- Research
- Open access
- Published:
Unveilling the hidden skillset: exploring non-technical skills in surgical education across spanish medical universities
BMC Medical Education volume 24, Article number: 376 (2024)
Abstract
Background
Non-Technical Skills (NTS) are cognitive, social, and personal resource skills that are crucial in complex and high-risk environments. The aims of our research are to determine the prevalence and content of NTS in the surgical rotation teaching guides of the Medicine Degree programs in Spanish Universities, to identify the most prevalent types and subtypes of NTS, and to analyze factors associated with the prevalence of surgical NTS in Medical Schools in Spain.
Methods
Descriptive observational cross-sectional study involving the identification and collection of competencies outlined in the surgical rotation teaching guides of Spanish Medical Schools. Information regarding university performance was obtained from the Foundation for Knowledge and Development Ranking webpage. The “Non-Technical Skills for Surgeons” (NOTSS) system was used to classify each competency in the teaching guides as NTS (categories and elements) and technical skills. Disagreements were resolved through group consensus.
Results
A total of 1,846 competencies were analyzed in surgical rotations of the Medicine Degree programs across 40 Spanish Universities, with 99 competencies identified as surgical NTS, accounting for 5% of the total. The most frequently identified surgical NTS were “Decision Making” (46%), “Communication & Teamwork” (25%), and “Leadership” (19%). Additionally, several NOTSS were not identified in any institution. Public universities and those including a greater number of competencies had a higher rate of surgical NTS competencies, and we did not find a correlation between surgical NTS competencies and quality indices of University Centers.
Conclusions
There is a limited presence of surgical NTS in the educational plans of Spanish Universities.
Background
Surgery stands as a pivotal and essential component of healthcare worldwide. Surgical safety is a global public health priority. In fact, 40–65% of events related to unsafe medical care occur within an operating theatre [1, 5].
The current challenges in surgery (an overall change of the medical model from paternalistic to cooperative, work more focused on the team and less individual, etc.) differ from those of the past, rendering technical skills and manual dexterity alone inadequate to ensure comprehensive quality care [1, 2]. Thus, the concept of Non-Technical Skills (NTS) has been introduced, encompassing cognitive, social, and personal resource skills crucial in complex and high-risk environments. In commercial aviation during the 1980s, once technological advancements mitigated common safety issues, it was realized that the “human factor” was the most frequent cause of aviation accidents. In 1981, United Airlines pilots became the first to receive training in key NTS under the “Crew Resource Management” (CRM) [3].
In 1997, James Reason, a psychologist from the University of Manchester, proposed the “Swiss cheese” model for risk analysis and management within organizations [4]. Presently, up to 60% of surgical adverse events result from NTS deficits [5,6,7]. NTS, categorized into “Situation Awareness,” “Communication & Teamwork,” “Decision Making,” and “Leadership,” are related to emotional intelligence and contribute to safe and efficient surgical performance [8, 9]. A behavioral error in the operating theatre can lead to a serious adverse event. According to Gawande AA et al. [7] and Vioque SM et al. [10], 43% of surgical errors result from communication failures. NTS, both at the individual and team levels, are interrelated and constitute an essential complement to technical skills.
Publications such as “Crisis Management in Anesthesiology” by Gaba D et al. [11], and projects like “MedTeams” [12] and “TeamSTEPPS” [13] developed in the United States, have adapted CRM programs to the field of Medicine. However, it wasn’t until 2004 when Fletcher G et al. introduced an innovative system called “The Anaesthetists Non-Technical Skills” (ANTS), the first behavior marker system for NTS training and assessment, specifically in anaesthesia [14]. Two years later, Yule S et al. created another NTS taxonomy and system named “Non-Technical Skills for Surgeons” (NOTSS) for surgeons [15]. In 2010, Mitchell L et al. developed “Scrub Practitioners’ List of Intraoperative Non-Technical Skills” (SPLINTS) for instrument nurse practitioners [16]. Presently, NOTSS [15] is one of the most evidence-based and validated systems for individual assessment, and “Oxford Non-Technical Skills” (NOTECHS) for team assessment [17].
Nevertheless, little effort has been made to enhance formal training in surgical NTS during undergraduate studies, despite the clear importance of knowledge and implementation for effective surgical team performance. Investment in research and educational innovation by Scientific Societies and Universities is greatly needed in the field of surgery to train competent professionals adapted to new technologies in an ever-changing surgical landscape (robotic surgery, surgical artificial intelligence, etc.). Considering that university education forms the cornerstone of medical training, focusing on the initial step of the surgical education pyramid, medical students, is crucial. Mastery of surgical NTS will allow future physicians to flourish both professionally and personally, as these skills are applicable across all domains of human knowledge.
Currently, there is limited scientific literature concerning the learning of surgical NTS, and in Spain, there is no research evaluating the prevalence, content, or implementation of surgical NTS among medical students. Furthermore, no validated system exists for the periodic assessment of the level of surgical NTS training achieved by future doctors. Hence, the objectives of our research are to determine the prevalence and content of NTS in the teaching guides of surgical rotations within the Medicine Degree programs at Spanish universities, identify the most prevalent types and subtypes of NTS, and analyze the factors related to the prevalence of surgical NTS within our country’s Medical Schools.
Methods
Descriptive Cross-Sectional Observational Study through the identification and compilation of competencies outlined in the surgical rotation teaching guides of Medical Schools in Spain in the year 2022. The inclusion criteria were: Medical Schools located in Spanish territory with a curriculum that includes the subject “Surgical Rotation” and accessible teaching guides via web or email. Among the 49 Medical Schools in Spanish territory, teaching guides for surgery could be identified for 38 through their websites, while emails were sent to the remaining 11 secretariats, resulting in obtaining guides from only 2 institutions. The surgical rotation subject within the Medicine Degree program is included in all Medical Schools in Spain and provides students with the opportunity to apply theoretical concepts learned in the classroom in a real clinical setting. This helps them develop practical skills, gain experience in managing surgical patients, and explore various surgical specialties before making more informed decisions about their future medical careers.
Out of the 40 Medical Schools included in the study, 34 are public and 6 are private. Two categories of school size were considered, categorizing as small (< 200 incoming students) and large (≥ 200 incoming students). Information regarding university performance was obtained from the Foundation for Knowledge and Development Ranking (CYD) [18] website, collecting the following variables for all institutions: teaching and learning area (faculty qualifications, success rate, innovative teaching and assessment methods), research area (publications per faculty member, normalized impact of publications, highly cited publications), knowledge transfer area (private funds), international orientation area (foreign faculty, international publications, international research funds), regional development contribution area (regional publications, regional research funds), and employment rate area (Social Security affiliation rate after one year). High performance was understood as an indicator > 66th percentile, intermediate performance as 33rd ≤ indicator ≤ 66th percentile, and low performance as indicator < 33rd percentile.
The NOTSS [15] system was employed to classify each competency in the teaching guides as NTS (categories and elements) and technical skills (Table 1). Additionally, NOTSS elements were subdivided into three categories (1 item, 2 items, and ≥ 3 items NOTSS out of the total competencies, respectively). A database was designed in Excel (Microsoft) version 19.0 for data recording, where all collected data were archived, and identifying data of participating Medical Schools were protected and encrypted. Competencies were evaluated by a single evaluator who received training and guidance in NTS identification from experts in the NOTSS system at the Royal College of Surgeons of Edinburgh [15]. Disagreements were resolved through group consensus. An intraobserver reliability study was conducted in two periods of the study (first period in August 2022 and second period in October 2022). Intraobserver agreement analysis was assessed using Cohen’s weighted kappa test.
Descriptive analysis presented qualitative variables through frequency distribution of category percentages, while quantitative variables were assessed for normal distribution using the Kolmogorov-Smirnov test, and indicators of central tendency (mean or median) and dispersion (standard deviation or percentiles) were provided. In bivariate analysis, the Pearson’s Chi-Square test was used for qualitative variables, Spearman’s rank correlation for quantitative variables, and Student’s t-test or one-way ANOVA for mean comparison. Statistically significant differences were considered when p-value was less than 0.05. Statistical analysis was conducted using the Statistical Package for Social Sciences (SPSS) program (IBM) version 19.0.
This research was carried out in accordance with the publication standards for observational studies outlined in the STROBE Statement [19].
Results
Among the 40 reviewed Medical Schools, a total of 1,846 competencies were analyzed within the surgical rotation subjects, identifying 99 surgical NTS, which accounts for 5% of the total competencies. Based on the total competencies required as stipulated in the curriculum of the subject (average score/university = 47.5), NTS exhibited an average of 2.3 per university.
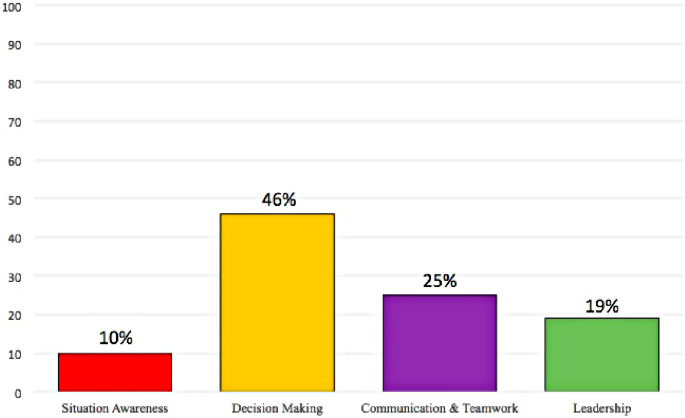
The most frequent NOTSS categories were “Decision Making” (46%), “Communication & Teamwork” (25%), and “Leadership” (19%) (Fig. 1: Distribution of Non-Technical Skills in Surgery in Spanish Universities). Furthermore, several NOTSS were not identified in any institution. Table 2 outlines the prevalence of each NOTSS element.
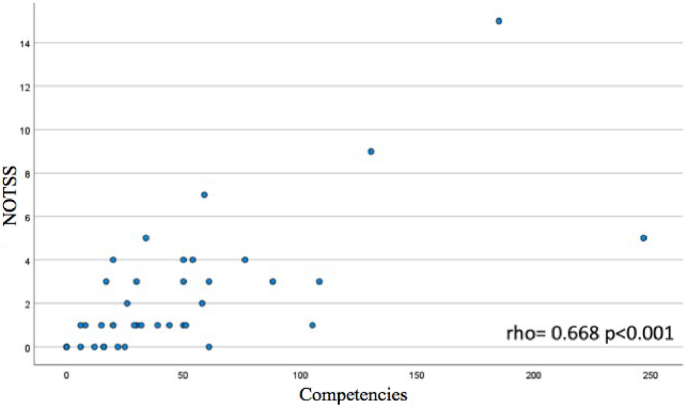
Universities with a higher number of competencies in surgical subjects displayed more NTS in those subjects, showing statistical significance (rho = 0.668, p < 0.001) (Fig. 2: Correlation between total competencies and NOTSS identified in surgical rotations of the Degree in Medicine from Spanish Universities). No significant relationships were found between surgical NTS competencies and other performance indices of the University Centers (Table 3).
Medicine degrees offered by public Universities exhibited an average of 2.6 ± 3 surgical NTS competencies, whereas Medicine degrees offered by private Universities had an average of 0.8 ± 1, with the differences between these types of institutions being statistically significant (p = 0.002).
Regarding the number of students, in terms of university size based on the number of available spots for enrolling in the Medicine Degree program at the institution, no significant differences were found (p = 0.082). However, a slight trend was observed that Universities with ≥ 200 spots had a higher number of NOTSS in their curricula compared to universities with < 200 spots (3.2 ± 4 vs. 1.9 ± 2).
Regarding intraobserver agreement, the kappa index was 0.9 (95% CI 0.8-1.0).
Discussion
The subject of “surgical rotation” within the Medicine Degree pertains to a practical training phase where medical students have the opportunity to rotate through different surgical specialties within a real clinical setting. The objective of this subject is to provide students with direct experience in the field of surgery, allowing them to acquire clinical skills and specific knowledge related to various surgical areas.
The outcomes of our study reveal the limited presence of surgical NTS within these subjects in Spanish Universities, figures that markedly differ from the total competencies that are evaluated to satisfactorily complete practical rotations in surgical specialties before graduation. Lee A et al. have affirmed this fact and underscored the necessity for NTS training during undergraduate studies within Medical Schools in Canada. Spanish Institutions exhibit a higher prevalence of NTS in their surgical rotations and differ in the order of the most prevalent NOTSS categories and elements identified compared to Canadian Institutions [20]. Since comprehensive figures on the prevalence of surgical NTS are not yet available, the trends in other countries remain unclear. What appears evident is that Medical students in both Spain and Canada are not receiving adequate training in surgical NTS, despite the evidence linking NTS to patient safety [21,22,23].
In our study, “Leadership” emerged as one of the least prevalent surgical NTS, with certain elements like “Coping with Pressure” not being identified in any institution. We believe that implementing specific leadership programmes for Medical students from the undergraduate level onwards could enhance the attitude of future professionals in critical situations.
The results of our study depict a greater prevalence of the NTS category “Communication & Teamwork” in surgical specialty rotations compared to other studies, despite communication failures being one of the foremost contributors to surgical errors today [7, 10, 24]. One possible explanation could be the challenge of imparting this skill to medical students.
Factors such as the type of university (public vs. private) have been associated with a higher number of NOTSS in the curricula of Spanish Medical Schools. This data has not been explored previously, and the rationale behind this observation is not straightforward to comprehend. While the observed differences in favour of public Institutions are statistically significant, it should be noted that the vast majority of Centers in Spain are public, and private Universities have a lesser tradition, which could explain these disparities; however, further insights from additional studies are warranted.
Surgical NTS, like any other skill, must be learned and can be honed through training [25,26,27]. Hence, an innovative teaching model is needed to enhance knowledge, interest, and bridge the “Learning Gap” of medical students concerning these matters. In this context, artificial intelligence or the metaverse could be novel and appealing educational tools for the youth due to their cutting-edge technology. Other strategies like case simulation, didactic courses, the GemaSim simulator, mentoring, or role-playing games have been extensively described in scientific literature as effective for acquiring NTS in risk-free environments [28,29,30,31,32].
One of the strengths of this study lies in the fact that the participating researchers possessed prior training in NTS and patient safety before designing the study. Additionally, the registration method assessed the technique and intraobserver variability in recording variables to ensure data reliability. Another strength of this research is that the team consisted of representation from medical students, senior surgeons, and teaching-research staff from the University, thus obtaining perspectives from all stakeholders involved in the medical training process.
Several methodological limitations in our study should be acknowledged. Firstly, the identification of competencies was carried out by a single observer; while we believe that observer training by experts and team resolution of doubts and conflicts have mitigated the potential impact of this limitation. Secondly, the NOTSS [15] system is not validated for application to medical students. However, we consider it a useful tool for the study’s objective. The third limitation stems from evaluating the competencies outlined in the teaching plan, but it doesn’t imply that teaching encompassing these behaviors and attitudes has not been imparted within theoretical or practical teachings of surgical subjects.
The most significant challenges in the future involve assessing the impact of implementing surgical NTS on patient safety-related outcomes and complications, and finally, securing the inclusion of surgical NTS training, refinement, and periodic evaluation as educational priorities by competent authorities and responsible bodies.
Conclusions
Our study examined 1,846 competencies in surgical rotation subjects within the Medicine Degree across 40 Spanish Universities, identifying 99 competencies falling within surgical NTS, which constitutes 5% of the total. The most frequently identified surgical NTS include “Decision Making,” “Communication & Teamwork,” and “Leadership.” Public Universities and those with a higher number of competencies exhibit a higher rate of surgical NTS competencies, and no correlation has been found between surgical NTS competencies and the quality indices of University Centers.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- - NTS:
-
- Non-Technical Skills
- - CRM:
-
- Crew Resource Management
- - ANTS:
-
- Anaesthetists Non-Technical Skills
- - NOTSS:
-
- Non-Technical Skills for Surgeons
- - SPLINTS:
-
- Scrub Practitioners’ List of Intraoperative Non-Technical Skills
- - NOTECHS:
-
- Oxford Non-Technical Skills
- - SPSS:
-
- Statistical Package for Social Sciences
References
McMullan M. Patients using the internet to obtain health information: how this affects the patient–health professional relationship. Patient Educ Couns. 2006;63:24–8. https://doi.org/10.1016/j.pec.2005.10.006.
Mayo WJ. Specialization in surgery. Arch Surg. 1925;10:264. https://doi.org/10.1001/archsurg.1925.01120100276011.
Helmreich RL, Merritt AC, Wilhelm JA. The evolution of Crew Resource Management Training in Commercial Aviation. Int J Aviat Psychol. 1999;9(1):19–32. https://doi.org/10.1207/s15327108ijap0901_2.
Reason JT, Brookfield. Vt., USA: Ashgate; 1997. 252. https://doi.org/10.4324/9781315543543.
de Vries EN, Ramrattan MA, Smorenburg SM, Gouma DJ, Boermeester MA. The incidence and nature of in-hospital adverse events: a systematic review. Qual Saf Health Care. 2008;17:216–23. https://doi.org/10.1136/qshc.2007.023622.
Gillespie BM, Harbeck E, Kang E, Steel C, Fairweather N, Panuwatwanich K, et al. Effects of a brief Team Training Program on Surgical teams’ nontechnical skills: an interrupted time-series study. J Patient Saf. 2021;17:e448–54. https://doi.org/10.1097/PTS.0000000000000361.
Gawande AA, Zinner MJ, Studdert DM, Brennan TA. Analysis of errors reported by surgeons at three teaching hospitals. Surgery. 2003;133:614–21. https://doi.org/10.1067/msy.2003.169.
Flin R, O ́Connor P, Crichton M. Safety at the Sharp end: a guide to non-technical skills. Burlington: Ashgate Publishing Company; 2008.
Yule S, Flin R, Paterson-Brown S, Maran N, Rowley D. Development of a rating system for surgeons’ non-technical skills. Med Educ. 2006;40:1098–104. https://doi.org/10.1111/j.1365-2929.2006.02610.
Vioque SM, Kim PK, McMaster J, Gallagher J, Allen SR, Holena DN, et al. Classifying errors in preventable and potentially preventable trauma deaths: a 9-year review using the Joint Commission’s standardized methodology. Am J Surg. 2014;208:187–94. https://doi.org/10.1016/j.amjsurg.2014.02.006.
Gaba DM, Fish KJ, Howard SK. Crisis management in anesthesiology. New York: Churchill Livingstone; 1994. p. 294.
Risser DT, Rice MM, Salisbury ML, Simon R, Jay GD, Berns SD. The potential for Improved Teamwork to reduce medical errors in the Emergency Department. Ann Emerg Med. 1999;34:373–83. https://doi.org/10.1016/S0196-0644(99)70134-4.
King HB, Battles J, Baker DP, Alonso A, Salas E, Webster J, et al. TeamSTEPPSTM: team strategies and tools to Enhance Performance and Patient Safety. In: Henriksen K, Battles JB, Keyes MA, Grady ML, editors. Advances in Patient Safety: new directions and alternative approaches. Performance and Tools. Volume 3. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008.
Flin R, Glavin R, Maran M, Patey R. Framework for Observing and Rating anaesthetics ́Non-Technical skills-anaesthetists ́Non-Technical skills (ANTS) System Handbook. 1st ed. Aberdeen: UniPrint, University of Aberdeen; 2012.
Yule S, Flin R, Paterson-Brown S, Maran N, Rowley D. The non-technical skills for surgeons (NOTSS) System Handbook. 1st ed. Aberdeen: UniPrint, University of Aberdeen; 2012.
Flin R, O ́Connor P, Crichton M. Scrub practitioners ́List of Intraoperativa non- technical skills (SPLINTS) System Handbook. 1st ed. Aberdeen: UniPrint, University of Aberdeen; 2014.
McMullan RD, Urwin R, Sunderland N, Westbrook J. Observational tools that quantify nontechnical skills in the operating room: a systematic review. J Surg Res. 2020;247:306–22.
Ranking CYD. https://www.rankingcyd.org; 2023 [accessed 26 March 2023].
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335:806–8. https://doi.org/10.1136/bmj.39335.541782.AD.
Lee A, Finstad A, Gawad N, Boet S, Raiche I, Balaa F. Nontechnical skills (NTS) in the Undergraduate Surgical and Anesthesiology Curricula: are we adequately preparing medical students? J Surg Educ. 2021;78:502–11. https://doi.org/10.1016/j.jsurg.2020.08.001.
Mazzocco K, Petitti DB, Fong KT, Bonacum D, Brookey J, Graham S, et al. Surgical team behaviors and patient outcomes. Am J Surg. 2009;197:678–85. https://doi.org/10.1016/j.amjsurg.2008.03.002.
Armour Forse R, Bramble JD, McQuillan R. Team training can improve operating room performance. Surgery. 2011;150:771–8. https://doi.org/10.1016/j.surg.2011.07.076.
Neily J, Mills PD, Young-Xu Y, Carney BT, West P, Berger DH, et al. Association between implementation of a medical team training program and surgical mortality. JAMA. 2010;304:1693–700. https://doi.org/10.1001/jama.2010.1506.
Lingard L, Espin S, Whyte S, Regehr G, Baker GR, Reznick R, et al. Communication failures in the operating room: an observational classification of recurrent types and effects. Qual Saf Health Care. 2004;13:330–4. https://doi.org/10.1136/qshc.2003.008425.
Chang Y, Lai C. Nontechnical skills for the surgery clerkship in the operating room based on adult learning principles in Taiwan. Kaohsiung J Med Sci. 2022;38:907–13. https://doi.org/10.1002/kjm2.12565.
Savoldelli GL, Naik VN, Park J, Joo HS, Chow R, Hamstra SJ. Value of debriefing during simulated Crisis Management. Anesthesiology. 2006;106:279–85. https://doi.org/10.1097/00000542-200608000-00010.
McCulloch P, Mishra A, Handa A, Dale T, Hirst G, Catchpole K. The effects of aviation-style non-technical skills training on technical performance and outcome in the operating theatre. Qual Saf Health Care. 2009;18:109–15. https://doi.org/10.1136/qshc.2009.032177.
Phillips EC, Smith SE, Hamilton AL, Kerins J, Clarke B, Tallentire VR. Assessing medical students’ nontechnical skills using Immersive Simulation: what are the essential components? Simul Healthc J Soc Simul Healthc. 2021;16:98–104. https://doi.org/10.1097/SIH.0000000000000463.
Lateef F. Simulation-based learning: just like the real thing. J Emerg Trauma Shock. 2010;3:348. https://doi.org/10.4103/0974-2700.70743.
Kaiser D, Eberhart J, Butler C et al. Real Time Cockpit Resource Management (CRM) training, 2012. [consultado el 26 de marzo de 2023].
Nicolaides M, Cardillo L, Theodoulou I, Hanrahan J, Tsoulfas G, Athanasiou T, et al. Developing a novel framework for non-technical skills learning strategies for undergraduates: a systematic review. Ann Med Surg. 2018;36:29–40. https://doi.org/10.1016/j.amsu.2018.10.005.
Yule S, Parker SH, Wilkinson J, McKinley A, MacDonald J, Neill A, et al. Coaching non-technical skills improves Surgical residents’ performance in a simulated operating room. J Surg Educ. 2015;72:1124–30. https://doi.org/10.1016/j.jsurg.2015.06.012.
Acknowledgements
Not applicable.
Funding
No sources of funding have been used in these manuscript.
Author information
Authors and Affiliations
Contributions
BOS designed the work, analyzed and interpreted the data and drafted the manuscript. JAGM and VSA designed the work, interpreted the data and revised it JAAA designed the work and revised the manuscript All authors have approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
B, OS., JA, GM., JL, AA. et al. Unveilling the hidden skillset: exploring non-technical skills in surgical education across spanish medical universities. BMC Med Educ 24, 376 (2024). https://doi.org/10.1186/s12909-024-05362-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-024-05362-w