Abstract
We investigated the early postnatal changes of the mesenteric circulation and its relation to the systemic circulation in 15 preterm infants. The infants were studied before the first feeding on d 1 and pre- and postprandially on d 3, 4, 5, and 7. Blood flow velocity was measured by ultrasound Doppler in the superior mesenteric artery, middle cerebral artery, and the aortic orifice for cardiac output calculations. Blood pressure and heart rate were monitored. From d 1 to d 3, the preprandial stroke volume decreased [1.5 ± 0.3 to 1.3 ± 0.2 mL/kg (mean ± SD),p < 0.05], whereas blood pressure (36 ± 3 to 50 ± 7 mm Hg, p < 0.001), superior mesenteric artery mean velocity(Vmean) (0.17 ± 0.08 to 0.30 ± 0.11 m/s,p < 0.05), and middle cerebral artery Vmean increased (0.15 ± 0.05 to 0.22 ± 0.03 m/s, p < 0.001). From d 3 through d 7, the preterm infants demonstrated higher preprandial end diastolic flow velocity in the superior mesenteric artery than we previously reported in term infants (0.15 ± 0.05 versus 0.12 ± 0.04, p < 0.05). Like the term infants, preterm infants increased their superior mesenteric artery Vmean by 83% postprandially and maintained a stable cerebral circulation with feeding. Unlike the term infants, feeding in the preterm infants induced a blood pressure decrease (51 ± 6 to 48 ± 6 mm Hg, p < 0.01) and a cardiac output increase (176 ± 30 to 188 ± 32 mL/kg/min, p < 0.001). These findings suggest that, in contrast to term infants, healthy preterm infants require compensatory systemic hemodynamic changes in response to feeding.
Similar content being viewed by others
Main
In newborn infants, major changes in the cardiovascular system take place at birth. These postnatal circulatory changes include alterations in systemic hemodynamics as well as changes in the distribution of blood flow to various regions. Disturbances in this circulatory adjustment may contribute to the pathogenesis of cerebral hemorrhages(1) and necrotizing enterocolitis(2, 3). Difference in postnatal circulatory adaptation and circulatory responses to feeding between preterm and term infants may play a role in the increased incidence of these diseases in preterm infants.
The aim of this study was to investigate the postnatal systemic, intestinal, and cerebral circulatory adaptation and the hemodynamic response pattern to feeding in the appropriate for gestational age preterm infants.
METHODS
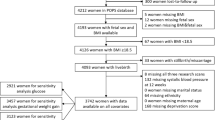
Subjects. Fifteen preterm infants were included in the study, nine were delivered vaginally and six by cesarean section. All infants were appropriate for gestational age (mean birth weight 2296 g, range 1980-2930 g; mean gestational age 34 wk, range 33-35 wk). Two of the mothers were given tocolytics (β agonists) and five mothers were given steroids before delivery. After birth, all infants had a pH above 7.25, and none of them needed ventilation or extra oxygen. The ductus arteriosus closed spontaneously in all infants. No one had any clinical signs of infection, and blood cultures were negative. On d 3-7, some infants had phototherapy for hyperbilirubinemia(d 3: two infants, d 4, 5, and 7: three infants).
To follow the early changes in the transitional circulation and the effect on regional blood flow, the first examination was performed at 2-5 h of age in nine infants (early group) and at 6-24 h of age in six infants (late group). All infants in both groups were reexamined daily on d 3, 4, 5, and 7.
No infants were fed milk, but three infants were fed 5-20 mL of 5% glucose at least 2 h before the first examination. The feeding interval was 3 h on all days. From d 3 to d 7 they were given increasing amounts of milk [9.9 ± 3.5 mL (mean ± SD), 13.0 ± 4.3, 18.9 ± 5.8, 21.7 ± 4.1 mL]. When available the infants were given mother's milk (on d 3 to 7; 2, 10, 11, and 12 infants respectively), and the remaining infants were given formula milk. The study was approved by the local ethical committee, and informed written consent was obtained from the parents.
A duplex scanner with pulsed Doppler and color flow mapping was used(Vingmed CFM 750, Vingmed Sound, Horten, Norway). The transducer used was 7.5 MHz for tissue imaging and 6.0 MHz for the Doppler recordings. TheVmax envelope was traced immediately after each recording. The instrument was programmed to calculate the Vmax,Vmean, and heart rate by tracing the velocity envelope. The EDFV was measured manually from the hard copies of the spectral tracings. An average of at least two measurements was used for the velocity tracings and aortic diameter calculations.
Measurement of cardiac output. From a right upper parasternal long axis view, the aortic flow velocity was obtained by placing the sample volume at the level of the aortic orifice. Velocity wave forms were considered optimal when the leaflet signal was on the recordings and the characteristic sound of the aortic Doppler signal was maximal. In the parasternal long axis view, the aortic diameter was measured as the distance between the attachment of the aortic leaflets (trailing to leading edge method) in systole when the leaflets were maximally separated. By entering the diameter of the aortic orifice after the aortic velocity curve was traced, the instrument calculated stroke volume and the cardiac output was obtained by multiplying with heart rate. The mean of at least two cardiac output calculations was used, normalized for weight, and expressed as mL/min/kg.
Ductus arteriosus. Using a parasternal short axis view the patency of and the direction of the ductal shunt was evaluated by color flow mapping.
Blood flow velocity measurements. For imaging of the superior mesenteric artery the transducer was placed on the mid abdomen above the umbilicus in the sagittal plane. Color flow mapping was used to identify the artery where it originated from the aorta. The sample volume of the pulsed Doppler was placed a few millimeters distal to the origin of the superior mesenteric artery. Angle correction was used when necessary; this varied from examination to examination. When stable wave forms were obtained, the curve was traced and the blood flow velocity was calculated.
Guided by color flow mapping the middle cerebral artery was located with the transducer perpendicular to the pterion part of the temporal bone, and blood flow velocity was measured.
The examination was performed in the following order: superior mesenteric artery, cardiac output, and middle cerebral artery. Blood pressure was then measured by an oscillometric method (Dinamap; Critikon Inc., Tampa, FL). The ratio of mean blood pressure to superior mesenteric arteryVmean was used as an index of relative mesenteric vascular resistance. The infants were examined in an incubator or in a heated bed maintaining a stable temperature. Whenever restlessness occurred, measurements were made after the infants were properly soothed and were quiet. The total examination time was approximately 0.5 h for each infant. All infants were examined by the same investigator. Preprandial examinations on d 3-7 were performed immediately before a feeding, and the postprandial examinations were performed 0.5 h after the feeding had been completed.
Statistical evaluations. To test the changes within the groups, early and late, a repeated measure analysis of variance was used. Thereafter, a paired t test was used to localize the changes within the groups. A repeated measures analysis of variance with a grouping factor (earlyversus late group) was used to test for differences between the groups. An unpaired t test was used to localize the differences. The difference in change from d 1 to d 3 between the groups was tested separately to further evaluate the changes during the first day. For comparison between preterm and the previously reported term infants(4), unpaired t test was used. Values are expressed as mean ± SD. The relationship between mean blood pressure and middle cerebral arteryVmean was tested for significance with Pearson's correlation test.
RESULTS
Circulatory Changes during the First 7 Days of Life
The circulatory changes over time are demonstrated by comparing the results from the measurements on d 1 before feeding and the preprandial measurements from d 3 through d 7.
Systemic circulation (Figs. 1 and2). Cardiac output and heart rate did not change either in the early or in the late examined group during the study. Stroke volume decreased, from d 1 to d 3, in the early examined group, whereas no changes occurred in the late examined group. From d 1 to d 3, mean blood pressure increased both in the early and in the late examined group. In both groups, there was no change in cardiac output, heart rate, stroke volume, or mean blood pressure after d 3. When comparing the two groups of infants, there were no differences in cardiac output, heart rate, stroke volume, or mean blood pressure.
Ductus arteriosus. At the first examination, the ductus arteriosus was open, shunting left to right, in all infants in the early examined group. In the late examined group, the ductus arteriosus was open, shunting left to right in four infants, and it was closed in two infants. The ductus was spontaneously closed in all infants on d 3.
Superior mesenteric artery (Fig. 3). Superior mesenteric artery Vmean and EDFV increased from d 1 to d 3 in the early examined group, whereas no significant changes occurred in the late examined group. On d 1, EDFV was negative in one infant and zero in seven infants in the early group, whereas all EDFV were positive in the late examined group. In both groups, there was no change in superior mesenteric artery Vmean or EDFV after d 3. When comparing the two groups of infants, there were no differences in superior mesenteric arteryVmean. In contrast EDFV was significantly lower in the early than in the late group on d 1. Furthermore, the increase in EDFV from d 1 to d 3 in the early group was significantly larger than in the late group(p < 0.05)
Middle cerebral artery (Fig. 4). Middle cerebral artery Vmean and EDFV increased from d 1 to d 3 in the early examined group, whereas no significant changes occurred in the late examined group. In both groups, there were no changes in middle cerebral artery Vmean or EDFV after d 3. When comparing the two groups of infants, there were no differences in middle cerebral arteryVmean or EDFV. However, the increase in EDFV from d 1 to d 3 in the early group was significantly larger than in the late group(p < 0.05). There was, when d 1 measurements and the prefed measurements during d 3 through 7 were included, a significant correlation between middle cerebral artery Vmean and blood pressure(r = 0.43, p < 0.001).
From d 3 through d 7, there were no changes in any of the preprandial measurements and there were no differences between the early and the late examined group as shown by the overlapping curves. Thus, the data of the two groups in this period of the study can be treated as belonging to one group.
Circulatory Responses to Feeding
From d 3 to d 7 the infants were fed increasing amounts of milk. As there were no differences between the early and the late examined groups and the circulatory responses to feeding were similar on all days, the preprandial data on d 3 through d 7 were combined, as were the postprandial data.
Superior mesenteric artery (Fig. 5). Superior mesenteric artery Vmean and EDFV increased postprandially. Vmean increased by 83% (56-103%), and EDFV increased by 77% (45-104%). The ratio of mean blood pressure to superior mesenteric artery Vmean was used as an index of relative mesenteric vascular resistance. This ratio decreased postprandially.
Feeding associated changes in superior mesenteric artery (SMA) Vmean, EDFV, and index of relative vascular resistance [mean blood pressure (BP)/SMA Vmean] in 15 preterm infants. The infants were examined before feeding and 0.5 h after the feeding had been completed. As the circulatory responses to feeding were similar on all days, the preprandial data on d 3 through 7 were combined, as were the postprandial data. *p < 0.001 vs prefeeding.
Middle cerebral artery. No feeding-related changes were found in the middle cerebral artery Vmean or EDFV (data not shown).
Systemic circulation (Fig. 6). Cardiac output increased whereas mean blood pressure decreased postprandially. The increase in cardiac output was the result of an increase in stroke volume whereas heart rate remained unchanged.
Feeding associated changes in cardiac output and mean blood pressure in 15 preterm infants. The infants were examined before feeding and 0.5 h after the feeding had been completed. As the circulatory responses to feeding were similar on all days, the preprandial data on d 3 through 7 were combined, as were the postprandial data. *p < 0.01vs prefeeding.
Comparison between Preterm and Term Infants
The results of the present study were compared with the results of our previously reported data of term infants (Table 1). The preterm infants had higher EDFV and lower relative vascular resistance in the superior mesenteric artery preprandially than the term infants. However, middle cerebral artery Vmean and EDFV were lower in the preterm than in the term infants.
DISCUSSION
Circulatory Changes during the First 7 d of Life
Systemic circulation. The decrease in stroke volume in the early, but not in the late, examined group, may reflect that a decrease in ductal shunting had already occurred at 6 h of age(5, 6). Closure of the duct may also explain the increased mean blood pressure on d 3; however, increasing peripheral vascular resistance with age in preterm infants(7) could also have contributed to this increase in mean blood pressure.
Superior mesenteric artery. Ductal steal effect on the mesenteric circulation has been described not only in preterm infants with symptomatic patent ductus arteriosus(8), but also in healthy term infants(4). The low superior mesenteric artery Vmean and EDFV in the early group, and the large increase in EDFV from d 1 to d 3 in this group, suggest a ductal steal effect on the mesenteric circulation during the first hours of life in healthy preterm infants. Feeding was well established on d 3, and the increased preprandial superior mesenteric artery Vmean and EDFV on d 3 may therefore not only represent the closure of the duct, but also the priming effect of feeding(9).
Middle cerebral artery. A ductal steal effect on the cerebral circulation, with decreased Vmean, has been reported in healthy preterm infants(10), but not in healthy term infants(4, 11). In our study, the low middle cerebral artery Vmean and EDFV on d 1 in the early group could therefore represent a ductal steal effect. This is further supported by the larger increase in EDFV from d 1 to d 3 in the early than in the late group. In contrast to the finding in the superior mesenteric artery, no difference was found in EDFV in the early versus the late group on d 1. Therefore, we speculate that the ductal steal effect on the cerebral circulation was not as pronounced as in the intestinal circulation. Furthermore, factors such as changes in CO2 reactivity(12) and increasing cerebral metabolic demands(13) may also have contributed to the increase on d 3.
The correlation between the middle cerebral artery Vmean and blood pressure may suggest a pressure-passive relationship. However, preterm newborn lambs have been shown to autoregulate their cerebral blood flow with a more narrow range of blood pressure than their term counterpart(14). A more likely explanation for the simultaneous increase in blood pressure and cerebral blood flow may therefore be a shift of the autoregulatory range in the first week of life in healthy preterm infants.
In agreement with previous reports(15, 16), we found lower cerebral blood flow velocities in the preterm than in the term infants. It has been speculated that lower neuronal activity and lower metabolic requirements could result in lower blood flow in the preterm brain(17–19).
Circulatory Responses to Feeding
The preterm infants demonstrated higher preprandial superior mesenteric artery EDFV and lower relative vascular resistance than term infants(4). This difference may reflect the generally lower vascular resistance in the preterm infant(7). It may also reflect a selectively lower intestinal vascular resistance caused by the metabolic demand of a rapidly growing gut. Recent investigations suggest an increased production of nitric oxide in the mesenteric circulation in younger compared with older animals and may explain an increased EDFV as a result of a lower vascular tone in preterm infants(20). The influence of some more frequent feeding in preterm infants (every 3 h) than in the term infants (every 4 h) could, however, not be excluded. The postprandial increase in superior mesenteric artery Vmean was of the same magnitude in preterm as in term infants. On d 3-7 some infants had phototherapy for hyperbilirubinemia. In term infants phototherapy blunted the postprandial superior mesenteric artery Vmean response(21). In this study we could not confirm this finding in the infants who received phototherapy. However, this study was not designed to investigate the effect of phototherapy on intestinal blood flow so that the duration on or off light was not strictly monitored in relation to feeding. Further studies are therefore required to evaluate the effect of phototherapy on the mesenteric circulatory response to feeding in preterm infants.
As a response to feeding we found a decrease in blood pressure and an increase in cardiac output. This suggests that a systemic circulatory compensation for the increased blood flow to the gut during digestion and absorption of food is necessary in preterm infants. In contrast, the term infants showed no changes in cardiac output and blood pressure with feeding(4). Peripheral vasoconstriction with feeding has been reported in term infants(22). This did not occur in preterm infants(23). The lack of associated changes in the peripheral circulation with feeding in preterm infants may thus represent a developmental immaturity of that vascular bed. As in the term infants, cerebral blood flow remained constant with feeding(4). Therefore, to increase blood flow to the gut during feeding, the preterm required increases in cardiac output. In the sick preterm infant, when systemic hemodynamics are unstable, we speculate that the circulatory responses to feeding may be compromised and lead to insufficient intestinal circulation.
Conclusion. Our results suggest that preterm infants have lower intestinal vascular resistance than term infants. The postprandial increase in superior mesenteric artery Vmean was of the same magnitude in preterm and term infants, and the preterm infants were also able to maintain a stable cerebral circulation with feeding. However, in the preterm infants there was a feeding-associated systemic hemodynamic compensation for the increased blood flow to the gut.
Abbreviations
- Vmean:
-
mean velocity
- EDFV:
-
end diastolic flow velocity
References
Van Bel F, Van de Bor M, Stijnen T, Baan J, Ruys JH 1987 Aetiological role of cerebral blood-flow alterations in development and extension of peri- intraventricular haemorrhage. Dev Med Child Neurol 29: 601–614
Schwartz MZ, Palder SB, Tyson KRT, Marr CC 1988 Complications of prematurity that may require surgical intervention. Arch Surg 123: 1135–1138
Cassady G, Crouse DT, Kirklin JW, Strange MJ, Joiner CH, Godoy G, Odrezin GT, Cutter GR, Kirklin JK, Pacifico AD, Collins MV, Lell WA, Satterwhite C, Philips JB 1989 A randomized, controlled trial of very early prophylactic ligation of the ductus arteriosus in babies who weighed 1000 g or less at birth. N Engl J Med 320: 1511–1516
Martinussen M, Brubakk A-M, Linker DT, Vik T, Yao AC 1994 Mesenteric blood flow velocity and its relation to circulatory adaptation during the first week of life in healthy term infants. Pediatr Res 36: 334–339
Winberg P, Ergander U 1992 Relationship between heart rate, left ventricular output, and stroke volume in preterm infants during fluctuations in heart rate. Pediatr Res 31: 117–120
Mellander M, Larsson LE 1988 Effects of left-to-right ductus shunting on left ventricular output and cerebral blood flow velocity in 3-day-old preterm infants with and without severe lung disease. J Pediatr 113: 101–109
Wu PYK, Wong WH, Guerra G, Miranda R, Godoy RR, Preston B, Schoentgen S, Levan NE 1980 Peripheral blood flow in the neonate. 1. Changes in total, skin, and muscle blood flow with gestational and postnatal age. Pediatr Res 14: 1374–1378
Coombs RC, Morgan MEI, Durbin GM, Booth IW, McNeish AS 1990 Gut blood flow velocities in the newborn: effects of patent ductus arteriosus and parenteral indomethacin. Arch Dis Child 65: 1067–1071
Leidig E 1989 Doppler analysis of superior mesenteric artery blood flow in preterm infants. Arch Dis Child 64: 476–480
Winberg P, Sonesson S-E, Lundell BPW 1990 Postnatal changes in intracranial blood flow velocity in preterm infants. Acta Paediatr Scand 79: 1150–1155
Sonesson S-E, Winberg P, Lundell BPW 1987 Early postnatal changes in intracranial arterial blood flow velocities in term infants. Pediatr Res 22: 461–464
Pryds O, Greisen G, Lou H, Friis-Hansen B 1989 Heterogeneity of cerebral vasore-activity in preterm infants supported by mechanical ventilation J P. ediatr 115: 638–645
Duffy TE, Kohle SJ, Vannucci RC 1975 Carbohydrate and energy metabolism in perinatal rat brain: relation to survival in anoxia. J Neurochem 24: 271–276
Papile L-N, Rudolph AM, Heymann MA 1985 Autoregulation of cerebral blood flow in the preterm fetal lamb. Pediatr Res 19: 159–161
Raju TNK, Kim SY 1989 Cerebral artery flow velocity acceleration and deceleration characteristics in newborn infants. Pediatr Res 26: 588–592
Horgan JG, Rumack CM, Hay T, Manco-Johnson ML, Merenstein GB, Esola C 1989 Absolute intracranial blood-flow velocities evaluated by duplex Doppler sonography in asymptomatic preterm and term neonates. AJR 152: 1059–1064
Richardson BS, Patrick JE, Abduljabbar H 1985 Cerebral oxidative metabolism in the fetal lamb: relationship to electrocortical state. Am J Obstet Gynecol 153: 426–431
Holowach Thurston J, McDougal Jr DB 1969 Effect of ischemia on metabolism of the brain of the newborn mouse. Am J Physiol 216: 348–352
Hernandez MJ, Brennan RW, Vannucci RC, Bowman GS 1978 Cerebral blood flow and oxygen consumption in the newborn dog. Am J Physiol 234: 209–215
Nowicki PT, Nankervis CA 1994 The role of the circulation in the pathogenesis of necrotizing enterocolitis. Clin Perinat 21: 219–234
Yao AC, Martinussen M, Johansen O-J, Brubakk A-M 1994 Phototherapy-associated changes in mesenteric blood flow response to feeding in term neonates. J Pediatr 124: 309–312
Yao AC, Wallgren G, Sinha SN, Lind J 1971 Peripheral circulatory response to feeding in the newborn infant. Pediatrics 47: 378–383
Raziuddin K, Kim MH, Yao AC 1984 Peripheral circulatory response to feeding in newborn low-birth-weight infants. J Pediatr Gastroenterol Nutr 3: 89–94
Acknowledgements
The authors thank the nursing staff in the neonatal unit at University of Trondheim for their invaluable cooperation and assistance. We also thank Matt Avitable, Scientific Academic Computing Center, SUNY Health Science Center, Brooklyn, NY, for his statistical assistance.
Author information
Authors and Affiliations
Additional information
Supported by the Norwegian National Health Association, the Norwegian Research Council for Science and Humanities (NAVF) (No. 351.90/007), the Norwegian Marshall Fund, and the Foundation for Neonatal Research at the University of Trondheim.
Philip T. Nowicki, M.D., Children's Hospital, 700 Children's Drive, Columbus, OH 43205.
Rights and permissions
About this article
Cite this article
Martinussen, M., Brubakk, AM., Vik, T. et al. Mesenteric Blood Flow Velocity and Its Relation to Transitional Circulatory Adaptation in Appropriate for Gestational Age Preterm Infants. Pediatr Res 39, 275–280 (1996). https://doi.org/10.1203/00006450-199602000-00015
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199602000-00015
This article is cited by
-
Nutrition of the preterm infant with persistent ductus arteriosus: existing evidence and practical implications
Pediatric Research (2023)
-
Early brain and abdominal oxygenation in extremely low birth weight infants
Pediatric Research (2022)
-
Serial Doppler velocimetry of mesenteric and portal flow in very-low-birth-weight preterm neonates with and without patent ductus arteriosus
Pediatric Radiology (2020)
-
The effect of enteral bolus feeding on regional intestinal oxygen saturation in preterm infants is age-dependent: a longitudinal observational study
BMC Pediatrics (2019)
-
Challenges Associated with Route of Administration in Neonatal Drug Delivery
Clinical Pharmacokinetics (2016)