk JJ 2008 Genetic risk factors of bronchopulmonary dysplasia. Pediatr Res 64: 682–688
Manar MH, Brown MR, Gauthier TW, Brown LA 2004 Association of glutathione-S-transferase-P1 (GST-P1) polymorphisms with bronchopulmonary dysplasia. J Perinatol 24: 30–35
Rova M, Haataja R, Marttila R, Ollikainen V, Tammela O, Hallman M 2004 Data mining and multiparameter analysis of lung surfactant protein genes in bronchopulmonary dysplasia. Hum Mol Genet 13: 1095–1104
Strassberg SS, Cristea IA, Qian D, Parton LA 2007 Single nucleotide polymorphisms of tumor necrosis factor-alpha and the susceptibility to bronchopulmonary dysplasia. Pediatr Pulmonol 42: 29–36
Calandra T, Roger T 2003 Macrophage migration inhibitory factor: a regulator of innate immunity. Nat Rev Immunol 3: 791–800
Ayoub S, Hickey MJ, Morand EF 2008 Mechanisms of disease: macrophage migration inhibitory factor in SLE, RA and atherosclerosis. Nat Clin Pract Rheumatol 4: 98–105
Renner P, Roger T, Calandra T 2005 Macrophage migration inhibitory factor: gene polymorphisms and susceptibility to inflammatory diseases. Clin Infect Dis 41: S513–S519
Kim HR, Park MK, Cho ML, Yoon CH, Lee SH, Park SH, Leng L, Bucala R, Kang I, Choe J, Kim HY 2007 Macrophage migration inhibitory factor upregulates angiogenic factors and correlates with clinical measures in rheumatoid arthritis. J Rheumatol 34: 927–936
Xu X, Wang B, Ye C, Ye C, Yao C, Lin Y, Huang X, Zhang Y, Wang S 2008 Overexpression of macrophage migration inhibitory factor induces angiogenesis in human breast cancer. Cancer Lett 261: 147–157
Donnelly SC, Haslett C, Reid PT, Grant IS, Wallace WA, Metz CN, Bruce LJ, Bucala R 1997 Regulatory role for macrophage migration inhibitory factor in acute respiratory distress syndrome. Nat Med 3: 320–323
Lai KN, Leung JC, Metz CN, Lai FM, Bucala R, Lan HY 2003 Role for macrophage migration inhibitory factor in acute respiratory distress syndrome. J Pathol 199: 496–508
Kevill KA, Bhandari V, Kettunen M, Leng L, Fan J, Mizue Y, Dzuira JD, Reyes-Mugica M, McDonald CL, Baugh JA, O'Connor CL, Aghai ZH, Donnelly SC, Bazzy-Asaad A, Bucala RJ 2008 A role for macrophage migration inhibitory factor in the neonatal respiratory distress syndrome. J Immunol 180: 601–608
Marsh LM, Cakarova L, Kwapiszewska G, von Wulffen W, Herold S, Seeger W, Lohmeyer J 2009 Surface expression of CD74 by type II alveolar epithelial cells: a potential mechanism for macrophage migration inhibitory factor-induced epithelial repair. Am J Physiol Lung Cell Mol Physiol 296: L442–L452
Welford SM, Bedogni B, Gradin K, Poellinger L, Broome Powell M, Giaccia AJ 2006 HIF1alpha delays premature senescence through the activation of MIF. Genes Dev 20: 3366–3371
Baugh JA, Gantier M, Li L, Byrne A, Buckley A, Donnelly SC 2006 Dual regulation of macrophage migration inhibitory factor (MIF) expression in hypoxia by CREB and HIF-1. Biochem Biophys Res Commun 347: 895–903
Donn R, Alourfi Z, De Benedetti F, Meazza C, Zeggini E, Lunt M, Stevens A, Shelley E, Lamb R, Ollier WE, Thomson W, Ray D 2002 Mutation screening of the macrophage migration inhibitory factor gene: positive association of a functional polymorphism of macrophage migration inhibitory factor with juvenile idiopathic arthritis. Arthritis Rheum 46: 2402–2409
De Benedetti F, Meazza C, Vivarelli M, Rossi F, Pistorio A, Lamb R, Lunt M, Thomson W, Ravelli A, Donn R, Martini A 2003 Functional and prognostic relevance of the −173 polymorphism of the macrophage migration inhibitory factor gene in systemic-onset juvenile idiopathic arthritis. Arthritis Rheum 48: 1398–1407
Vivarelli M, D'Urbano LE, Insalaco A, Lunt M, Jury F, Tozzi AE, Ravelli A, Martini A, Donn R, De Benedetti F 2007 Macrophage migration inhibitory factor (MIF) and oligoarticular juvenile idiopathic arthritis (o-JIA): association of MIF promoter polymorphisms with response to intra-articular glucocorticoids. Clin Exp Rheumatol 25: 775–781
Meazza C, Travaglino P, Pignatti P, Magni-Manzoni S, Ravelli A, Martini A, De Benedetti F 2002 Macrophage migration inhibitory factor in patients with juvenile idiopathic arthritis. Arthritis Rheum 46: 232–237
Vivarelli M, D'Urbano LE, Stringini G, Ghiggeri GM, Caridi G, Donn R, Tozzi A, Emma F, De Benedetti F 2008 Association of the macrophage migration inhibitory factor −173*C allele with childhood nephrotic syndrome. Pediatr Nephrol 23: 743–748
Matoba N, Yu Y, Mestan K, Pearson C, Ortiz K, Porta N, Thorsen P, Skogstrand K, Hougaard DM, Zuckerman B, Wang X 2009 Differential patterns of 27 cord blood immune biomarkers across gestational age. Pediatrics 123: 1320–1328
Ietta F, Todros T, Ticconi C, Piccoli E, Zicari A, Piccione E, Paulesu L 2002 Macrophage migration inhibitory factor in human pregnancy and labor. Am J Reprod Immunol 48: 404–409
Roger T, David J, Glauser MP, Calandra T 2001 MIF regulates innate immune responses through modulation of toll-like receptor 4. Nature 414: 920–924
Oda S, Oda T, Nishi K, Takabuchi S, Wakamatsu T, Tanaka T, Adachi T, Fukuda K, Semenza GL, Hirota K 2008 Macrophage migration inhibitory factor activates hypoxia-inducible factor in a p53-dependent manner. PLoS ONE 3: e2215
Rajatapiti P, van der Horst IW, de Rooij JD, Tran MG, Maxwell PH, Tibboel D, Rottier R, de Krijger RR 2008 Expression of hypoxia-inducible factors in normal human lung development. Pediatr Dev Pathol 11: 193–199
Zhong XB, Leng L, Beitin A, Chen R, McDonald C, Hsiao B, Jenison RD, Kang I, Park SH, Lee A, Gregersen P, Thuma P, Bray-Ward P, Ward DC, Bucala R 2005 Simultaneous detection of microsatellite repeats and SNPs in the macrophage migration inhibitory factor (MIF) gene by thin-film biosensor chips and application to rural field studies. Nucleic Acids Res 33: e121
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by the Department of Health, Italy.
Rights and permissions
About this article
Cite this article
Prencipe, G., Auriti, C., Inglese, R. et al. A Polymorphism in the Macrophage Migration Inhibitory Factor Promoter Is Associated With Bronchopulmonary Dysplasia. Pediatr Res 69, 142–147 (2011). https://doi.org/10.1203/PDR.0b013e3182042496
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e3182042496
This article is cited by
-
Bronchopulmonary dysplasia and wnt pathway-associated single nucleotide polymorphisms
Pediatric Research (2022)
-
Verification of immunology-related genetic associations in BPD supports ABCA3 and five other genes
Pediatric Research (2022)
-
Inhibition of microRNA-451 is associated with increased expression of Macrophage Migration Inhibitory Factor and mitigation of the cardio-pulmonary phenotype in a murine model of Bronchopulmonary Dysplasia
Respiratory Research (2020)
-
Small molecular modulation of macrophage migration inhibitory factor in the hyperoxia-induced mouse model of bronchopulmonary dysplasia
Respiratory Research (2013)
-
Pancreatic stone protein as a novel marker for neonatal sepsis
Intensive Care Medicine (2013)