No CrossRef data available.
Article contents
Antipsychotic prescribing choices in patients with First Episode Psychosis
Published online by Cambridge University Press: 01 September 2022
Abstract
As all first line options in treating First Episode Psychosis (FEP) are similarly effective there is a consensus among prescribing guidelines that clinicians and patients should consider side-effect profile as the ‘driver’ of initial choice of antipsychotic. Anecdotally it has been observed that different care teams prescribe particular medications preferentially.
To evaluate the patterns of antipsychotic prescribing in patients with FEP at the time of initial treatment and over the first year with the Early Intervention Service (EIS).
Medical records of all patients who had completed 1 year of follow-up with EIS in Sussex Partnership Foundation Trust (n=274) were reviewed. The first antipsychotic prescribed and antipsychotic prescribed at 12-months was recorded alongside initiating care team (EIS, non-EIS community services, inpatient services).
99% (n=272) of patients were prescribed an antipsychotic. 46% were initiated by inpatient serves, 40% non-EIS community services and 14% EIS. Aripiprazole, olanzapine, quetiapine and risperidone accounted for 95% of initial prescriptions. Different care teams prescribed antipsychotics preferentially (p=<0.005) (Fig.1). Rates at which initial medication was continued at 12-months varied according to initial prescription (P=<0.05) (Fig.2).
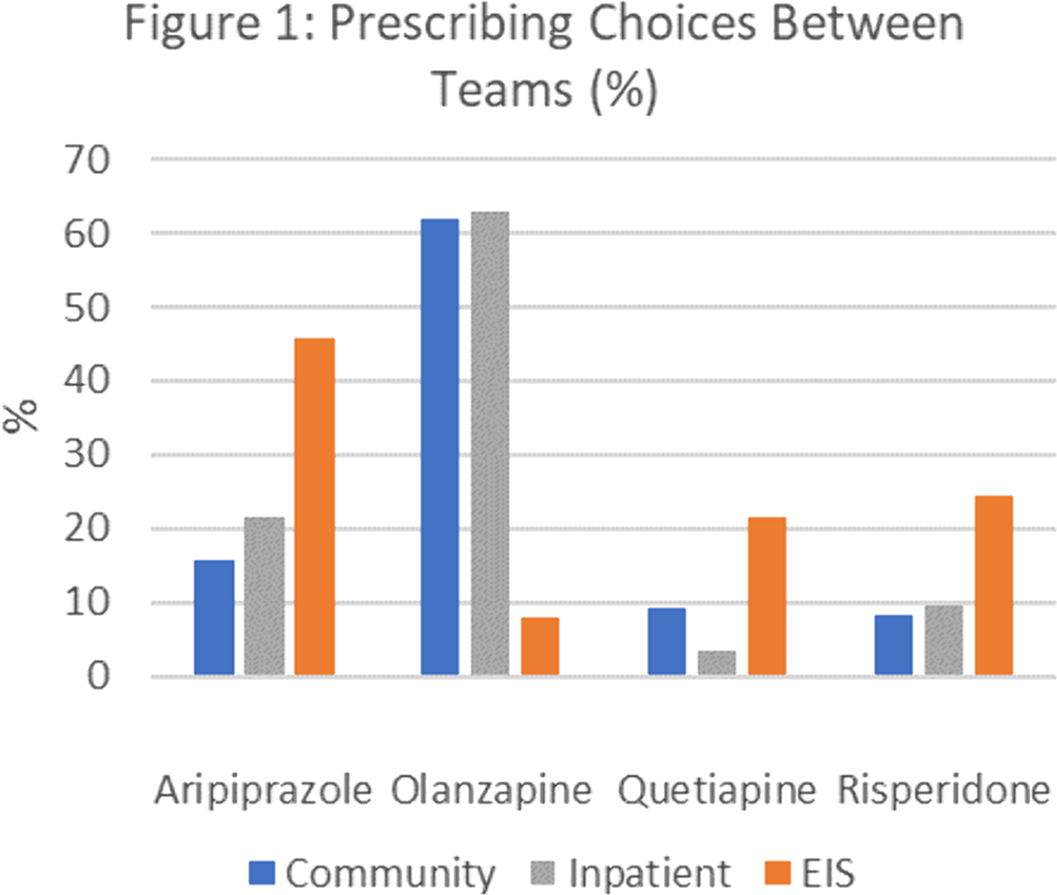
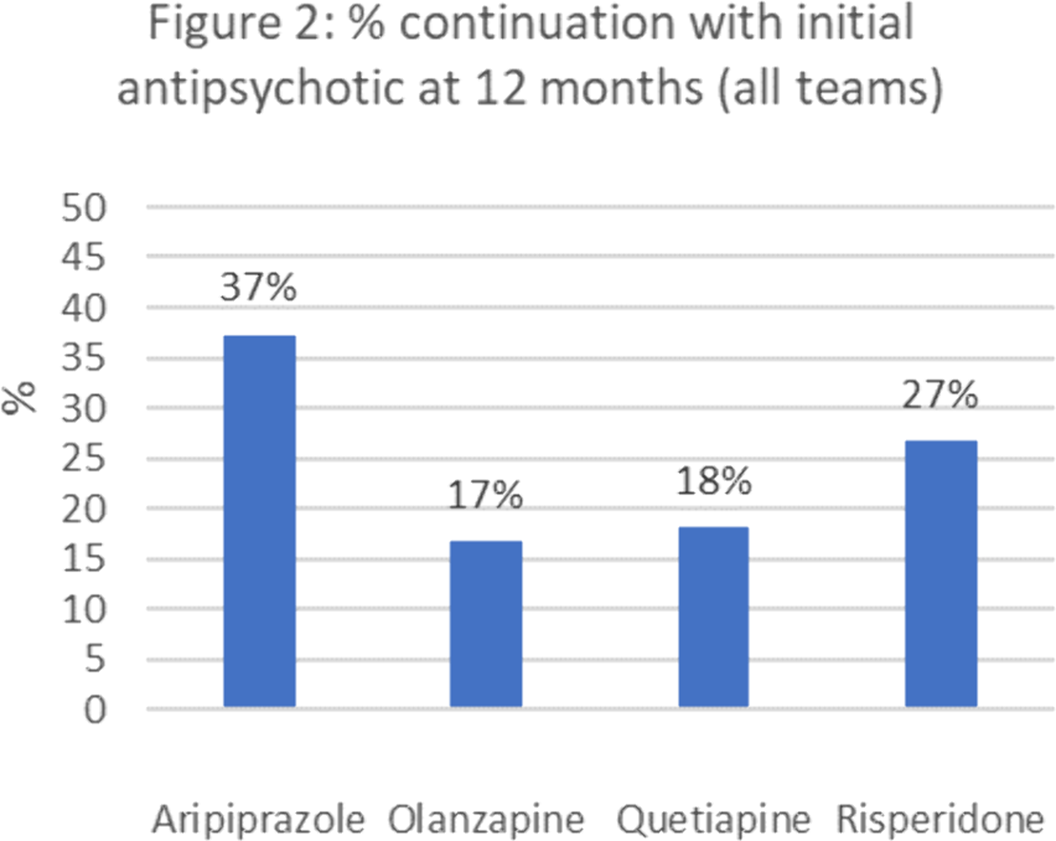
The frequency that specialist EIS services prescribed aripiprazole as initial treatment contrasts the preference for olanzapine in other services. Olanzapine has a significant metabolic side effect profile, is sedating and was least likely to be continued at 12 months. This raises questions about why non-FEP specialist services prefer olanzapine and whether EIS services can support these services around initial medication choices more likely to be continued throughout the key first year of treatment.
No significant relationships.
- Type
- Abstract
- Information
- European Psychiatry , Volume 65 , Special Issue S1: Abstracts of the 30th European Congress of Psychiatry , June 2022 , pp. S285
- Creative Commons
- This is an Open Access article, distributed under the terms of the Creative Commons Attribution licence (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted re-use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Copyright
- © The Author(s), 2022. Published by Cambridge University Press on behalf of the European Psychiatric Association





Comments
No Comments have been published for this article.