- Research
- Open access
- Published:
The association between ultra-processed food and common pregnancy adverse outcomes: a dose-response systematic review and meta-analysis
BMC Pregnancy and Childbirth volume 24, Article number: 369 (2024)
Abstract
Objectives
Given the increasing incidence of negative outcomes during pregnancy, our research team conducted a dose-response systematic review and meta-analysis to investigate the relationship between ultra-processed foods (UPFs) consumption and common adverse pregnancy outcomes including gestational diabetes mellitus (GDM), preeclampsia (PE), preterm birth (PTB), low birth weight (LBW), and small for gestational age (SGA) infants. UPFs are described as formulations of food substances often modified by chemical processes and then assembled into ready-to-consume hyper-palatable food and drink products using flavors, colors, emulsifiers, and other cosmetic additives. Examples include savory snacks, reconstituted meat products, frozen meals that have already been made, and soft drinks.
Methods
A comprehensive search was performed using the Scopus, PubMed, and Web of Science databases up to December 2023. We pooled relative risk (RR) and 95% confidence intervals (CI) using a random-effects model.
Results
Our analysis (encompassing 54 studies with 552,686 individuals) revealed a significant association between UPFs intake and increased risks of GDM (RR = 1.19; 95% CI: 1.10, 1.27; I2 = 77.5%; p < 0.001; studies = 44; number of participants = 180,824), PE (RR = 1.28; 95% CI: 1.03, 1.59; I2 = 80.0%; p = 0.025; studies = 12; number of participants = 54,955), while no significant relationships were found for PTB, LBW and SGA infants. Importantly, a 100 g increment in UPFs intake was related to a 27% increase in GDM risk (RR = 1.27; 95% CI: 1.07, 1.51; I2 = 81.0%; p = 0.007; studies = 9; number of participants = 39,812). The non-linear dose-response analysis further indicated a positive, non-linear relationship between UPFs intake and GDM risk Pnonlinearity = 0.034, Pdose-response = 0.034), although no such relationship was observed for PE (Pnonlinearity = 0.696, Pdose-response = 0.812).
Conclusion
In summary, both prior to and during pregnancy, chronic and excessive intake of UPFs is associated with an increased risk of GDM and PE. However, further observational studies, particularly among diverse ethnic groups with precise UPFs consumption measurement tools, are imperative for a more comprehensive understanding.
Introduction
The Centers for Disease Control and Prevention’s (CDC’s) 2022 National Center for Health Statistics report alarmingly indicates a persistent rise in pregnancy-related mortality in the US across three decades, highlighting significant disparities in “race” and maternal age [1]. This trend underscores the pivotal role of addressing common pregnancy adverse outcomes as a critical component of maternal morbidity and mortality prevention strategies [2].
Promoting healthy dietary habits during pregnancy is imperative to meet the increased physiological needs of expectant mothers. The phenomenon of “nutritional transition”, characterized by a shift towards high-calorie, low-micronutrient foods, culminates in malnutrition and obesity [3]. The significance of maternal nutrition in prenatal care is heavily emphasized by researchers as a preventive measure against adverse pregnancy outcomes [4]. The consumption of diets rich in refined carbohydrates, fats, and sweets is linked to an increased risk of gestational diabetes mellitus (GDM) and preterm birth (PTB) [5]. Moreover, such dietary patterns adversely affect women’s health by exacerbating hypertensive disorders and contributing to conditions like preeclampsia (PE), low birth weight (LBW), and small-for-gestational-age (SGA) infants [6]. Recognizing the detrimental impact of these unhealthy dietary patterns, it becomes crucial to consider the role of food processing in the maternal diet.
The NOVA classification, a framework for grouping edible substances, categorizes foods into four groups based on the extent and purpose of food processing applied, ranging from unprocessed or minimally processed foods to ultra-processed foods (UPFs) [7, 8]. UPFs are characterized by their high content of additives such as preservatives, artificial flavors, colors, and sweeteners, and are typically devoid of whole or minimally processed ingredients [9]. The consumption of UPFs has been associated with higher risks of obesity, hypertension, cancer, and other chronic diseases [8, 10,11,12]. These foods are implicated in disrupting insulin signaling, promoting excessive energy intake, weight gain, and increased urinary concentrations of phthalate metabolites, which act as endocrine disruptors [13, 14]. In the context of adverse pregnancy outcomes, recent meta-analytic work highlighted a heightened risk of GDM (odds ratio (OR): 1.48; 95% confidence interval (CI): 1.17, 1.87) and PE (OR: 1.28; 95% CI: 1.15, 1.42) among high UPFs consumers, with no significant associations observed in LBW, PTB, and Large for Gestational Age (LGA) [15]. However, the previous meta-analysis did not encompass a comprehensive set of extant studies for each adverse outcome (as evidenced by the inclusion of only 10 studies for GDM in contrast to the 44 studies incorporated in our current investigation), thereby underscoring the challenge posed by the unutilized data in previous analyses. Additionally, recent studies of relevance have emerged [16,17,18] and the preceding meta-analytic work did not include a dose-response analysis [15]. The integration of dose-response analysis offers benefits such as facilitating the formulation of public health directives, augmenting precision, and quantifying the dose-response relationship. Consequently, we decided to conduct an updated dose-response systematic review and meta-analysis to rigorously evaluate the association between UPFs consumption and common adverse pregnancy outcomes, including GDM, SGA, LBW, PTB, and PE.
Methods
This systematic review and meta-analysis was conducted according to the guidelines specified in the 2020 Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [19]. The study protocol was registered with the International Prospective Register of Systematic Reviews Database (PROSPERO) under the registration number CRD42023486135.
Literature search and selection
A systematic literature search was done employing PubMed/MEDLINE, ISI Web of Science and Scopus, with no date restrictions, up to December 6, 2023. The search keywords and strategy are reported in Supplementary Table 1. Data from grey literature sources such as notes, conference abstracts, reviews, case reports, letters, short surveys, and reports were obtained from a manual search of references mentioned in original research articles published in one of these databases. To augment the breadth of research identified, references within reviews and pertinent studies that met eligibility criteria were further subjected to manual examination.
Inclusion and exclusion criteria
Inclusion criteria were defined as follows: a) observational studies (cohort, case-control, or cross-sectional,) in adult subjects (≥18 years) reporting data on the association between UPFs intake and the risk of adverse pregnancy outcomes (including GDM PE, PTB, LBW, and SGA infants), and reporting effect estimates in the form of hazard ratio (HR), relative risk (RR), or odds ratios (OR), each with at least 95% confidence interval (95% CI). Exclusion criteria included: a) studies done in children and adolescents (< 18 years), b) studies without sufficient data (for instance, those failing to report effect sizes or 95% CIs, instead reporting beta coefficients), and c) those with no relevant exposure. Study titles and abstracts, as well as full-text reviews from database searches meeting the inclusion criteria, were assessed by two reviewers (ST and SM). Any disagreements regarding study inclusion/exclusion criteria were resolved by consensus following discussion. The PICOS tool for each article was reported in Supplementary Table 2.
Data extraction
Two investigators (FJ and SM) extracted the following data, based on a standardized extraction form, from the studies that met the inclusion criteria: a) first author’s name, year of publication, and country of origin; b) study characteristics (design, follow-up period, and source of data on health status); c) participant characteristics (number of participants/cases, age and sex); d) methods of evaluating UPFs intake; e) the risk of adverse pregnancy outcomes; f) main study results (outcomes), and g) covariates utilized for adjustments in multivariate analyses. Any disagreement regarding data extraction characteristics was decided by consensus following the discussion.
Quality assessment
Applying the Newcastle-Ottawa Scale (NOS) [20], two investigators assessed the quality of each shortlisted study. The NOS was specifically chosen due to its comprehensive framework designed to evaluate the quality of non-randomized studies. This scale excels in its design, content, and user-friendliness, making it particularly suitable for integrating quality assessments into the interpretation of meta-analytic results. The NOS scale for systematic reviews or meta-analyses, allocating up to 9 points across three domains: study group selection (four points), study group comparability (two points), and exposure and outcomes ascertainment for case-control or cohort studies (three points). Studies scoring 7–9 are deemed high quality/low risk of bias, whereas a score of 0–3 indicates a high risk of bias. Table 1 shows the consensus from this assessment.
Statistical analyses and data synthesis
Statistical analyses were performed applying STATA version 14.0 (StataCorp, College Station, TX, USA) and SPSS version 25.0 (IBM, Armonk, NY, USA). The RR and 95% CI were established as overall effect sizes in this work, similar to effect estimates reported in observational articles meeting the inclusion criteria for this meta-analysis [21]. The synthesized effect estimates were reported as pooled RR with 95% CI. Due to anticipated heterogeneity between studies, effect estimates were calculated using the DerSimonian-Laird weighted random-effects model [22]. A pairwise meta-analysis combined the effect size results for the highest and lowest categories of UPFs intake. Heterogeneity among the articles was examined by the Cochran Q and I-squared (I2) statistics, with the I2 value estimated from [(Q-df)/Q × 100%]; where Q is the χ2 value and df the corresponding degrees of freedom. Between-study heterogeneity was considered significant when the Cochran Q statistic was significant (p < 0.05) or if I2 > 50%; specifically, low, moderate, high, and extreme heterogeneity was defined based on the I2 statistics cut-offs of < 25%, 25–50%, 50–75%, and >75%, respectively.
Furthermore, subgroup analyses were conducted to evaluate any potential effects due to the study design (cross-sectional, case-control, or cohort), UPFs classification method (NOVA food classification, Western-type diet pattern, fast-food, or sweets consumption), the study region of origin (North America, South America, Asia, Europe, and Australia), pre-pregnancy body mass index (< 25 kg/m2 and ≥ 25 kg/m2) [23, 24], age (< 30 years and ≥ 30 years) [24], number of cases (< 100 or ≥ 100), number of participants (< 1000 or ≥ 1000), dietary assessment method (food frequency questionnaires [FFQ], 24 h recall, or food records), dietary assessment period (pre-pregnancy, early pregnancy, mid-pregnancy), and other covariate adjustments. Sensitivity analysis was conducted by omitting each study and evaluating the remaining pooled effect estimates. Publication bias was evaluated by visual inspection of funnel plots, and formal testing using Egger’s regression asymmetry and Begg’s rank correlation tests [25, 26], with outcomes considered as significant at p < 0.05.
A dose-response meta-analysis was completed to estimate the RRs per 100 g increment in UPFs intake, based on the method introduced by Greenland and colleagues [27, 28]. For this process, studies needed to report the number of cases (i.e., participants with incidence) and non-cases (i.e., participants without incidence) or person-years (i.e., the number of people in the study and the duration of their participation) as well as the median point of UPFs intake across more than three categories of intake. Ultimately, a one-stage linear mixed-effects meta-analysis was undertaken to model the dose-response associations, estimating and combining study-specific slope lines to obtain an average slope in a single stage. This linear mixed-effects meta-analysis includes studies with two categories of exposures (at least two effect sizes) in the dose-response analysis.
Quality of evidence
The quality of evidence across articles was ranked employing the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) working group guidelines. The GRADE criteria categorize evidence quality into high, moderate, low, or very low levels [29].
Results
Study characteristics
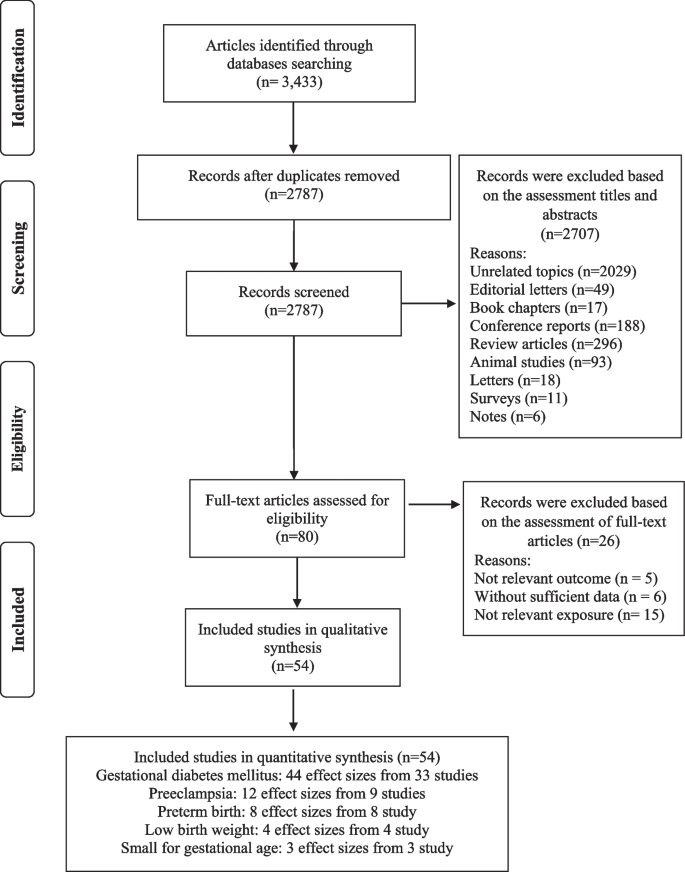
Our systematic search and examination of reference lists yielded a total of 3433 records. After omitting duplicates, 2787 articles remained for assessment (Fig. 1). A title and abstract review led to the removal of 2707 articles. Subsequent full-text assessment of the 80 remaining studies resulted in the exclusion of a further 26 articles for the following reasons: five articles reported outcomes not relevant to our research scope, six lacked sufficient data, and 15 did not focus on relevant exposure (Supplemental Table 3). Consequently, 54 studies met our inclusion criteria and were selected in the present meta-analysis [16,17,18, 30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79].
The selected studies (detailed in Supplemental Table 4) encompass 38 cohort studies [16, 31, 33,34,35,36,37, 39, 40, 42,43,44,45,46,47,48,49, 51, 52, 54, 55, 57,58,59,60,61,62, 65,66,67, 69,70,71, 73,74,75, 78], 11 case-control studies [17, 18, 30, 32, 34, 50, 63, 66, 68, 72, 77], and five cross-sectional studies [38, 46, 64, 76, 79]. These articles, conducted between 1988 and 2023, originated from different countries including the USA [33, 36, 53, 58, 60, 62, 69, 74, 78], the UK [16], China [43, 49, 51, 71, 73], Brazil [31, 59, 63, 64, 68, 79], Spain [39, 40, 42, 55, 57], Iran [17, 18, 30, 32, 48, 54, 66, 76, 77], Malaysia [75], Palestine [72], Australia [45, 46, 65], Singapore [37, 38], Norway [35, 44, 47], Japan [41, 67], Czech Republic [34], Iceland [70] and Denmark [61]. The study-specific, maximally adjusted RR was reported for 552,686 individuals across the included articles and was pooled for meta-analysis to assess the association between UPFs and the risk GDM [16, 32,33,34, 36, 38,39,40,41, 43, 48,49,50,51, 53,54,55,56, 59, 60, 64,65,66, 70,71,72,73,74,75, 77,78,79], PE [17, 18, 30, 35, 48, 52, 62, 69, 74, 76], PTB [31, 37, 44,45,46, 48, 52, 58, 61, 67], LBW [45, 63, 67] and SGA infants [46, 67, 68]. The Newcastle-Ottawa grade (used for quality assessment) categorized 27 studies as high quality [17, 33, 35,36,37, 39,40,41,42,43,44,45, 47, 51, 53, 55, 57, 58, 60, 62, 65, 67, 69, 74, 75, 78] and 27 as medium quality [16, 18, 30,31,32, 34, 38, 46, 48,49,50, 52, 54, 56, 59, 61, 63, 64, 66, 68, 70,71,72,73, 76, 77, 79]. Moreover, the outcomes revealed that the level of agreement between investigators for data collection as well as for quality assessment was appropriate (Kappa = 0.897).
Ultra-processed food and common adverse pregnancy outcomes
Our results suggested a significant relationship between higher UPF intake and an increased risk of GDM (RR = 1.19; 95% CI: 1.10, 1.27; I2 = 77.5%; p < 0.001; n = 44), PE (RR = 1.28; 95% CI: 1.03, 1.59; I2 = 80.0%; p = 0.025; n = 12), but not PTB (RR = 1.06; 95% CI: 0.97, 1.17; I2 = 34.2%; p = 0.231; n = 8), LBW (RR = 1.01; 95% CI: 0.91, 1.12; I2 = 52.2%; p = 0.905; n = 4) and SGA infants (RR = 1.11; 95% CI: 0.81, 1.52; I2 = 66.3%; p = 0.532; n = 3), (Refer to Table 1, Supplementary Fig. 1).
In the context of GDM, subgroup analysis showed that a greater UPFs intake was significantly associated with an enhanced risk in cohort studies (vs. cross-sectional) (RR = 1.18; 95% CI: 1.09, 1.27; I2 = 79.3%; p < 0.001; n = 31) and case-control studies (RR = 2.06; 95% CI: 1.31, 3.35; I2 = 77.7%; p = 0.002; n = 10), particularly in studies assessed western dietary pattern (RR = 1.34; 95% CI: 1.01, 1.76; I2 = 43.0%; p = 0.040; n = 7) or fast-foods (RR = 1.32; 95% CI: 1.15, 1.51; I2 = 79.3%; p < 0.001; n = 22), (vs. NOVA classification or sweets consumption), in North America (vs. Europe, South America, Asia and Australia) (RR = 1.43; 95% CI: 1.27, 1.53; I2 = 45.4%; p < 0.001; n = 10), and across studies with > 100 number of case (RR = 1.38; 95% CI: 1.21, 1.58; I2 = 74.8%; p < 0.001; n = 12)(vs. < 100 number of case), in studies with > 1000 number of participants (RR = 1.33; 95% CI: 1.15, 1.54; I2 = 76.9%; p < 0.001; n = 21)(vs. < 1000 number of participants), in studies used FFQ for dietary assessment (RR = 1.27; 95% CI: 1.14, 1.43; I2 = 78.6%; p < 0.001; n = 34) (vs. 24 h recall or food record), particularly in studies where the period of dietary assessment was at early pregnancy (RR = 1.26; 95% CI: 1.09, 1.46; I2 = 80.5%; p = 0.002; n = 19) (vs. pre-pregnancy or mid-pregnancy). Moreover, subgroup analysis for covariates adjustment showed that BMI and physical activity may influence the association between UPF intake and the risk of GDM (Table 2).
For PE, the subgroup analysis also highlighted that greater UPFs intake was significantly associated with an enhanced risk in studies assessed western dietary pattern (RR = 2.51; 95% CI: 1.13, 5.57; I2 = 91.1%; p = 0.023; n = 3) or NOVA classification (RR = 1.22; 95% CI: 1.04, 1.42; I2 = 0.0%; p = 0.013; n = 3), (vs. sweets consumption), in Asia (vs. Europe or US areas) (RR = 1.65; 95% CI: 1.07, 2.55; I2 = 86.1%; p < 0.001; n = 6), and across studies with > 100 number of case (RR = 1.57; 95% CI: 1.03, 2.40; I2 = 93.2%; p < 0.001; n = 4)(vs. < 100 number of case), in studies with number of < 1000 participants (RR = 1.65; 95% CI: 1.07, 2.55; I2 = 86.1%; p = 0.023; n = 6)(vs. > 1000 number of participants), in participants aged ≥30 years (RR = 1.28; 95% CI: 1.07, 1.54; I2 = 50.4%; p = 0.089; n = 5)(vs. participants aged < 30 years), in participants with pre-pregnancy-BMI > 25 (RR = 1.52; 95% CI: 1.07, 2.15; I2 = 84.7%; p = 0.021; n = 1)(vs. participants with pre-pregnancy-BMI ≤ 25), in studies used FFQ for dietary assessment (RR = 1.38; 95% CI: 1.10, 1.72; I2 = 82.6%; p = 0.005; n = 10) (vs. questions), and particularly in studies where the period of dietary assessment was at mid-pregnancy (RR = 1.23; 95% CI: 1.05, 1.43; I2 = 38.8%; p = 0.009; n = 3) (vs. early pregnancy). Furthermore, subgroup analysis for covariates adjustment showed that BMI and physical activity may influence the association between UPF intake and the risk of PE (Table 3).
Linear and non-linear dose-response analysis
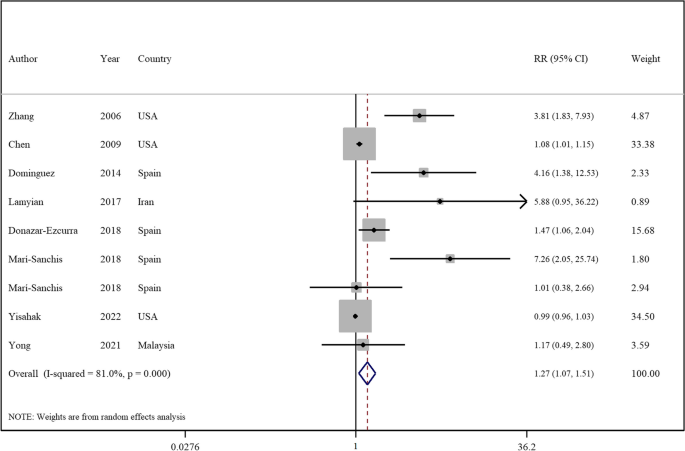
The linear dose-response analysis (refer to Table 1 and Fig. 2) indicates a 27% increase in GDM risk per 100 g increment in UPF intake RR = 1.27; 95% CI: 1.07, 1.51; I2 = 81.0%; p = 0.007; n = 9). However, the linear dose-response analysis for other outcomes was not undertaken due to the limited number of studies available.
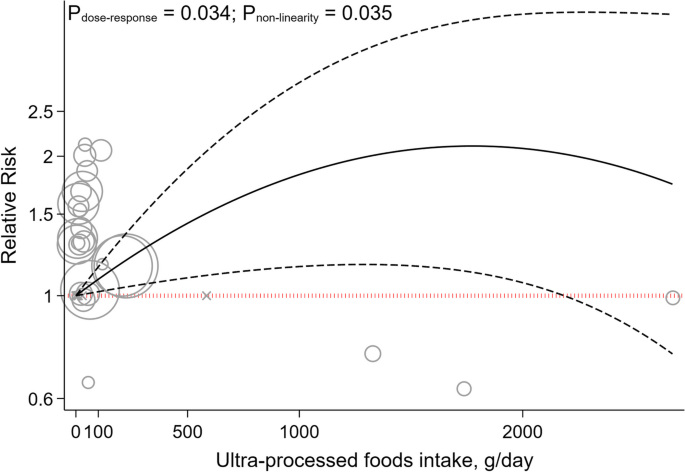
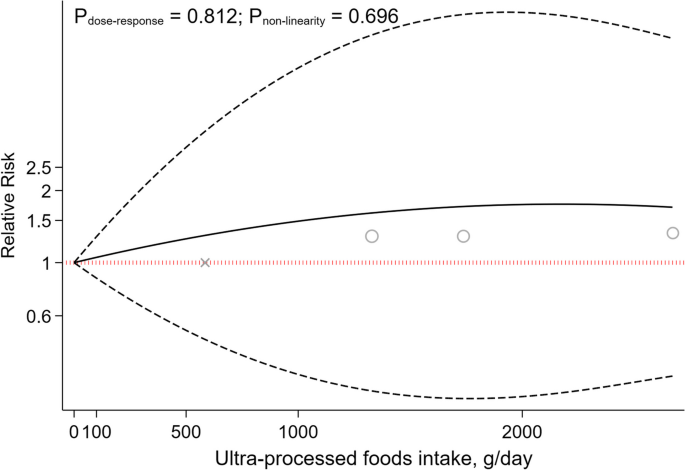
The non-linear dose-response analysis revealed a positive non-linear relationship between UPFs intake and GDM risk (Pnonlinearity = 0.034, Pdose-response = 0.034, Fig. 3), but not for PE (Pnonlinearity = 0.696, Pdose-response = 0.812, Fig. 4). The non-linear dose-response analysis was not conducted for other outcomes due to insufficient studies.
Sensitivity analyses and publication bias
Sensitivity analysis across the highest to the lowest meta-analysis for GDM, PE, PTB, LBW and SGA infants showed no significant influence of any single study (Supplemental Fig. 2).
No evidence of publication bias was found in articles related to the association with an increased risk of PE (p = 0.529, Egger’s test; p = 0.891, Begg’s), PTB (p = 0.458, Egger’s test; p = 0.473, Begg’s), LBW (p = 0.905, Egger’s test; p = 1.00, Begg’s test), and SGA infants (p = 0.348, Egger’s test; p = 1.00, Begg’s test). Although, for GDM, Egger’s test indicated potential publication bias (p < 0.001), not corroborated by Begg’s test (p = 0.241). As illustrated in Supplemental Fig. 3, the funnel plot was symmetrical for the association between the UPFs intake and all outcomes, except for studies that reported the risk of GDM disease.
Quality of evidence
Utilizing the GRADE scale for quality evaluation, we detected the evidence for associations between UPFs intake and risk of GDM, PE, PTB, LBW and SGA infants was classified as moderate (Refer to Table 1).
Discussion
In the realm of maternal and fetal health, the quality of dietary intake during pregnancy is of paramount significance. Accumulating evidence suggests a correlation between the consumption of UPFs and the deterioration of diet quality, potentially elevating the risk of various health complications [80,81,82]. This systematic review and meta-analysis aimed to elucidate the relationship between UPFs intake and adverse pregnancy outcomes including GDM, SGA, LBW, PTB, and PE, through an integrative analysis of existing studies. Our outcomes indicate a significant association between UPFs consumption and increased risks of PE, and GDM either prior to or during pregnancy. However, no significant association was found between UPFs intake and the risks of LBW, SGA, and PTB. Importantly, a 27% increment in the incidence of GDM was linked to a 100 g increase in UPF intake. Furthermore, a positive, non-linear relationship between UPF intake and GDM risk was identified through non-linear dose-response analysis, albeit no analogous association was found for PE.
The results of the current work showed a positive association between UPFs consumption and the risk of PE. In addition, subgroup analysis revealed this relationship to be more pronounced in studies using the NOVA-food classification and a Western dietary pattern for UPFs intake assessment, compared to those focusing on sweet intake. The NOVA classification categorizes foods based on the extent of processing, encompassing various UPFs. Moreover, the association between UPFs consumption and the risk of PE was significant in studies conducted in Asia (vs other regions). Prevalence of PE varies globally, ranging from 0.2–6.7% in Asia, 2.8–9.2% in Oceania, 2.8–5.2% in Europe, 2.6–4.0% in North America, and 1.8–7.7% in South America and the Caribbean [83]. However, the high heterogeneity in Asian studies should be noted when interpreting this result. Furthermore, a significant association was observed in studies involving women aged 30 years or older, aligning with the increased PE risk associated with advanced maternal age [84]. Additionally, a significant association was identified between PE risk and UPFs intake in women with pre-pregnancy BMI higher than 25 kg/m2 (vs BMI ≤25). This aligns with previous findings linking excessive weight gain in expectant mothers to an elevated PE risk, with overweight and obese mothers facing substantially higher risks [85].
The association between UPFs intake and PE can be elucidated through several mechanisms. The risk factors for PE, including GDM, maternal obesity, and advanced maternal age, are extensively documented in the literature [84,85,86]. It has been established that adopting healthy lifestyle habits (including dietary patterns) can mitigate these risk factors [87]. A higher intake of UPFs is associated with a diminished dietary quality, marked by an increased consumption of sugars and fats, alongside a decrease in fiber, protein, vitamins, and minerals [88, 89]. UPFs are known to contain elevated levels of pro-inflammatory agents such as refined sugars, salt, and trans fats. The ingestion of these inflammatory components can precipitate oxidative stress and systemic inflammation [90,91,92], which are implicated in the pathogenesis of preeclampsia [93, 94]. Additionally, the presence of trans fatty acids, added phosphates, and a high salt content in UPFs may impair endothelial function [95,96,97], a critical factor in the pathophysiology of hypertension observed in preeclampsia [98]. Furthermore, the intake of UPFs can alter the composition and diversity of the gut microbiota [99]. Studies have shown that food additives commonly found in UPFs, such as emulsifiers, sweeteners, and colorants, adversely affect the gut flora [100]. The interplay between the gut microbiota and the placenta, referred to as the “gut–placenta” axis, is crucial for understanding the etiology of PE. Dysbiosis of the gut microbiota and bacterial products like lipopolysaccharide (LPS) have been identified as promotive of PE [101, 102]. According to Kell et al., microbial infection, particularly through bacterial products such as LPS (also known as endotoxin), which is highly inflammatory, can initiate an innate immune response that exacerbates inflammation [103]. Hence, it is hypothesized that dysbiosis induced by UPFs consumption may play a significant role in the promotion of preeclampsia. Moreover, UPFs intake is positively associated with a risk of obesity [104], a condition marked by insulin resistance and hyperinsulinemia, crucial factors in PE development [105]. Pregnant women with obesity and PE exhibit higher leptin levels, correlating with increased Tumor Necrosis Factor-Alfa (TNF-α), Interleukin 6 (IL-6), and C-reactive protein concentrations [106, 107]. Additionally, excessive adipose tissue near the reproductive tract is the source of increased complement components and fragments in preeclamptic pregnancies. These complement proteins may promote an imbalance in angiogenic factors (characterized by increased production of antiangiogenic factors and a decrease in proangiogenic factors). This imbalance leads to placental injury, resulting in decreased blood flow to the tissue, and is accompanied by changes in cytokines levels (decreased IL-10 and increased TNF-α) before the onset of PE [108].
Our pooled analysis also revealed that higher UPFs intake was related to an increased risk of GDM. This association was significant in studies employing cohort and case-control designs (as opposed to those with cross-sectional methodologies). The inherent recall bias in cross-sectional studies that rely on self-reporting, is a notable limitation affecting the reliability of outcomes [109]. Moreover, this association was more pronounced in studies that used Western dietary patterns and fast-food consumption for the assessment of UPFs intake (vs those employing NOVA food classification and sweet consumption metrics). The concept of a dietary pattern, which represents the aggregate of eating and drinking habits, is critical as it exerts a greater impact on health and chronic diseases than any individual food item [110]. Additionally, the application of the NOVA food classification in existing studies is less frequent, suggesting the need for further research utilizing this methodology to derive more meaningful results. Geographical variations were also evident, with significant associations observed in studies conducted in America, compared to those in Asia and Europe. This is in context with the differing regional prevalences of GDM: 7.1% in North America and the Caribbean, 7.8% in Europe and 20.8% in South-East Asia [111]. Despite the higher prevalence of GDM in Asian populations, the greater intake of UPFs in American and European cohorts may have influenced the study outcomes [112,113,114,115]. Additionally, a positive association between UPFs intake and GDM risk was observed in studies focusing on women with a pre-pregnancy BMI > 25. Previous research indicates that being overweight or obese before and during pregnancy is a significant risk factor for GDM [116,117,118]. However, the scarcity of studies in women with pre-pregnancy BMI > 25 kg/m2kg/m suggests the need for more research in this demographic for robust conclusions.
Our outcomes also indicated that a 100 g increase in UPF intake was associated with a 27% increase in the risk of GDM. Moreover, the non-linear dose-response analysis similarly showed a positive, non-linear association between the consumption of UPFs and the risk of GDM. These findings underscore the significant impact that UPF consumption can have on GDM risk. The evidence points towards a robust and worrying correlation where even moderate increases in UPF intake can precipitate a marked rise in GDM risk, highlighting the critical need for dietary awareness and intervention among pregnant women. This aligns with broader nutritional science, emphasizing the importance of minimizing UPF consumption to mitigate not only GDM risk but potentially other metabolic disorders as well, given the multitude of adverse mechanisms through which UPFs affect glucose metabolism and insulin sensitivity.
Pathophysiologically, UPFs intake may increase GDM risk through several mechanisms. In pregnant women with GDM, pre-pregnancy reduced insulin sensitivity and β-cell dysfunction lead to hyperglycemia [119, 120]. The hypothesis that excessive sugar intake may augment body mass, thereby indirectly precipitating insulin resistance and subsequent diabetes, is widely recognized. Moreover, the liver’s capacity to assimilate and metabolize refined sugars prevalent in UPFs (such as fructose and sucrose) may be compromised, leading to augmented fat deposition and deteriorated insulin sensitivity [121]. Furthermore, insulin resistance may be induced by cosmetic ingredients present in UPFs. For example, dietary additives like carrageenan, employed as a thickening and stabilizing agent, may interfere with insulin signaling and thus foster insulin resistance [122]. Additionally, UPFs intake correlates with increased production of reactive oxygen species and inflammatory biomarkers [123], inducing insulin resistance through molecular pathways such as β-cell and mitochondrial dysfunction, decreased GLUT4 expression, impaired insulin signaling and heightened inflammatory responses [124]. Furthermore, UPFs often contain packaging materials like phthalates and bisphenol A, known to have endocrine disruption properties that may contribute to insulin resistance and diabetes development [125, 126]. The ingestion of substantial quantities of UPFs also elevates inflammation, a pivotal factor in the genesis of insulin resistance, culminating in hyperglycemia and the development of GDM [127]. A diet replete with saturated fats, trans fats, sugars, and salt, characteristic of high UPFs consumption, may contribute to chronic inflammation [128]. Furthermore, excessive UPFs consumption may supplant essential components of a balanced and nutritious diet. For instance, fruits and vegetables are associated with an anti-inflammatory effect [129]. In addition, the leaching of chemicals from food packaging into UPFs could introduce non-nutritional elements such as phthalates or bisphenol A, potentially eliciting an inflammatory response [130].
The present study did not establish a significant association between UPFs consumption and the risk of LBW. This result may be attributable to several factors. Firstly, a limited number of studies have evaluated the association between UPFs intake and LBW risk. Additionally, the intake of high-sugar foods (such as sugar-sweetened beverages) has been correlated with an increased risk of LBW in non-GDM subjects [34, 40]. This could be attributed to impaired fetal nutrition due to reduced vascular function, potentially induced by oxidative stress, inflammation, and endothelial dysfunction associated with high sugar consumption [131]. However, in GDM subjects this association may not be found due to the higher glucose loads in the fetus [47]. Therefore, additional research is warranted in both GDM and non-GDM populations to elucidate these relationships comprehensively.
Moreover, SGA was not associated with the intake of UPFs according to the pooled analysis of conducted studies. Although additional studies are necessary to explore this relationship further, existing evidence suggests that a fast-food dietary pattern may lead to increased fat intake and a reduced intake of essential micronutrients crucial for fetal development [132]. Maternal UPFs intake is linked to lower protein intake, reduced overall nutrition quality, and higher intake of trans fats, carbohydrates and saturated fats, which may increase the risk of neonatal adiposity [133,134,135]. Furthermore, higher fast-food intake during pregnancy has been linked with an elevated risk of maternal obesity, which in turn, may increase the likelihood of LGA babies [132, 136].
Regarding PTB, the current study found no association with UPFs consumption. Previous research has indicated that dietary patterns rich in fruits and vegetables are associated with a lower risk of PTB [37, 45]. Inadequate nutrition before and during pregnancy can lead to health issues for both the mother and fetus, increasing the risk of preterm delivery and intrauterine growth retardation [137]. The absence of an association between UPFs consumption and preterm delivery in this study could be due to various factors, including the need for a higher UPFs consumption threshold during pregnancy to manifest negative impacts on preterm birth. Additionally, the varied diet of pregnant women, typically including beneficial foods such as fruits, vegetables and nuts, may mitigate the adverse effects of UPFs.
The current investigation has several crucial strengths that make its findings highly significant. Firstly, by pooling all available observational data on the topic, the study provides a comprehensive and robust analysis of the relationship between UPFs intake and adverse pregnancy outcomes. Secondly, the study’s use of a dose-response analysis adds further weight to its conclusions and bolsters our understanding of the link between these two factors. However, there are limitations to consider. These include potential information and recall biases due to the self-reported nature of dietary intake assessments (such as the FFQ) and the absence of specific dietary tools for assessing UPFs consumption. Additionally, this meta-analysis included studies that did not use NOVA’s specialized dietary assessments. Moreover, dietary changes following pregnancy discovery could affect results, and the observational nature of the included studies precludes causal inference. Despite the inclusion of numerous confounding variables, several factors must be cautiously considered in the interpretation of the research findings. For instance, the socio-economic status of participants influences their dietary habits, while race and ethnicity may affect pregnancy outcomes. Furthermore, disparities in access to healthcare services can impact dietary choices and pregnancy outcomes. Other health statuses, such as mental health conditions among pregnant subjects, also influence dietary selections and pregnancy results [138, 139]. Finally, the availability of data on broader categories such as diabetes in pregnancy and hypertensive disorders was limited, hindering our ability to conduct a comprehensive analysis on these broader categories.
Conclusion
Our outcomes indicate that prior to or during pregnancy, UPFs intake is associated with a higher risk of GDM and PE. However, no significant link tying UPFs intake to SGA, LWB and PTB was established. Importantly, a 100 g increment in UPFs intake was related to a 27% increase in GDM risk. This study aligns with global trends, where a rise in adverse pregnancy outcomes seems to align with the escalation of industrialization and the corresponding surge in UPFs production and consumption. Investigating the potential linkage between UPFs intake and the rise of adverse pregnancy outcomes may help in the development of nutrition-centric policies for expecting mothers and promote more health-conscious decision-making. To further substantiate these findings, extensive empirical research is required. Future studies should encompass observational research across diverse ethnic groups. Moreover, the adoption of more precise tools for measuring UPFs consumption is imperative. In observational research, it may be challenging to ascertain whether the consumption of UPFs directly contributes to adverse pregnancy outcomes or if it serves as an indicator of other underlying factors. Components of UPFs may escalate the risk of negative pregnancy outcomes. Moreover, UPF consumption could be part of a complex interplay affecting other variables that directly result in adverse outcomes. For instance, UPF intake could influence gestational weight gain, potentially leading to insulin resistance, which is known to correlate with unfavorable pregnancy outcomes, including GDM. Additionally, the consumption of UPFs may not only diminish dietary quality but also be linked with various lifestyle and dietary factors, such as poor diet quality, thereby increasing the risk of adverse pregnancy outcomes [140]. The bidirectional correlation between UPF consumption and unfavorable pregnancy outcomes also merits consideration. For example, individuals experiencing depression or other health conditions might alter their dietary patterns to include a higher intake of UPFs [138]. Evaluating changes in UPF consumption over time, utilizing precise questionnaires that assess food items classified as UPFs according to the NOVA food classification system, and their association with other health outcomes affecting pregnancy, such as obesity, could offer insights into this relationship. Considering these approaches is essential to enhance the depth and accuracy of investigations into the potential association between UPFs intake and the incidence of adverse pregnancy outcomes.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due but are available from the corresponding author on reasonable request.
References
Hoyert DL, Miniño AM. Maternal Mortality in the United States: Changes in Coding, Publication, and Data Release, 2018. Natl Vital Stat Rep. 2020;69(2):1–18.
Parikh NI, Gonzalez JM, Anderson CA, Judd SE, Rexrode KM, Hlatky MA, et al. Adverse pregnancy outcomes and cardiovascular disease risk: unique opportunities for cardiovascular disease prevention in women: a scientific statement from the American Heart Association. Circulation. 2021;143(18):e902–e16.
Hashmi AH, Solomon N, Lee SJ, Min AM, Gilder ME, Wiladphaingern J, et al. Nutrition in transition: historical cohort analysis summarising trends in under-and over-nutrition among pregnant women in a marginalised population along the Thailand–Myanmar border from 1986 to 2016. Br J Nutr. 2019;121(12):1413–23.
Lind JM, Hennessy A, McLean M. Cardiovascular disease in women: the significance of hypertension and gestational diabetes during pregnancy. Curr Opin Cardiol. 2014;29(5):447–53.
Englund-Ögge L, Birgisdottir BE, Sengpiel V, Brantsæter AL, Haugen M, Myhre R, et al. Meal frequency patterns and glycemic properties of maternal diet in relation to preterm delivery: results from a large prospective cohort study. PLoS One. 2017;12(3):e0172896.
Mekie M, Mekonnen W, Assegid M. Cohabitation duration, obstetric, behavioral and nutritional factors predict preeclampsia among nulliparous women in West Amhara zones of Ethiopia: age matched case control study. PLoS One. 2020;15(1):e0228127.
Monteiro CA, Cannon G, Levy R, Moubarac J-C, Jaime P, Martins AP, et al. NOVA The star shines bright. World Nutrition. 2016;7(1–3):28–38.
da Costa Louzada ML, Baraldi LG, Steele EM, Martins APB, Canella DS, Moubarac J-C, et al. Consumption of ultra-processed foods and obesity in Brazilian adolescents and adults. Prev Med. 2015;81:9–15.
Monteiro CA, Levy RB, Claro RM, Castro IRR, Cannon G. A new classification of foods based on the extent and purpose of their processing. Cadernos de saude publica. 2010;26:2039–49.
Mendonça RD, Pimenta AM, Gea A, de la Fuente-Arrillaga C, Martinez-Gonzalez MA, Lopes ACS, et al. Ultraprocessed food consumption and risk of overweight and obesity: the University of Navarra Follow-up (SUN) cohort study. Am J Clin Nutr. 2016;104(5):1433–40.
Mendonça RD, Lopes ACS, Pimenta AM, Gea A, Martinez-Gonzalez MA, Bes-Rastrollo M. Ultra-processed food consumption and the incidence of hypertension in a Mediterranean cohort: the Seguimiento Universidad de Navarra project. Am J Hypertens. 2017;30(4):358–66.
Fiolet T, Srour B, Sellem L, Kesse-Guyot E, Allès B, Méjean C, Deschasaux M, Fassier P, Latino-Martel P, Beslay M, Hercberg S, Lavalette C, Monteiro CA, Julia C, Touvier M. Consumption of ultra-processed foods and cancer risk: results from NutriNet-Santé prospective cohort. BMJ. 2018;360:k322. https://doi.org/10.1136/bmj.k322.
Bhattacharyya S, Feferman L, Tobacman JK. Carrageenan inhibits insulin signaling through GRB10-mediated decrease in Tyr (P)-IRS1 and through inflammation-induced increase in Ser (P) 307-IRS1. J Biol Chem. 2015;290(17):10764–74.
Buckley JP, Kim H, Wong E, Rebholz CM. Ultra-processed food consumption and exposure to phthalates and bisphenols in the US National Health and nutrition examination survey, 2013–2014. Environ Int. 2019;131:105057.
Paula WO, Patriota ES, Gonçalves VS, Pizato N. Maternal consumption of ultra-processed foods-rich diet and perinatal outcomes: a systematic review and meta-analysis. Nutrients. 2022;14(15):3242.
Mahendra A, Kehoe SH, Kumaran K, Krishnaveni GV, Arun N, Pidaparthy P, et al. Periconceptional diet and the risk of gestational diabetes in south Indian women: findings from the BAngalore nutrition gestational diabetes LiFEstyle study (BANGLES). Lancet Glob Health. 2023;11:S4.
Kooshki A, Sovizi B, Mahmoudi R, Ghezi S, Foroumandi E. The association between food groups and preeclampsia: a case-control study. Hyperten Pregnancy. 2022;41(1):64–9.
Moradi M, Niazi A, Selajgeh F, Mazloumi E. Comparing dietary patterns during pregnancy in women with preeclampsia and healthy women: a case-control study. J Midwife Reproduct Health. 2022;10(1)
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Oxford: Ottawa Hospital Research Institute; 2000.
Symons M, Moore D. Hazard rate ratio and prospective epidemiological studies. J Clin Epidemiol. 2002;55(9):893–9.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Jayedi A, Soltani S, Zargar MS, Khan TA, Shab-Bidar SJB. Central fatness and risk of all cause mortality: systematic review and dose-response meta-analysis of 72 prospective cohort studies. 2020;370.
Song C, Lyu Y, Li C, Liu P, Li J, Ma R, et al. Long-term risk of diabetes in women at varying durations after gestational diabetes: a systematic review and meta-analysis with more than 2 million women 2018;19(3):421–9.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–101.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ (Clin res ed). 1997;315(7109):629–34.
Berlin JA, Longnecker MP, Greenland S. Meta-analysis of epidemiologic dose-response data. Epidemiology. 1993;4(3):218–28. https://doi.org/10.1097/00001648-199305000-00005.
Orsini N, Bellocco R, Greenland SJTsj. Generalized least squares for trend estimation of summarized dose–response data 2006;6(1):40–57.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. Bmj. 2008;336(7650):924–6.
Abbasi R, Bakhshimoghaddam F, Alizadeh M. Major dietary patterns in relation to preeclampsia among Iranian pregnant women: a case–control study. J Matern Fetal Neonatal Med. 2021;34(21):3529–36.
Alves-Santos NH, Cocate PG, Benaim C, Farias DR, Emmett PM, Kac G. Prepregnancy dietary patterns and their association with perinatal outcomes: a prospective cohort study. J Acad Nutr Diet. 2019;119(9):1439–51.
Asadi M, Shahzeidi M, Nadjarzadeh A, Hashemi Yusefabad H, Mansoori A. The relationship between pre-pregnancy dietary patterns adherence and risk of gestational diabetes mellitus in Iran: a case–control study. Nutr Diet. 2019;76(5):597–603.
Bao W, Tobias DK, Olsen SF, Zhang C. Pre-pregnancy fried food consumption and the risk of gestational diabetes mellitus: a prospective cohort study. Diabetol. 2014;57(12):2485–91.
Bartáková V, Kuricová K, Zlámal F, Bělobrádková J, Kaňková K. Differences in food intake and genetic variability in taste receptors between Czech pregnant women with and without gestational diabetes mellitus. Eur J Nutr. 2018;57(2):513–21.
Brantsæter AL, Haugen M, Samuelsen SO, Torjusen H, Trogstad L, Alexander J, et al. A dietary pattern characterized by high intake of vegetables, fruits, and vegetable oils is associated with reduced risk of preeclampsia in nulliparous pregnant Norwegian women. J Nutr. 2009;139(6):1162–8.
Chen LW, Hu FB, Yeung E, Willett W, Zhang CL. Prospective study of pre-gravid sugar-sweetened beverage consumption and the risk of gestational diabetes mellitus. Diabetes Care. 2009;32(12):2236–41.
Chia AR, de Seymour JV, Colega M, Chen LW, Chan YH, Aris IM, et al. A vegetable, fruit, and white rice dietary pattern during pregnancy is associated with a lower risk of preterm birth and larger birth size in a multiethnic Asian cohort: the growing up in Singapore towards healthy outcomes (GUSTO) cohort study. Am J Clin Nutr. 2016;104(5):1416–23.
de Seymour J, Chia AR, Colega M, Jones B, McKenzie E, Cai SR, et al. Maternal dietary patterns and gestational diabetes mellitus in a multi-ethnic Asian cohort: the GUSTO study. Nutrients. 2016;8(9)
Dominguez LJ, Martinez-Gonzalez MA, Basterra-Gortari FJ, Gea A, Barbagallo M, Bes-Rastrollo M. Fast food consumption and gestational diabetes incidence in the SUN project. PLoS One. 2014;9(9):e106627.
Donazar-Ezcurra M, Lopez-del Burgo C, Martinez-Gonzalez MA, Basterra-Gortari FJ, de Irala J, Bes-Rastrollo M. Soft drink consumption and gestational diabetes risk in the SUN project. Clin Nutr. 2018;37(2):638–45.
Dong JY, Kimura T, Ikehara S, Cui M, Kawanishi Y, Yamagishi K, et al. Chocolate consumption and risk of gestational diabetes mellitus: the Japan environment and Children's study. Br J Nutr. 2019;122(8):936–41.
Drozd-Dąbrowska M, Trusewicz R, Ganczak M. Selected risk factors of developmental delay in polish infants: a case-control study. Int J Environ Res Public Health. 2018;15(12)
Du HY, Jiang H, Karmin O, Bo C, Xu LJ, Liu SP, et al. Association of dietary pattern during pregnancy and gestational diabetes mellitus: a prospective cohort study in northern China. Biomed Environ Sci. 2017;30(12):887–97.
Englund-Ögge L, Brantsæter AL, Sengpiel V, Haugen M, Birgisdottir BE, Myhre R, et al. Maternal dietary patterns and preterm delivery: Results from large prospective cohort study. BMJ (Online). 2014;348
Gete DG, Waller M, Mishra GD. Prepregnancy dietary patterns and risk of preterm birth and low birth weight: findings from the Australian longitudinal study on Women's health. Am J Clin Nutr. 2020;111(5):1048–58.
Grieger JA, Grzeskowiak LE, Clifton VL. Preconception dietary patterns in human pregnancies are associated with preterm delivery. J Nutr. 2014;144(7):1075–80.
Grundt JH, Eide GE, Brantsæter AL, Haugen M, Markestad T. Is consumption of sugar-sweetened soft drinks during pregnancy associated with birth weight? Mater Child Nutrit. 2017;13(4):e12405.
Hajianfar H, Esmaillzadeh A, Feizi A, Shahshahan Z, Azadbakht L. The association between major dietary patterns and pregnancy-related complications. Archiv Iran Med. 2018;21(10):443–51.
Hehua Z, Yang X, Qing C, Shanyan G, Yuhong Z. Dietary patterns and associations between air pollution and gestational diabetes mellitus. Environ Int. 2021;147
Hezaveh ZS, Feizy Z, Dehghani F, Sarbakhsh P, Moini A, Vafa M. The association between maternal dietary protein intake and risk of gestational diabetes mellitus. International journal of. Prev Med. 2019;10(1)
Hu JJ, Oken E, Aris IM, Lin PID, Ma YA, Ding N, et al. Dietary patterns during pregnancy are associated with the risk of gestational diabetes mellitus: evidence from a Chinese prospective birth cohort study. Nutrients. 2019;11(2)
Ikem E, Halldorsson TI, Birgisdóttir BE, Rasmussen MA, Olsen SF, Maslova E. Dietary patterns and the risk of pregnancy-associated hypertension in the Danish National Birth Cohort: a prospective longitudinal study. BJOG: An Int J Obstetr Gynaecol. 2019;126(5):663–73.
Kahr MK, Suter MA, Ballas J, Ramin SM, Monga M, Lee W, et al. Geospatial analysis of food environment demonstrates associations with gestational diabetes. Am J Obstet Gynecol. 2016;214(1):110.e1-.e9.
Lamyian M, Hosseinpour-Niazi S, Mirmiran P, Banaem LM, Goshtasebi A, Azizi F. Pre-pregnancy fast food consumption is associated with gestational diabetes mellitus among tehranian women. Nutrients. 2017;9(3)
Leone A, Martínez-González M, Craig W, Fresán U, Gómez-Donoso C, Bes-Rastrollo M. Pre-gestational consumption of ultra-processed foods and risk of gestational diabetes in a Mediterranean cohort. The SUN project. Nutrients. 2021;13(7)
Lotfi MH, Fallahzadeh H, Rahmanian M, Hosseinzadeh M, Lashkardoost H, Doaei S, et al. Association of food groups intake and physical activity with gestational diabetes mellitus in Iranian women. J Mater -Fetal Neonatal Med. 2020;33(21):3559–64.
Marí-Sanchis A, Díaz-Jurado G, Basterra-Gortari FJ, de la Fuente-Arrillaga C, Martínez-González MA, Bes-Rastrollo M. Association between pre-pregnancy consumption of meat, iron intake, and the risk of gestational diabetes: the SUN project. Eur J Nutr. 2018;57(3):939–49.
Martin CL, Sotres-Alvarez D, Siega-Riz AM. Maternal dietary patterns during the second trimester are associated with preterm birth. J Nutr. 2015;145(8):1857–64.
Nascimento GR, Alves LV, Fonseca CL, Figueiroa JN, Alves JG. Dietary patterns and gestational diabetes mellitus in a low income pregnant women population in Brazil - a cohort study. Archivos Latinoamericanos de Nutricion. 2016;66(4):301–8.
Osorio-Yáñez C, Gelaye B, Qiu C, Bao W, Cardenas A, Enquobahrie DA, et al. Maternal intake of fried foods and risk of gestational diabetes mellitus. Ann Epidemiol. 2017;27(6):384–90.e1.
Rasmussen MA, Maslova E, Halldorsson TI, Olsen SF. Characterization of dietary patterns in the Danish National Birth Cohort in relation to preterm birth. PLoS One. 2014;9(4)
Saftlas AF, Triche EW, Beydoun H, Bracken MB. Does chocolate intake during pregnancy reduce the risks of preeclampsia and gestational hypertension? Ann Epidemiol. 2010;20(8):584–91.
Santos IS, Victora CG, Huttly S, Carvalhal JB. Caffeine intake and low birth weight: a population-based case-control study. Am J Epidemiol. 1998;147(7):620–7.
Sartorelli DS, Crivellenti LC, Zuccolotto DCC, Franco LJ. Relationship between minimally and ultra-processed food intake during pregnancy with obesity and gestational diabetes mellitus. Cadernos de Saude Publica. 2019;35(4)
Schoenaker DA, Soedamah-Muthu SS, Callaway LK, Mishra GD. Pre-pregnancy dietary patterns and risk of gestational diabetes mellitus: results from an Australian population-based prospective cohort study. Diabetol. 2015;58(12):2726–35. https://doi.org/10.1007/s00125-015-3742-1. Epub 2015 Sep 10.
Sedaghat F, Akhoondan M, Ehteshami M, Aghamohammadi V, Ghanei N, Mirmiran P, Rashidkhani B. Maternal Dietary Patterns and Gestational Diabetes Risk: A Case-Control Study. J Diabetes Res. 2017;2017:5173926. https://doi.org/10.1155/2017/5173926. Epub 2017 Dec 6.
Tamada H, Ebara T, Matsuki T, Kato S, Sato H, Ito Y, et al. Ready-meal consumption during pregnancy is a risk factor for stillbirth: the Japan environment and Children’s study (JECS). Japan environment and Children’s study, Ready-Meal Consumption During Pregnancy is a Risk Factor for Stillbirth: The Japan Environment and Children’s Study (JECS).
Teixeira JA, Hoffman DJ, Castro TG, Saldiva S, Francisco RPV, Vieira SE, et al. Pre-pregnancy dietary pattern is associated with newborn size: results from ProcriAr study. Br J Nutr. 2021;126(6):903–12.
Triche EW, Grosso LM, Belanger K, Darefsky AS, Benowitz NL, Bracken MB. Chocolate consumption in pregnancy and reduced likelihood of preeclampsia. Epidemiol. 2008;19(3):459–64.
Tryggvadottir EA, Medek H, Birgisdottir BE, Geirsson RT, Gunnarsdottir I. Association between healthy maternal dietary pattern and risk for gestational diabetes mellitus. Eur J Clin Nutr. 2016;70(2):237–42.
Tsoi KY, Chan RSM, Tam CH, Li LS, Tam WH, Ma RCW. Dietary patterns of Chinese pregnant women in Hong Kong. Asia Pac J Clin Nutr. 2022;31(3):378–93.
Wahedy K, El Bilbeisi AHH, Bakry MJ. DIETARY PATTERNS and THEIR ASSOCIATION with GLYCEMIC CONTROL and RISK of GESTATIONAL DIABETES MELLITUS in GAZA STRIP, PALESTINE: a CASE-CONTROL STUDY. Bullet Pharmaceut Sci Assiut. 2021;44(2):537–49.
Wen L, Ge H, Qiao J, Zhang L, Chen X, Kilby MD, et al. Maternal dietary patterns and risk of gestational diabetes mellitus in twin pregnancies: a longitudinal twin pregnancies birth cohort study. Nutr J. 2020;19(1)
Yisahak SF, Hinkle SN, Mumford SL, Gleason JL, Grantz KL, Zhang C, et al. Periconceptional and first trimester Ultraprocessed food intake and maternal Cardiometabolic outcomes. Diabetes Care. 2022;45(9):2028–36.
Yong HY, Mohd Shariff Z, Mohd Yusof BN, Rejali Z, Tee YYS, Bindels J, van der Beek EM. Beverage Intake and the Risk of Gestational Diabetes Mellitus: The SECOST. Nutrients. 2021;13(7):2208. https://doi.org/10.3390/nu13072208.
Zareei S, Homayounfar R, Naghizadeh MM, Ehrampoush E, Amiri Z, Rahimi M, et al. Dietary pattern in patients with preeclampsia in Fasa. Iran Shiraz E Med J. 2019;20(11)
Zareei S, Homayounfar R, Naghizadeh MM, Ehrampoush E, Rahimi M. Dietary pattern in pregnancy and risk of gestational diabetes mellitus (GDM). Diabet Metabol Syndrome: Clin Res Rev. 2018;12(3):399–404.
Zhang C, Schulze MB, Solomon CG, Hu FB. A prospective study of dietary patterns, meat intake and the risk of gestational diabetes mellitus. Diabetologia. 2006;49(11):2604-13. https://doi.org/10.1007/s00125-006-0422-1. Epub 2006 Sep 7.
Zuccolotto DCC, Crivellenti LC, Franco LJ, Sarotelli DS. Dietary patterns of pregnant women, maternal excessive body weight and gestational diabetes. Revista de Saude Publica. 2019;53.
Moradi S, Hojjati Kermani MA, Bagheri R, Mohammadi H, Jayedi A, Lane MM, et al. Ultra-processed food consumption and adult diabetes risk: a systematic review and dose-response Meta-analysis. Nutrients. 2021;13(12)
Suksatan W, Moradi S, Naeini F, Bagheri R, Mohammadi H, Talebi S, Mehrabani S, Hojjati Kermani MA, Suzuki K. Ultra-Processed Food Consumption and Adult Mortality Risk: A Systematic Review and Dose-Response Meta-Analysis of 207,291 Participants. Nutrients. 2021;14(1):174. https://doi.org/10.3390/nu14010174.
Babaei A, Pourmotabbed A, Talebi S, Mehrabani S, Bagheri R, Ghoreishy SM, et al. The association of ultra-processed food consumption with adult inflammatory bowel disease risk: a systematic review and dose-response meta-analysis of 4 035 694 participants. Nutr Rev. 2023;
Umesawa M, Kobashi G. Epidemiology of hypertensive disorders in pregnancy: prevalence, risk factors, predictors and prognosis. Hyperten res: official j Japan Soc Hypert. 2017;40(3):213–20.
Sutan R, Aminuddin NA, Mahdy ZA. Prevalence, maternal characteristics, and birth outcomes of preeclampsia: a cross-sectional study in a single tertiary healthcare center in greater Kuala Lumpur Malaysia. Front Public Health. 2022;10:973271.
Bodnar LM, Ness RB, Markovic N, Roberts JM. The risk of preeclampsia rises with increasing prepregnancy body mass index. Ann Epidemiol. 2005;15(7):475–82.
Catalano PM, McIntyre HD, Cruickshank JK, McCance DR, Dyer AR, Metzger BE, et al. The hyperglycemia and adverse pregnancy outcome study: associations of GDM and obesity with pregnancy outcomes. Diabetes Care. 2012;35(4):780–6.
Perry A, Stephanou A, Rayman MP. Dietary factors that affect the risk of pre-eclampsia. BMJ nutrit prevent health. 2022;5(1):118–33.
Martini D, Godos J, Bonaccio M, Vitaglione P, Grosso G. Ultra-processed foods and nutritional dietary profile: a Meta-analysis of nationally representative samples. Nutrients. 2021;13(10)
Maldonado-Pereira L, Barnaba C, de Los CG, Medina-Meza IG. Evaluation of the nutritional quality of ultra-processed foods (ready to eat + fast food): fatty acids, sugar, and sodium. J Food Sci. 2022;87(8):3659–76.
Monguchi T, Hara T, Hasokawa M, Nakajima H, Mori K, Toh R, et al. Excessive intake of trans fatty acid accelerates atherosclerosis through promoting inflammation and oxidative stress in a mouse model of hyperlipidemia. J Cardiol. 2017;70(2):121–7.
Ma X, Nan F, Liang H, Shu P, Fan X, Song X, et al. Excessive intake of sugar: an accomplice of inflammation. Front Immunol. 2022;13:988481.
Wojcik M, Krawczyk M, Zieleniak A, Mac Marcjanek K, Wozniak LA. Chapter 14 - associations of high blood sugar with oxidative stress and inflammation in patients with type 2 diabetes. In: Preuss HG, Bagchi D, editors. Dietary Sugar Salt and Fat in Human Health. Academic Press; 2020. p. 305–23.
Chiarello DI, Abad C, Rojas D, Toledo F, Vázquez CM, Mate A, et al. Oxidative stress: Normal pregnancy versus preeclampsia. Biochim Biophys Acta (BBA)-Mol Basis Dis. 2020;1866(2):165354.
Harmon AC, Cornelius DC, Amaral LM, Faulkner JL, Cunningham MW, Jr., Wallace K, et al. The role of inflammation in the pathology of preeclampsia. Clinical science (London, England : 1979). 2016;130(6):409–19.
Patik JC, Lennon SL, Farquhar WB, Edwards DG. Mechanisms of dietary sodium-induced impairments in Endothelial function and potential countermeasures. Nutrients. 2021;13(1)
Shuto E, Taketani Y, Tanaka R, Harada N, Isshiki M, Sato M, et al. Dietary phosphorus acutely impairs endothelial function. J Am Soc Nephrol: JASN. 2009;20(7):1504–12.
Lopez-Garcia E, Schulze MB, Meigs JB, Manson JE, Rifai N, Stampfer MJ, et al. Consumption of trans fatty acids is related to plasma biomarkers of inflammation and Endothelial Dysfunction1. J Nutr. 2005;135(3):562–6.
Lamarca B. Endothelial dysfunction. An important mediator in the pathophysiology of hypertension during pre-eclampsia. Minerva Ginecol 2012;64(4):309–20.
Fernandes AE, Rosa PWL, Melo ME, Martins RCR, Santin FGO, Moura AMSH, et al. Differences in the gut microbiota of women according to ultra-processed food consumption. Nutr Metab Cardiovasc Dis. 2023;33(1):84–9. https://doi.org/10.1016/j.numecd.2022.09.025. Epub 2022 Oct 11.
Whelan K, Bancil AS, Lindsay JO, Chassaing B. Ultra-processed foods and food additives in gut health and disease. Nat Rev Gastroenterol Hepatol. 2024;22:1–22.
Fan M, Li X, Gao X, Dong L, Xin G, Chen L, et al. LPS induces preeclampsia-like phenotype in rats and HTR8/SVneo cells dysfunction through TLR4/p38 MAPK pathway. Front Physiol. 2019;10:1030.
Jin J, Gao L, Zou X, Zhang Y, Zheng Z, Zhang X, et al. Gut Dysbiosis promotes preeclampsia by regulating macrophages and trophoblasts. Circ Res. 2022;131(6):492–506.
Kell DB, Kenny LC. A dormant microbial component in the development of preeclampsia. Front Med. 2016;3:60.
Rauber F, Chang K, Vamos EP, da Costa Louzada ML, Monteiro CA, Millett C, et al. Ultra-processed food consumption and risk of obesity: a prospective cohort study of UK biobank. Eur J Nutr. 2021;60(4):2169–80.
Wondmkun YT. Obesity, insulin resistance, and type 2 diabetes: associations and therapeutic implications. Diabet metab syndrome obes: targets therapy. 2020;13:3611–6.
Teran E, Escudero C, Moya W, Flores M, Vallance P, Lopez-Jaramillo P. Elevated C-reactive protein and pro-inflammatory cytokines in Andean women with pre-eclampsia. Int J Gynecol Obstet. 2001;75(3):243–9.
Palei AC, Spradley FT, Granger JP. Chronic hyperleptinemia results in the development of hypertension in pregnant rats. Am J Phys Regul Integr Comp Phys. 2015;308(10):R855–R61.
Olson KN, Redman LM, Sones JL. Obesity "complements" preeclampsia. Physiol Genom. 2019;51(3):73–6.
Wang X, Cheng Z. Cross-sectional studies: strengths, weaknesses, and recommendations. Chest. 2020;158(1 Supplement):S65–71.
Mozaffarian D, Ludwig DS. Dietary guidelines in the 21st century—a time for food. Jama. 2010;304(6):681–2.
Wang H, Li N, Chivese T, Werfalli M, Sun H, Yuen L, et al. IDF diabetes atlas: estimation of global and regional gestational diabetes mellitus prevalence for 2021 by International Association of Diabetes in pregnancy study Group's criteria. Diabetes Res Clin Pract. 2022;183:109050.
Kityo A, Lee SA. The intake of ultra-processed foods and prevalence of chronic kidney disease: the health examinees study. Nutrients. 2022;14(17)
Nardocci M, Leclerc B-S, Louzada M-L, Monteiro CA, Batal M, Moubarac J-C. Consumption of ultra-processed foods and obesity in Canada. Can J Public Health. 2019;110:4–14.
Rauber F, Louzada MLC, Steele EM, Millett C, Monteiro CA, Levy RB. Ultra-processed food consumption and chronic non-communicable diseases-related dietary nutrient profile in the UK (2008–2014). Nutrients. 2018;10(5):587.
Lavigne-Robichaud M, Moubarac J-C, Lantagne-Lopez S, Johnson-Down L, Batal M, Sidi EAL, et al. Diet quality indices in relation to metabolic syndrome in an indigenous Cree (Eeyouch) population in northern Québec. Canada Pub health nutrit. 2018;21(1):172–80.
Sun Y, Shen Z, Zhan Y, Wang Y, Ma S, Zhang S, et al. Effects of pre-pregnancy body mass index and gestational weight gain on maternal and infant complications. BMC pregnan childbirth. 2020;20(1):1–13.
Linder T, Eder A, Monod C, Rosicky I, Eppel D, Redling K, et al. Impact of prepregnancy overweight and obesity on treatment modality and pregnancy outcome in women with gestational diabetes mellitus. Front Endocrinol. 2022;13:799625.
Najafi F, Hasani J, Izadi N, Hashemi-Nazari S-S, Namvar Z, Shamsi H, et al. Risk of gestational diabetes mellitus by pre-pregnancy body mass index: a systematic review and meta-analysis. Diabet Metab Syndrome: Clin Res Rev. 2021;15(4):102181.
McIntyre HD, Catalano P, Zhang C, Desoye G, Mathiesen ER, Damm P. Gestational diabetes mellitus. Nat Rev Dis Primers. 2019;5(1):47.
Plows JF, Stanley JL, Baker PN, Reynolds CM, Vickers MH. The pathophysiology of gestational diabetes mellitus. Int J Mol Sci. 2018;19(11):3342.
Stanhope KL. Sugar consumption, metabolic disease and obesity: the state of the controversy. Crit Rev Clin Lab Sci. 2016;53(1):52–67.
Bhattacharyya S, I OS, Katyal S, Unterman T, Tobacman JK. Exposure to the common food additive carrageenan leads to glucose intolerance, insulin resistance and inhibition of insulin signalling in HepG2 cells and C57BL/6J mice. Diabetologia. 2012;55(1):194–203.
Quetglas-Llabrés MM, Monserrat-Mesquida M, Bouzas C, Mateos D, Ugarriza L, Gómez C, et al. Oxidative stress and inflammatory biomarkers are related to high intake of ultra-processed food in old adults with metabolic syndrome. Antioxidants (Basel, Switzerland). 2023;12(8).
Yaribeygi H, Sathyapalan T, Atkin SL, Sahebkar A. Molecular mechanisms linking oxidative stress and diabetes mellitus. Oxidative Med Cell Longev. 2020;2020:8609213.
Bertoli S, Leone A, Battezzati A. Human bisphenol a exposure and the “diabesity phenotype”. Dose-Response. 2015;13(3):1559325815599173.
Rolfo A, Nuzzo AM, De Amicis R, Moretti L, Bertoli S, Leone A. Fetal–maternal exposure to endocrine disruptors: correlation with diet intake and pregnancy outcomes. Nutrients. 2020;12(6):1744.
Lorenzo PI, Martín-Montalvo A, Cobo Vuilleumier N, Gauthier BR. Molecular modelling of islet β-cell adaptation to inflammation in pregnancy and gestational diabetes mellitus. Int J Mol Sci. 2019;20(24)
Christ A, Lauterbach M, Latz E. Western diet and the immune system: an inflammatory connection. Immunity. 2019;51(5):794–811.
Neale E, Batterham M, Tapsell LC. Consumption of a healthy dietary pattern results in significant reductions in C-reactive protein levels in adults: a meta-analysis. Nutr Res. 2016;36(5):391–401.
Liu Z, Lu Y, Zhong K, Wang C, Xu X. The associations between endocrine disrupting chemicals and markers of inflammation and immune responses: a systematic review and meta-analysis. Ecotoxicol Environ Saf. 2022;234:113382.
Node K, Inoue T. Postprandial hyperglycemia as an etiological factor in vascular failure. Cardiovasc Diabetol. 2009;8:23.
Hu Z, Tylavsky FA, Kocak M, Fowke JH, Han JC, Davis RL, et al. Effects of maternal dietary patterns during pregnancy on early childhood growth trajectories and obesity risk: the CANDLE study. Nutrients. 2020;12(2)
Wang Y, Wang K, Du M, Khandpur N, Rossato SL, Lo C-H, et al. Maternal consumption of ultra-processed foods and subsequent risk of offspring overweight or obesity: results from three prospective cohort studies. Bmj. 2022:379.
Paula WO, Gonçalves VSS, Patriota ESO, Franceschini SCC, Pizato N. Impact of ultra-processed food consumption on quality of diet among Brazilian pregnant women assisted in primary health care. Int J Environ Res Public Health. 2023;20(2)
Crume TL, Brinton JT, Shapiro A, Kaar J, Glueck DH, Siega-Riz AM, et al. Maternal dietary intake during pregnancy and offspring body composition: the healthy start study. Am J Obstet Gynecol. 2016;215(5):609–e1-e8.
Wan Y, Chen Y, Wu X, Yin A, Tian F, Zhang H, et al. Mediation effect of maternal triglyceride and fasting glucose level on the relationship between maternal overweight/ obesity and fetal growth: a prospective cohort study. BMC Pregnancy and Childbirth. 2023;23(1):449.
Akbari Z, Mansourian M, Kelishadi R. Relationship of the intake of different food groups by pregnant mothers with the birth weight and gestational age: need for public and individual educational programs. J educ health promot. 2015;4:23.
Fischer S, Morales-Suárez-Varela M. The bidirectional relationship between gestational diabetes and depression in pregnant women: a systematic search and review. Healthcare (Basel, Switzerland). 2023;11(3).
Khan R, Waqas A, Bilal A, Mustehsan ZH, Omar J, Rahman A. Association of Maternal depression with diet: a systematic review. Asian J Psychiatr. 2020;52:102098.
Ancira-Moreno M, O'Neill MS, Rivera-Dommarco J, Batis C, Rodríguez Ramírez S, Sánchez BN, et al. Dietary patterns and diet quality during pregnancy and low birthweight: the PRINCESA cohort. Matern Child Nutr. 2020;16(3):e12972.
Acknowledgments
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
SM and ST designed this study. SM, MZ and PA contributed to the conduct of the search. SM and ST performed the statistical analysis and interpreted the results. SM, SM-GH, Sanaz Merabani, and MA-HK wrote the initial manuscript. AW, AM and PR_F critically revised the manuscript and contributed to the subsequent drafts of the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Talebi, S., Mehrabani, S., Ghoreishy, S.M. et al. The association between ultra-processed food and common pregnancy adverse outcomes: a dose-response systematic review and meta-analysis. BMC Pregnancy Childbirth 24, 369 (2024). https://doi.org/10.1186/s12884-024-06489-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-024-06489-w