Abstract
Skilful use of the C Mac D-blade videolaryngoscope, with preservation of spontaneous respiration, can avert preoperative tracheostomy and guide microlaryngeal surgery (MLS) tube insertion in patients with large growths obliterating glottic view. The long narrow stylet accompanying double-lumen tubes can be used for D-Blade guided MLS tube orotracheal intubation. A definite protocol for safe insertion and removal of throat packs has been described here. Throat packs may go missing despite following protocols. Our algorithm includes visual and documentary precautions and means of exploration of missing throat packs. D-blade is invaluable in scanning the oropharynx in event of a lost throat pack.
Similar content being viewed by others
Introduction
D-blade (Doerges/difficult airway blade) is a remarkable extension of the C Mac videolaryngoscope (Karl Storz, Tuttlingen, Germany) in the anesthesiologist’s armamentarium with untapped potential benefits (Shah et al., 2016a; Shah et al., 2016b). In those difficult airway patients undergoing microlaryngeal surgery(MLS), where the extent of surgical resection does not warrant a postoperative tracheostomy, preoperative surgical airway can be avoided by skilful use of the D-blade in awake/anesthetized spontaneously breathing patients.
A throat pack comprises surgical gauze that absorbs fluids and stops surgical debris from entering the aerodigestive tract. Throat packs may alarmingly vanish, despite following a definite protocol for their safe insertion and removal (Colbert et al., 2012). D-blade is valuable in scanning the oropharynx in the event of a lost throat pack.
Case report
A 37-year-old, 45-kg lady presented at Rajiv Gandhi Cancer Institute and Research Centre with dysphagia. MRI revealed a massive hemangioma in the posterior supraglottic region involving both aryepiglottic folds extending into the right pyriform sinus. Her hematological and biochemical investigations were normal and laser excision was planned.
Patient was not premedicated. After applying standard monitors and securing an IV line in the operation theatre, the supraglottic area was sprayed with 10% lignocaine. Surgeons were gloved for an emergency backup tracheostomy. The lubricated stylet of a double-lumen tube was inserted into a straightened 5-mm internal diameter microlaryngeal surgery (MLS) tube followed by bending into a C-shaped curve conforming to the concavity of D-blade.
A check, awake D-blade laryngoscopy was performed to visualize the hemangioma and glottis (Fig. 1). In an anterior larynx [Cormack–Lehane grade IIb], only the posterior 10% comprising the arytenoids is visible. Contrarily, the anterior 10% glottis was visible in our patient, the remainder being obliterated by the hemangioma. After administering IV fentanyl (30 μg), anesthesia was deepened using 3% incremental sevoflurane maintaining spontaneous ventilation. The MLS tube was inserted with the concavity facing rightwards and rotated 90° anticlockwise once midway into the oral cavity to reach the barely visible chink of larynx above the tumor. The D-blade was withdrawn slightly, the BURP applied, the tumor pushed down by a suction catheter, the neck flexed by an assistant, and the trachea intubated. The stylet was withdrawn, and endotracheal placement capnographically confirmed. The deep and superficial cuffs were inflated with 2 ml saline and 3 ml methylene blue, respectively. Eyes were taped shut, and protective wet gauze and laser-proof goggles applied. Intravenous fentanyl (70 μg), propofol (60 mg), and atracurium (30 mg) were administered. Surgeons placed a wet oral pack (2 × 20 cm) around the tube. Anesthesia was maintained with sevoflurane in medical air and 35% oxygen, IV fentanyl 30 μg, hydrocortisone 100 mg, and atracurium (10 + 5) mg. The laser excision lasted 75 min.
When surgery ended, the throat pack went missing. The D-blade was utilized to systematically scan the oral cavity including both pyriform sulci. The MLS tube was included with the tongue and pushed up with the D-blade to visualise the area beneath it. Thorough suctioning was done. Raw mucosa and the laserized hemangioma stump could be visualised but not the throat pack. Swab count did not tally, so drapes, floor, and wastebins were re-checked. Fluoroscopy was not an option since the throat pack was devoid of radio-opaque markings. With the D-blade in situ, a fiberoptic bronchoscope (FOB) was inserted through the glottic chink above the ETT to rule out subglottic migration of pack. The upper esophagus and nasopharynx were also fiberoptic bronchoscopically examined. After an hour of repeated exploration, the elusive pack was finally retrieved from the mid-esophagus by the gastroenterologist using a gastroscope. IV hydrocortisone 100 mg and dexamethasone 8 mg were administered. The oral laser tube was replaced with a 7-mm ID nasal ETT, patient shifted to postoperative ward on a T-piece and uneventfully extubated over a bougie after 2 h.
Discussion
Spontaneous respiration must never be ablated in difficult airway patients. Awake intubation and inhalational induction are good options. D-blade videolaryngoscope rescued us from this tricky situation where loss of airway tone would have caused complete airway obstruction by the pedunculated tumor plug. Any bleeding from handling the hemangioma could lead to catastrophic aspiration. Young ladies with non-malignant pathologies deserve a chance to avoid disfiguring tracheostomies with potential complications including tracheal stenosis. Hence, tracheostomy was kept as a backup plan and the trachea intubated videolaryngoscopically utilizing several skilful clinical maneuvers (Shah et al., 2016a; Shah et al., 2016b). We straightened the laser tube before introducing the long narrow stylet that accompanies double-lumen tubes (stylets are not supplied with laser tubes) to prevent damage to rings and facilitate D-blade guided oral intubation.
Since peripheral nerve stimulator guided atracurium was administered intraoperatively, the patient could not have voluntarily swallowed the oral pack (swab count was done before reversal of anesthesia). The possibility of the oral pack being pushed deeper into the esophagus by the FOB is highly unlikely owing to the limp nature of the scope. The pack might have been mistakenly placed partially into the esophagus by the surgeon owing to the obstruction of the line of vision by the massive hemangioma. It might have got pushed deeper by the suction catheter, instrumentation, pulsations of major vessels, and peristaltic movement.
Leaving the throat pack in situ could have caused intestinal obstruction besides possibilities of vomiting, aspiration, laryngospasm, and respiratory obstruction in the immediate postoperative period.
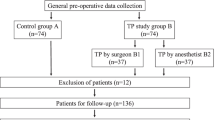
Leaving one end of the throat pack protruding externally, securing the throat pack to the artificial airway device, and sticking a label or mark on the patient’s forehead or ETT are various precautionary measures (Colbert et al., 2012; Knepil & Blackburn, 2008; Tsang et al., 2001). A documentation procedure should be implemented employing a designated person to record the time of insertion and removal of the throat pack on the white board and to include the throat pack in the swab count (Colbert et al., 2012; Knepil & Blackburn, 2008). We propose an algorithm for prevention of retained throat swabs in orofacial surgeries (Fig. 2).
Conclusion
With a massive growth obstructing vision, the throat pack can be misplaced. A high index of suspicion should exist for pack displacement into the esophagus if a thorough videolaryngoscopic scan of the oral cavity is negative. Hence, throat packs should be placed using D-blade. We present a useful algorithm and recommend the use of throat packs with a radio-opaque marking (Raytec gauze) to facilitate their radiographic identification in such rare situations.
Availability of data and materials
Not applicable
Abbreviations
- D-blade:
-
Doerges/difficult airway blade
- MLS:
-
Microlaryngeal surgery
- FOB:
-
Fiberoptic bronchoscope
- PONV:
-
Postoperative nausea vomiting
References
Colbert S, Jackson M, Turner M, Brennan PA (2012) Reducing the risk of retained throat packs after surgery. Br J Or Maxillofacial Surg 50:680–681
Knepil GJ, Blackburn CW (2008) Retained throat packs: results of a national survey and the application of an organisational accident model. Br J Or Maxillofacial Surg 46:473–476
Shah SB, Bhargava AK, Hariharan U, Mittal AK, Goel N, Choudhary M (2016a) A randomized clinical trial comparing the standard mcintosh laryngoscope and the C-mac D blade video laryngoscope™ for double lumen tube insertion for one lung ventilation in Onco surgical patients. Indian J Anaesth 60:312–318
Shah SB, Hariharan U, Bhargava AK. C Mac D blade: Clinical tips and tricks. Trends in Anaesthesia and Critical Care 2016b; 6 :6-10
Tsang WM, Yiu F, Chan M (2001) A missing throat pack. Anaesthesia 56:383–384. To EW
Acknowledgements
None
Conflicts of interest
The authors declare that they have no competing interest.
Funding
None
Author information
Authors and Affiliations
Contributions
SBS planned the anaesthetic technique and preanaesthetic checkup review, performed the videolaryngoscopy and intubation, and did data collection and manuscript drafting and preparation. MB planned the anaesthetic technique, did the photography (data collection), and prepared the manuscript. AKB planning the anaesthetic technique, collected the data, and drafted the manuscript. VB did the preanaesthetic checkup, data collection, and preparation of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
The manuscript contains an individual person’s data, and consent to publish has been obtained from that person.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Shah, S.B., Bhardwaj, M., Bhargava, A.K. et al. Microlaryngeal surgery, difficult airway and a missing throat pack: C Mac D-blade to the rescue!. Ain-Shams J Anesthesiol 12, 7 (2020). https://doi.org/10.1186/s42077-020-00056-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42077-020-00056-z