Abstract
The reason why some infants with respiratory distress syndrome fail to respond to surfactant, or respond only transiently, is incompletely understood. We hypothesized that resuscitation with large breaths at birth might damage the lungs and blunt the effect of surfactant. Five pairs of lamb siblings were delivered by cesarean section at 127-128 d of gestation. One lamb in each pair was randomly selected to receive six manual inflations of 35-40 mL/kg (“bagging”) before the start of mechanical ventilation, a volume roughly corresponding to the inspiratory capacity of lamb lungs after prophylactic surfactant supplementation. Both siblings were given rescue porcine surfactant, 200 mg/kg, at 30 min of age. Blood gases and deflation pressure-volume (P-V) curves of the respiratory system were recorded until the lambs were killed at 4 h. The P-V curves became steeper after surfactant in the control group, but no such effect was seen in those subjected to bagging. At 4 h, inspiratory capacity and maximal deflation compliance were almost three times higher (p < 0.01) in the controls than in the bagged lambs. The latter were also more difficult to ventilate and tended to have less well expanded alveoli and more widespread lung injury in histologic sections. We conclude that a few inflations with volumes that are probably harmless in other circumstances might, when forced into the surfactant-deficient lung immediately at birth, compromise the effect of subsequent surfactant rescue treatment. Our findings challenge current neonatal resuscitation practice of rapidly establishing a normal lung volume by vigorous manual ventilation.
Similar content being viewed by others
Main
In animal models of respiratory distress syndrome, total lung capacity is reduced by a widespread proteinaceous edema(1) caused by transepithelial leakage of macromolecules(2). This leakage occurs both in ventilated and unventilated segments of the lungs(3) and is probably a consequence of the postnatal increase in blood flow in an immature lung. However, it is aggravated by mechanical ventilation(3), probably because breaths forced into the lungs cause epithelial disruption(4). If surfactant is given immediately after birth, the epithelial damage may be prevented(4) and the protein leak diminished(2), but if instilled after a longer or shorter period of mechanical ventilation, the surfactant may be inactivated by the leaking protein and may fail to enter collapsed or fluid-filled lung regions(5).
Although experiments thus suggest that surfactant should be given early, randomized clinical trials have not consistently yielded better outcome after prophylactic surfactant treatment than after rescue therapy(6). To administer surfactant, the trachea must be intubated. Because the premature newborn often develops hypoxia and bradycardia soon after birth, it may be difficult to abstain from ventilating the lungs until the drug has been instilled. In fact, in most clinical comparisons between prophylaxis and rescue, the prophylactic treatment was sometimes(7) or always(8, 9) given after the infant had been ventilated for a short period. Pilot animal experiments made us surmise that ventilation-induced lung damage might occur within seconds, if vigorous bag-and-mask ventilation were used after birth or the lungs inflated forcefully after tracheal intubation to recruit volume and ascertain that the tube had been correctly placed. It is therefore possible that, in the above-mentioned studies, the decisive lung trauma had already occurred when the “prophylactic” surfactant was given. In the present study, we tested whether as few as six large breaths, given shortly after birth, would blunt the therapeutic effect of subsequent surfactant replacement in immature lambs.
METHODS
Overview of the study. A series of five two-lamb siblings were randomized pairwise to either receive or not receive six large breaths at birth. The large breaths were administered with a neonatal resuscitation bag. Surfactant was given after a period of cautious mechanical ventilation, at 30 min of age. Three lambs, studied subsequently, received surfactant before the first breath and were used to establish that the size of the breaths was not harmful per se.
The study was approved by the local Institutional Review Board for animal research.
Surfactant. The surfactant used in these experiments was isolated from minced pig lungs by a sequence of steps including washing, extraction with chloroform-methanol, and liquid-gel chromatography(10). The final product contained about 99% polar lipids(mainly phospholipids) and 1% hydrophobic proteins (surfactant proteins B and C in approximate molar proportions 1:2). It was administered at a concentration of 80 mg/mL.
Procedure in the bagged lambs and their sibling controls. Cesarean section was done in date-mated ewes, carrying more than one lamb, at 127-128 d postconception. The ewe was premedicated with xylazine, 6-8 mg i.m., before transportation to the laboratory. After sedation with ketamine, 35 mg i.v., anesthesia was induced with thiopental, 650-800 mg i.v., and maintained with isoflurane in nitrous oxide/oxygen after intubation of the trachea. The lungs were ventilated with a Servo Ventilator 900 B. End-tidal Pco2 was held at 4.5-6 kPa. Maintenance fluid with a balanced glucose/salt solution was given. Arterial pressure was monitored through an indwelling arterial cannula, and systolic pressure was maintained between 90 and 110 mm Hg by adjusting the isoflurane concentration and infusing Ringer's acetate as needed.
With the ewe on her right side, the uterus was exposed through a lateral subcostal incision. The head of the lamb was exteriorized, and possible breathing attempts were prevented by threading a rubber glove over the snout; however, probably because of the isoflurane anesthesia, such attempts were never seen. A 3.5- or 4.0-mm inner diameter tracheal tube was inserted through an incision in the trachea, so that the tip was located well above the carina. The tube was secured with ligatures around the trachea to prevent any leak. Ten milliliters of lung fluid were removed by syringe and immediately frozen for analysis of phospholipid content. During the following procedure additional lung fluid was allowed to slowly drain through plastic tubing connected to a small bag. All in all, approximately 20 mL of lung fluid were removed before the start of ventilation. Catheters were inserted into a jugular vein and a carotid artery. The lamb was given ketamine 8 mg and pancuronium 0.4 mg i.v., and the umbilical cord was cut.
An overview of the subsequent experiment is given in Figure 1. The lamb was weighed and placed in an open incubator. In the study group (“bagging”) a self-inflating neonatal resuscitation bag (Laerdal, Saltsjö Boo, Sweden), with an oxygen supply set at 10 L/min, was connected to the endotracheal tube. The bag was squeezed nearly maximally six times with the pop-off valve inactivated, yielding breaths of 120-130 mL, and each breath was held at maximal inspiration for 5 s. This was found to result in a fraction of inspired oxygen(Fio2) of approximately 75%. The airway pressure, as measured with a calibrated anaeroid manometer, was noted at the end of the sixth insufflation(see Table 1). All the lambs were bagged by the same investigator. The tracheal tube was then connected with a Servo Ventilator(model 900C; Siemens-Elema, Solna, Sweden) in the pressure control mode; ventilatory rate 50/min; inspiratory time 50% of the cycle; and Fio2 0.9. These settings were held unchanged. PEEP was initially set at 4 cm H2O, but in four lambs PEEP was increased during the study to a maximum of 6 cm H2O to counteract hypoxia. Inspiratory pressure was initially set at 29 cm H2O (25 cm H2O + PEEP), but was later adjusted with the aim of achieving a Paco2 of approximately 6 kPa. However, peak inspiratory pressure was not allowed to exceed 40 cm H2O. Ketamine, 1 mg/mL in 5% glucose, was infused at a rate of 4 mL/kg/h. The arterial catheter was connected to a pressure transducer. If mean arterial pressure was less than 40 mm Hg, then 10 mL/kg blood was taken from the ewe and given to the lamb, unless the lamb's Hb concentration in blood simultaneously exceeded 150 g/L, in which case Ringer's acetate was instead used for volume expansion. Ten milliliters/kg blood was likewise given if Hb was less than 130 g/L. One mmol/kg sodium bicarbonate was given if the pH was less than 7.25 and base deficit more than 5 mmol/L.
At approximately 10 min of age, an anteroposterior chest radiograph was taken to reveal possible pneumothorax. An arterial sample was withdrawn for measurement of blood gases (ABL 300, Radiometer, Denmark), and static expiratory P-V diagrams of the respiratory system were obtained(11). Briefly, the lungs were inflated with a syringe to an airway pressure of 35 cm H2O. After maintaining this pressure for 15 s, the lungs were allowed to empty passively through a flowmeter and through an electronically operated occluder, which cyclically interrupted the expired flow for 80 ms and let it through for 80 ms. The slow expiration, which lasted 10-15 s, continued until airway pressure was 0 cm H2O (or, to be more precise, until it was less than 0.5 cm H2O). A computer recorded the pressure during each flow interruption, and used the flow signal to calculate the volume decrement between successive interruptions so that a P-V diagram could be drawn. At each stage of the experiment, three to four diagrams were made.
The following measures were extracted from the P-V curves: IC,i.e. the expired volume between 30 and 0 cm H2O, and Crsmax, i.e. the steepest slope of the P-V curve. Because we had previously found that these parameters tended to increase somewhat with repeated inflations, the means from the last two acceptable curves obtained at each stage were used.
At 30 min of age, surfactant 200 mg/kg (=2.5 mL/kg) was given through a feeding tube inserted to reach the lower trachea just below the tip of the endotracheal tube. Half the dose was given as a rapid bolus with the lamb lying on its side. After 1 min of mechanical ventilation, the lamb was turned to its opposite side, and the other half dose was given. New blood gas samples and P-V diagrams were taken at a further five stages, namely at approximately 45, 75, 135, 175, and 235 min of age. Two additional chest radiographs were made at 70 and 230 min. At the end of the experiment, cardiac arrest was induced with an overdose of thiopental.
All chest radiographs were examined for the presence of pneumothorax, first by the investigators during the experiments, and then retrospectively by a pediatric radiologist, who was unaware both of the aim of the study and of the treatment given.
Lambs given surfactant before the first breath. Gestational age was the same as for the first 10 lambs, 127-128 d. One lamb (no. 11) was given surfactant before delivery. The surfactant was mixed with 15 mL of lung fluid in a syringe, which was then attached to the tracheal tube. After emptying the mixture into the lungs, the plunger was moved back and forth five times with the aim of distributing surfactant evenly in the lungs. Thereafter, the tube was clamped. Ventilation was started about 10 min later when the umbilical cord had been cut. Bagging was done at 30 min of age. Otherwise the protocol was essentially the same as for the other bagged lambs.
Two lambs (nos. 12 and 13) were part also of another experiment and were not bagged. They were given surfactant after the umbilical cord had been cut and before the start of mechanical ventilation, as a single bolus into the lower trachea with the lamb supine. Repeated P-V diagrams were made during the next 4 h, as described above.
Preparation of the lungs for light microscopy. After death, the lungs were ventilated with air for 5 min, after which a constant airway pressure of 10 cm H2O was applied. The diaphragms were inspected from the abdominal side to reveal pneumothorax, and the lungs and heart were then removed en bloc. The ductus arteriosus was ligated. The airway pressure was increased to 30 cm H2O for a few minutes. It was again decreased to 10 cm H2O, and the lungs were perfused through the pulmonary artery with normal saline, until the effluent was free of blood. The perfusate was changed to 4% formaldehyde, 300 mL of which were infused during the next 30 min. The lungs were then stored in formaldehyde, the continuous distending pressure of 10 cm H2O being maintained overnight.
Histologic examination of lungs. Large paraffin sections from all lung lobes, stained with hematoxylin and eosin, were examined by light microscopy with particular reference to the alveolar expansion pattern, necrosis and desquamation of airway epithelium, alveolar hyaline membranes, and recruitment of granulocytes to the air spaces. The effect of surfactant treatment was classified as satisfactory if ≥75% of the alveoli were estimated to be air-expanded, and evidence of lung injury (epithelial necrosis, hyaline membranes, and recruitment of granulocytes) was limited to wedges of nonaerated parenchyma, usually present in the subpleural region. It was rated as suboptimal if the estimated proportion of aerated alveoli was above 50% but less than 75%, and unsatisfactory if ≤50% of the alveoli were air-expanded. The examination of the lung sections was carried out blindly,i.e. without knowledge of the experimental condition of individual animals.
Statistics. Comparisons between the bagged lambs and their sibling controls were made with the t test for paired samples. Two-sided p values <0.05 were taken to indicate statistical significance. In addition, the effect of time and bagging on Pao2 was evaluated with a repeated measures ANOVA procedure. This was done as a precaution against reporting spurious significance due to t testing at multiple stages. As only three lambs were given surfactant before the first breath, we chose not to do any significance testing between these and the 10 lambs given surfactant at 30 min of age.
RESULTS
Lung function in the bagged lambs and their sibling controls. An overview of the studied lambs is given in Table 1. Four ewes were delivered of twins. One ewe carried four lambs. The second quadruplet died during delivery, so the first and third quadruplets were studied.
Two lambs, both bagged (nos. 8 and 10), had a right-sided pneumothorax at autopsy. In one of them (no. 10), a small basal pneumothorax was evident also in the final chest radiograph, but there was no pneumothorax in the preceding radiographs. In four other lambs (nos. 3, 4, 6, and 9), the radiologist suspected a small pneumothorax, in all cases because of a diffusely increased radiolucency in one lung field in the final radiographs. None of these lambs had pneumothorax at autopsy, and the radiologic findings probably represented a locally increased aeration in the lung itself.
Phospholipid content in fluid aspirated from the trachea was <0.1 mg/mL in all lambs in which it was analyzed (four pairs), indicating a severe surfactant deficiency(12). There was no significant difference in phospholipid content between the bagged lambs and their controls.
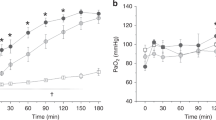
In the controls, surfactant had the expected effect on lung mechanics with the P-V curve becoming steeper with time (Fig. 2). No such effect was seen in the bagged lambs. As a consequence, the curves describing changes in IC over time diverged (Fig. 3). A similar, large difference between groups was seen for Crsmax(Table 2).
Mean expiratory P-V curves of the respiratory system for the bagged lambs (right panel) and their sibling controls(left panel) at six different times after birth. The bagged lambs were given six deep breaths with a Laerdal neonatal resuscitation bag shortly after birth, whereas the control lambs were directly connected to the ventilator. Surfactant was given at 30 min in both groups.
IC, i.e. the volume change between 30 and 0 cm H2O airway pressure, in the bagged lambs and their sibling controls(left panel), and in the lambs treated with surfactant before the first breath (right panel). In the left panel, symbols indicate group means and error bars indicate standard deviations. The significance of between-group differences (t tests for paired samples) are indicated: NS, not significant; *p < 0.05;**p < 0.01; ***p < 0.001. It is shown that bagging severely compromised the effect of subsequent surfactant treatment. It is also shown that lambs treated with surfactant before the first breath had a much better IC than those bagged at birth and that bagging did not damage an already expanded lung with adequate surfactant content (lamb no. 11, bagged at 30 min).
Before instillation of surfactant, there was no significant difference in Pao2, Paco2, or pH between the bagged lambs and their sibling controls (Table 2). After surfactant treatment, Paco2 was greater in the bagged lambs (significant at 75, 135, and 175 min) in spite of attempts to reduce it by increasing the inspiratory pressure. As a consequence, inspiratory pressure was significantly greater in the bagged lambs at all time points after the first hour. Pao2 increased after administration of surfactant in both groups (p < 0.01). The increase was more pronounced in the controls, but the difference between groups was significant only at 45 min of age, i.e. 15 min after surfactant treatment.
Lung function in lambs given surfactant before the first breath. Each of the three lambs given surfactant before the first breath had a higher Pao2 and IC/weight and a lower Paco2 when first studied at 10-25 min of age than any of the 10 lambs who were given surfactant later on, at 30 min of age. IC was approximately 25 mL/kg when it was first measured and subsequently increased to values between 36 and 45 mL/kg at 4 h of age (Fig. 3). The lamb that was bagged at 30 min of age (no. 11) showed a 51% increase in IC within 15 min after bagging, and IC then increased by a further 22% during the following 3 h.
Crsmax increased rapidly in all three lambs and was 3.5-4.3 mL/kg/cm H2O at 4 h. At the same time Pao2 was between 8.4 and 30.2 kPa, Paco2 was 4.4-6.0 kPa, and inspiratory pressure 18-22 cm H2O.
At 4 h IC/weight (Fig. 3) and Crsmax/weight were greater and inspiratory pressure less in each of these lambs than in any of those bagged at birth. The values in the group of sibling controls tended to be intermediate, but with some overlap.
Histologic findings. The histologic findings in the bagged lambs and their sibling controls (lambs nos. 1-10) are summarized in Table 3 and illustrated in Figures 4 and 5. In the animal receiving surfactant before delivery (no. 11), the treatment response was rated as optimal. In one of the two lambs that were treated with surfactant at birth without previous bagging, the response was likewise graded as optimal; in the other animal it was classified as suboptimal.
Histologic findings in animal with a clearly unsatisfactory response to surfactant treatment. This lamb (no. 8) was subjected to the bagging maneuver at birth, and IC after 4 h of mechanical ventilation was only 9.4 mL/kg. Hematoxylin and eosin stain. (A) Low power field showing poor aeration of the alveolar compartment; magnification,×14. (B) Detail illustrating prominent lung injury characterized by epithelial necrosis in peripheral conducting airways(asterisk), alveolar hyaline membranes, and recruitment of granulocytes to the air spaces; magnification, ×65.
Histologic findings in animal with optimal response to surfactant treatment. This lamb (no. 9) was not subjected to the bagging maneuver. IC recorded after 4 h of mechanical ventilation was 40.4 mL/kg. Hematoxylin and eosin stain. (A) Low power field showing uniform aeration of most alveoli, except for small wedges of nonexpanded parenchyma in the subpleural region; magnification, ×14. (B) Detail illustrating well expanded parenchyma without evidence of lung injury; magnification, ×65.
Lambs with morphologic evidence of widespread lung injury had a lower IC than those with an optimal surfactant response. At 4 h of age IC was 37± 8 mL/kg (mean ± SD) in animals with a treatment response rated histologically as optimal. In animals with a treatment response rated as suboptimal the corresponding value was only 24 ± 11 mL/kg, and in animals with unsatisfactory response it was 14 ± 8 mL/kg. The difference between the lambs with an optimal response and those with an unsatisfactory response was statistically significant (p < 0.01; two-sample t test).
DISCUSSION
The main result of this study was that a few large breaths (35-40 mL/kg), given at birth to immature lambs, inhibited the effect on lung mechanics of subsequently instilled natural surfactant (Figs. 2–5; Table 2). Strictly speaking, we measured P-V relations of the total respiratory system rather than those of the lungs. However, because the chest wall contributes little to total elastance in lambs(13), the distinction has little real significance. That lung compliance was poor in the bagged lambs is reflected also by the high Paco2 that was recorded in spite of attempts to reduce it by increasing the inspiratory pressure (Table 2). Two of the bagged lambs had pneumothorax at autopsy, but this does not explain the findings, as a marked difference between the bagged lamb and its control was seen also in the other three sibling pairs. In addition, the repeat chest radiographs indicated that the gas leaks into the pleura were small and probably developed at a late stage. The histologic findings were in keeping with lung mechanics as recorded just before sacrifice. Thus, mean IC/weight in the lambs with morphologic evidence of severe lung injury(unsatisfactory surfactant response) was only about half of that in the lambs with a surfactant response rated histologically as optimal.
In contrast to the lack of effect on lung mechanics in the bagged lambs, surfactant caused a significant increase in Pao2. A similar phenomenon was encountered in human infants given late rescue surfactant treatment for respiratory distress syndrome(14), in whom there was no correlation between early improvement in oxygenation and lung volume changes. At later stages in the present study, Pao2 tended to fall both in the lambs subjected to the bagging maneuver and in the controls, and after 1 h the difference in Pao2 between the two groups was no longer significant. This was in spite of a large difference in IC and Crsmax. A similar course was reported previously in an early study of surfactant-treated preterm lambs(15), in which Pao2 fell to pretreatment levels within a few hours, whereas compliance remained high. The reasons for the poor correlation between oxygenation and lung mechanics remain obscure, but may possibly be related to changes in intra- or extrapulmonary shunting of blood.
Why did the few large breaths have such a deleterious effect on lung function? Several factors may be considered, namely the high airway pressure during bagging, the size of the breaths, the time at which they were given, and the surfactant deficiency in the lungs.
High airway pressure was needed to force gas into the lungs during the insufflations (Table 1). However, animal studies have demonstrated that lung overdistension, rather than the elevated airway pressures per se, is responsible for the development of acute lung injury during mechanical ventilation(16). Although similar studies have not been done in newborn or immature animals, one would expect that the same applies to these. Furthermore, during the bagging maneuver, the epithelium was subjected to high pressure for only siz times at 5 s each, which seems unlikely to cause permanent damage.
It might be argued that the breaths were so large that severe damage was inevitable, whatever the circumstances. However, we rather believe that the timing of inflations was decisive, i.e. that they were given at birth when the lung was still fluid-filled and surfactant-deficient. Although findings from single animals must be interpreted with caution, the results from lambs nos. 11-13 seem to indicate that such large inflations are not harmful when given to a lung with adequate surfactant content at a time when most of the lung fluid is absorbed. Thus, the lamb given surfactant before delivery (no. 11) and later bagged at 30 min with as many and as large breaths consistently showed much greater inspiratory capacity and compliance than the lambs that were bagged at birth (Fig. 3). In histologic sections, this lamb also showed an optimal response to surfactant, with little evidence of epithelial injury, no hyaline membranes, and no recruitment of granulocytes to air spaces. Furthermore, lamb nos. 12 and 13, that were given surfactant after delivery but before the first breath, had an IC of 35-40 mL/kg from 1 h of age and onward. This means that repeated P-V maneuvers were done with similar volumes as those insufflated during bagging, and yet caused no apparent injury.
The importance of surfactant deficiency for the development of lung injury during mechanical ventilation has been studied in the immature rabbit model(4, 17, 18). Newborn lungs with adequate surfactant content can be ventilated, at least for short time periods (10 min), with high pressures, and consequently relatively large tidal volumes, with no untoward effect, as the alveoli expand synchronously and the inspired gas is distributed uniformly in the parenchyma(18). If, on the other hand, some alveoli remain unexpanded throughout the ventilatory cycle, and others are subjected to iterated reopening and collapse, considerable shear forces may be generated in the airway epithelial lining during respiration. This problem is typical of the surfactant-deficient lung, and necrosis and desquamation of airway epithelium, similar to what occurred in the lambs subjected to the bagging maneuver (Fig. 4B), are probably triggered by mechanical disruption, in turn caused by overexpansion of the airway during inspiration. The development of this type of ventilator-induced epithelial injury can be prevented by treatment with surfactant at birth(4, 18).
Can the harmful effect of the bagging maneuver also be wholly or partly prevented by preceding surfactant supplementation, thus strengthening the argument for surfactant treatment before the first breath? This is plausible, but not necessarily conclusive, from the present data. Mechanical ventilation is usually pressure-limited, and though overexpansion of the ventilated part of the lung does occur, this mode still offers some degree of protection against very large tidal volumes. In contrast, the bagging maneuver implied that a predetermined volume was delivered to the lung at birth, irrespective of the pressure needed. In the study by Grossmann et al.(18) of immature rabbits, a peak pressure of approximately 35 cm H2O typically resulted in tidal volumes of 10-13 mL/kg during the first 5-10 min, in contrast to the 35-40 mL/kg given immediately after birth in the present study. Before surfactant rescue, IC is very low (Fig. 3, left panel), probably because of a delayed absorption of lung liquid, and large inflation volumes may easily cause overexpansion of the small air-filled lung parts. However, even when surfactant is administered before the first breath, a maximal IC is not established until around 1 h (Fig. 3, right panel), and there may still be an early period when the lung is sensitive to overdistension.
Kendig et al.(19) found that immediate surfactant prophylaxis before the first breath resulted in significantly better survival than rescue treatment in very premature infants (≤26-wk gestation). However, a recent study from the same group(20) showed an even better survival when prophylaxis was postponed until respiration was established. One explanation may be that immediate bolus prophylaxis requires immediate intubation, and surfactant instillation will then be followed by early manual ventilation, which may cause overexpansion of the lungs.
It may be questioned if the volutrauma used in this study is clinically relevant, i.e. if preterm infants would ever be subjected to inflations as large as 35-40 mL/kg during resuscitation. We find it quite possible that they may. It is often recommended that preterm infants who do not establish regular respiration spontaneously immediately after delivery should be intubated and given positive pressure ventilation [see e.g. Roberton(21)]. During bag ventilation, airway pressure is usually not monitored, and if there is a pop-off valve it is often deliberately inactivated during the first few breaths. Less force is needed to squeeze a small resuscitation bag than a larger one, and the neonatologist may not feel that considerable pressure is generated. Therefore the size of the breaths will be governed by the magnitude of thoracic excursions rather than pressure. The Laerdal bag used in the present study is the manufacturer's smallest model and is recommended for use in neonates. We found that the squeezes used for the bagging maneuvers yielded a volume of approximately 120 mL. A seemingly small squeeze of one fifth of this volume will result in an inflation of 24 mL (40 mL/kg in a 600-g infant). Monitoring inflation volumes during bag ventilation is usually not feasible, but monitoring pressure is easy and will serve the same purpose. There is equipment available for pressure-limited ventilation during resuscitation(Neopuff RD1000, Fisher & Paykel, Auckland, NZ), but as a minimum safety precaution, a manometer could be attached to the resuscitation bag, so that the neonatologist is alerted if excessive pressures are generated(22).
Our data suggest that ventilation techniques commonly and successfully used in mature or older infants to recruit lung volume and provide the tissues with oxygen may be inappropriate for very immature infants at birth. For resuscitation of term neonates, long inflation times (2-5 s) are recommended, with the explicit aim of achieving larger tidal volumes(21). Likewise, in older neonates, prolonged breaths that achieve marked thoracic expansion may sometimes be beneficial,e.g. to eliminate atelectasis after endotracheal suctioning. However, if such techniques are used during resuscitation of immature infants at birth, the effect may be deleterious.
In summary, this study shows that manual ventilation with a few large breaths at birth may cause lung injury and blunt the effect of subsequent surfactant treatment. The immature lung may be particularly vulnerable at birth not only because it lacks surfactant but also because it is fluid-filled with little room for air entry. Ventilation with large breaths may cause gross overexpansion of regions that are forced open, leaving major parts of the lung blocked by fluid and unexpanded. Such regional overdistension can be expected to cause epithelial and microvascular injury and an increased fluid flux into the air spaces. The resulting edema may not only cause surfactant inactivation but probably also may make the lung more susceptible to further volutrauma during conventional mechanical ventilation(23).
The risk of lung injury is in all likelihood related to the magnitude of the volutrauma at birth. However, preliminary data from a new series of experiments in immature lambs suggest that reducing the manual insufflations at birth to half or even one fourth of the volumes used here does not completely abolish their harmful effect(24). Ventilation early after birth may therefore need to be very gentle.
Abbreviations
- Crsmax:
-
maximal deflation compliance of the respiratory system
- Fio2:
-
fraction of inspired oxygen
- IC:
-
inspiratory capacity
- PEEP:
-
positive end-expiratory pressure
- P-V:
-
pressure-volume
- Pao2:
-
arterial O2 pressure
- Paco2:
-
arterial CO2 pressure
References
Jackson JC, Mackenzie AP, Chi EY, Standaert TA, Truog WE, Hodson WA 1990 Mechanisms for reduced total lung capacity at birth and during hyaline membrane disease in premature newborn monkeys. Am Rev Respir Dis 142: 413–419.
Robertson B, Berry D, Curstedt T, Grossmann G, Ikegami M, Jacobs H, Jobe A, Jones A 1985 Leakage of protein in the immature rabbit lung: effect of surfactant replacement. Respir Physiol 61: 265–276.
Berry D, Jobe A, Ikegami M 1991 Leakage of macromolecules in ventilated and unventilated segments of preterm lamb lungs. J Appl Physiol 70: 423–429.
Nilsson R, Grossmann G, Robertson B 1978 Lung surfactant and the pathogenesis of neonatal bronchiolar lesions induced by artifical ventilation. Pediatr Res 12: 249–255.
Seidner SR, Ikegami M, Yamada T, Rider ED, Castro R, Jobe AH 1995 Decreased surfactant dose-response after delayed administration to preterm rabbits. Am J Respir Crit Care Med 152: 113–120.
Soll RF 1995 Clinical trials of surfactant therapy in the newborn. In: Robertson B, Taeusch HW (eds) Surfactant Therapy for Lung Disease. Marcel Dekker, New York, pp 407–441.
Dunn MS, Shennan AT, Zayack D, Possmayer F 1991 Bovine surfactant replacement therapy in neonates of less than 30 wk gestation: a randomized controlled trial of prophylaxis versus treatment. Pediatrics 87: 377–386.
Merritt TA, Hallman M, Berry C, Pohjavuori M, Edwards DK, Jaaskelainen J, Grafe MR, Vaucher Y, Wozniak P, Heldt G, Rapola J 1991 Randomized, placebo-controlled trial of human surfactant given at birth versus rescue administration in very low birth weight infants with lung immaturity. J Pediatr 118: 581–594.
Walti H, Paris-Llado J, Breart G, Couchard M, the French Collaborative Study group 1995 Porcine surfactant replacement therapy in newborns of 25-31 wk gestation: a randomized, multicentre trial of prophylaxis versus rescue with multiple doses. Acta Paediatr 84: 913–921.
Robertson B, Curstedt T, Johansson J, Jörnvall H, Kobayashi T 1990 Structural and functional characterization of porcine surfactant isolated by liquid-gel chromatography. Prog Respir Res 25: 237–246.
Vilstrup C, Gommers D, Bos JAH, Lachmann B, Werner O, Larsson A 1992 Natural surfactant instilled in premature lambs increases lung volume and improves ventilation homogeneity within five minutes. Pediatr Res 32: 595–599.
Cummings JJ, Holm BA, Hudak ML, Hudak BB, Ferguson WH, Egan EA 1992 A controlled clinical comparison of four different surfactant preparations in surfactant-deficient preterm lambs. Am Rev Respir Dis 145: 999–1004.
Davis GM, Coates AL, Papageorgiou A, Bureau MA 1988 Direct measurement of static chest wall compliance in animal and human neonates. J Appl Physiol 65: 1093–1098.
Björklund LJ, Vilstrup CT, Larsson A, Svenningsen NW, Werner O 1996 Changes in lung volume and static expiratory pressure-volume diagram after surfactant rescue treatment of neonates with established respiratory distress syndrome. Am J Respir Crit Care Med 154: 918–923.
Jobe A, Ikegami M, Glatz T, Yoshida Y, Diakomanolis E, Padbury J 1981 Duration and characteristics of treatment of premature lambs with natural surfactant. J Clin Invest 67: 370–375.
Martin LD 1995 New approaches to ventilation in infants and children. Curr Opin Pediatr 7: 250–261.
Nilsson R, Grossmann G, Robertson B 1980 Bronchiolar epithelial lesions induced in the premature rabbit neonate by short periods of artificial ventilation. Acta Pathol Microbiol Scand Sect A Pathol 88: 359–367.
Grossmann G, Nilsson R, Robertson B 1986 Scanning electron microscopy of epithelial lesions induced by artificial ventilation of the immature neonatal lung; the prophylactic effect of surfactant replacement. Eur J Pediatr 145: 361–367.
Kendig JW, Notter RH, Cox C, Reubens LJ, Davis JM, Maniscalco WM, Sinkin RA, Bartoletti A, Dweck HS, Horgan MJ, Risemberg H, Phelps DL, Shapiro DL 1991 A comparison of surfactant as immediate prophylaxis and as rescue therapy in newborns of less than 30 wk gestation. N Engl J Med 324: 865–871.
Kendig JW, Cox C, Maniscalco WM, Sinkin RA, Reubens L, Horgan MJ, Dweck HS, Phelps DL, the Rochester Surfactant Study Group 1996 Surfactant prophylaxis as immediate bolus (IB) versus post-ventilatory aliquots (PVA): a multicenter randomized trial. Pediatr Res 39: 221A
Roberton NRC 1995 Resuscitation of the newborn infant. In: Yu VYH (ed) Pulmonary Problems in the Neonatal Period and their Sequelae. Baillière's Clinical Pediatrics, Vol 3(1). Baillière Tindall, London, pp 1–26.
Goldstein B, Catlin EA, Vetere JM, Arguin LJ 1989 The role of in-line manometers in minimizing peak and mean airway pressure during the hand-regulated ventilation of newborn infants. Respir Care 34: 23–27.
Dreyfuss D, Soler P, Saumon G 1995 Mechanical ventilation-induced pulmonary edema: interaction with previous lung alterations. Am J Respir Crit Care Med 151: 1568–1575.
Björklund LJ, Curstedt T, Ingimarsson J, Larsson A, Robertson B, Svenningsen NW, Werner O 1996 Lung injury caused by neonatal resuscitation of immature lambs-relation to volume of lung inflations. Pediatr Res 39: 326A ( abstr).
Acknowledgements
The authors thank veterinary surgeon Eva Swanberg, neonatal nurses Ingela Mattisson-Sandström and Ulla Ganestam, and research engineer Mikael Tarland for technical assistance. The chest radiographs were examined by Peter Hochbergs and Catarina Holmqvist, Department of Radiology, University Hospital, Lund. Per-Erik Isberg, Department of Statistics, Lund University, gave advice on the numerical analysis.
Author information
Authors and Affiliations
Additional information
Supported by grants from the Swedish Medical Research Council (Project Nos. 3351 and 4732), the Medical Faculty of Lund University (4421-4 and 4021-2), the Swedish Society for Medical Research, Oscar II:s Jubileumsfond, and Ove Bengtsson's Foundation for Research on Prematurity.
Rights and permissions
About this article
Cite this article
Björklund, L., Ingimarsson, J., Curstedt, T. et al. Manual Ventilation with a Few Large Breaths at Birth Compromises the Therapeutic Effect of Subsequent Surfactant Replacement in Immature Lambs. Pediatr Res 42, 348–355 (1997). https://doi.org/10.1203/00006450-199709000-00016
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199709000-00016
This article is cited by
-
Comparison of positive pressure ventilation devices during compliance changes in a neonatal ovine model
Pediatric Research (2024)
-
NON-pharmacological Approach Less Invasive Surfactant Administration (NONA-LISA) trial: protocol for a randomised controlled trial
Pediatric Research (2024)
-
A clinical study evaluating the combination of LISA and SNIPPV for the treatment of respiratory distress syndrome in preterm infants
Scientific Reports (2024)
-
Oscillatory mechanics at birth for identifying infants requiring surfactant: a prospective, observational trial
Respiratory Research (2021)
-
T-piece resuscitator or self-inflating bag during neonatal resuscitation: a scoping review
Pediatric Research (2021)