-
PDF
- Split View
-
Views
-
Cite
Cite
Hillary D Lum, Kathryn Nearing, Camilla B Pimentel, Cari R Levy, William W Hung, Anywhere to Anywhere: Use of Telehealth to Increase Health Care Access for Older, Rural Veterans, Public Policy & Aging Report, Volume 30, Issue 1, 2020, Pages 12–18, https://doi.org/10.1093/ppar/prz030
Close - Share Icon Share
Introduction
Rural veterans are older and have more complex medical issues than their urban counterparts. Veterans aged 65 and above represent 57% of all rural veterans who are enrolled in the Veterans Health Administration (VHA; Department of Veterans Affairs, 2019a). These older adults often have multiple chronic conditions and aging-related issues that require care from multiple disciplines, including primary care, specialty care, mental health care, and coordinated health and social services; and yet, accessing these services at a health-care facility may require extensive travel. This article describes telehealth approaches by the VHA, including the Geriatric Research Education and Clinical Centers (GRECC) Connect clinical demonstration project, to increase access to geriatric care for aging veterans and family caregivers residing in rural areas.
Health-Care Needs Among Older Rural Veterans
In 2015, there were 21.5 million veterans living in the United States. Of these, about 4.7 million veterans (24%) lived in rural America (Cowper Ripley, Ahern, Litt, & Wilson, 2017). Rural veterans are significantly older than urban veterans. This older veteran population is medically complex and more likely to be diagnosed with diabetes, obesity, high blood pressure, and heart conditions that require more frequent, ongoing, and costly care (Department of Veterans Affairs, 2019a).
Health-care provider shortages, long distances to health-care facilities, and limited transportation options often keep rural veterans from obtaining timely and quality care. Interdisciplinary geriatric teams have the expertise to improve care for older veterans with complex needs, but veterans in rural areas often lack access to specialized geriatric care (Gruen, Weeramanthri, Knight, & Bailie, 2006). Rural health-care providers often indicate a need for support and education to address the complex needs of older adults (Tumosa et al., 2012).
The demand for geriatricians is projected to outpace the supply, leading to a national shortage of about 27,000 geriatricians by 2025 (Supiano et al., 2012). Additionally, more than 90% of geriatric specialists reside in urban areas (Peterson, Bazemore, Bragg, Xierali, & Warshaw, 2011), leaving a dearth of geriatric expertise in rural areas, both within the VHA and through community-based providers. Thus, even with expanded access to community-based health care through the Veterans Affairs (VA) MISSION Act (https://missionact.va.gov/), veterans still face limited access to geriatricians and associated interdisciplinary teams.
Veterans Health Administration Commitment to Rural Health
The VHA Office of Rural Health advances the VHA’s commitment to improving the health and wellbeing of veterans living in rural areas (www.ruralhealth.va.gov; Department of Veterans Affairs, 2019a). The VHA is a prominent source of health care for rural residents, as evidenced by 58% of rural veterans choosing to enroll in the VA health-care system, compared to the 37% enrollment rate among urban veterans (Cowper Ripley et al., 2017). To overcome challenges to health-care access, the VHA Office of Rural Health uses telehealth technology to help rural veterans access clinical services from their home or nearby VHA facilities. In fiscal year (FY) 2018, the Office of Rural Health supported telehealth care for more than 291,000 rural veterans, funded more than 20 virtual programs, and dedicated $120 million to VA telehealth programs (Department of Veterans Affairs, 2019b).
Telehealth Approaches for Older Rural Veterans
What is Telehealth?
In 1996, the Institute of Medicine, now known as the National Academies of Science, Engineering, and Medicine, defined telemedicine as “the use of electronic information and communications technologies to provide and support health care when distance separates participants” (Institute of Medicine, 1996). Attention to telehealth has rapidly grown over the past two decades in the public and private sectors. Multiple stakeholders, including innovators, health-care providers, health systems, payers, and the federal government are actively engaged in developing and implementing technology, practices, policies, and payment models for telehealth. The use of telehealth to provide clinical support to individuals separated geographically has the potential to increase access to care and facilitate “healing at a distance” (Dorsey & Topol, 2016). Telehealth has become an important tool for enhancing health-care service delivery, reducing costs, and increasing quality (Wade, Karnon, Elshaug, & Hiller, 2010).
Veterans Health Administration Commitment to Telehealth
Through the Office of Connected Care, the VHA is the largest provider of telehealth services in the country (https://connectedcare.va.gov/). The VHA began piloting telehealth technologies in the 1990s and provides telehealth access through three primary modalities: Clinical Video Telehealth, Store-and-Forward Telehealth, and Remote Patient Monitoring (Table 1; https://www.telehealth.va.gov/; Institute of Medicine, 2012). As a subset of clinical video telehealth, VHA video-to-home telehealth (also known as VA Video Connect) provides care for veterans directly in their homes. Both clinic and home telehealth visits can facilitate chronic care management, mental health care, health promotion, disease prevention, and caregiver support. To support clinical telehealth, the VHA has dedicated national telehealth training centers for staff. The VHA continues to expand telehealth access through the “Anywhere to Anywhere” initiative, a new federal rule that allows VHA health-care providers to deliver care using telehealth technology across state lines (Department of Veterans Affairs, 2018). A June 2018 communication (VHA Notice 2018–25, “Expansion Of Telehealth Services Into The Home And Other Non-VA Settings”) described the VHA goal to ensure that 100% of VHA primary care teams and outpatient mental health providers are capable of delivering telehealth services to a veteran’s mobile device by the end of FY2020. Based on these operational goals, any VHA outpatient appointment is a potential candidate for telehealth services if it does not require hands-on services.
Telehealth Modalities in the Veterans Health Administration
| Telehealth Modality . | Description . |
|---|---|
| Clinical video telehealth | Synchronous, real-time visits between patients and clinicians via a communications link. Rural Veterans at home or at local VHA Community-Based Outpatient Clinics interact with VHA primary care physicians or specialists through a secure video platform. |
| Store-and-forward telehealth | Asynchronous encounter where providers electronically send images, sounds, and videos to be evaluated by experts who may be thousands of miles away. It does not require the simultaneous presence of both parties. |
| Remote patient monitoring | Clinicians and case managers use simple technology to remotely monitor health data from rural veterans’ homes. |
| Telehealth Modality . | Description . |
|---|---|
| Clinical video telehealth | Synchronous, real-time visits between patients and clinicians via a communications link. Rural Veterans at home or at local VHA Community-Based Outpatient Clinics interact with VHA primary care physicians or specialists through a secure video platform. |
| Store-and-forward telehealth | Asynchronous encounter where providers electronically send images, sounds, and videos to be evaluated by experts who may be thousands of miles away. It does not require the simultaneous presence of both parties. |
| Remote patient monitoring | Clinicians and case managers use simple technology to remotely monitor health data from rural veterans’ homes. |
Note. VHA = Veterans Health Administration.
Telehealth Modalities in the Veterans Health Administration
| Telehealth Modality . | Description . |
|---|---|
| Clinical video telehealth | Synchronous, real-time visits between patients and clinicians via a communications link. Rural Veterans at home or at local VHA Community-Based Outpatient Clinics interact with VHA primary care physicians or specialists through a secure video platform. |
| Store-and-forward telehealth | Asynchronous encounter where providers electronically send images, sounds, and videos to be evaluated by experts who may be thousands of miles away. It does not require the simultaneous presence of both parties. |
| Remote patient monitoring | Clinicians and case managers use simple technology to remotely monitor health data from rural veterans’ homes. |
| Telehealth Modality . | Description . |
|---|---|
| Clinical video telehealth | Synchronous, real-time visits between patients and clinicians via a communications link. Rural Veterans at home or at local VHA Community-Based Outpatient Clinics interact with VHA primary care physicians or specialists through a secure video platform. |
| Store-and-forward telehealth | Asynchronous encounter where providers electronically send images, sounds, and videos to be evaluated by experts who may be thousands of miles away. It does not require the simultaneous presence of both parties. |
| Remote patient monitoring | Clinicians and case managers use simple technology to remotely monitor health data from rural veterans’ homes. |
Note. VHA = Veterans Health Administration.
Veterans Health Administration Utilization of Telehealth Modalities
Telehealth technology helps the VHA improve rural veterans’ health and wellbeing by connecting rural communities with qualified clinicians, thereby increasing access to specialists and reducing travel distances to care (Department of Veterans Affairs, 2019b). Between 2009–2015, annual clinical video telehealth utilization in the VHA grew from 30 to 124 encounters per 1,000 veterans (>300% increase), with faster growth among rural veterans than urban veterans (Adams et al., 2019). In FY2018, 13% of veterans who received VHA care did so via telehealth. In a 2016–2017 evaluation of video-to-home telehealth visits using a VHA-provided tablet, veterans with mental health diagnoses had more psychotherapy encounters and more medication management visits, were more likely to engage in continuity of care, and had fewer missed appointments (Jacobs et al., 2019).
Telehealth for Older Rural Veterans
Geriatric Research Education and Clinical Centers Connect
The VHA established GRECCs as centers of excellence focused on supporting veterans as they age. There are 20 GRECCs in 18 geographic regions, or VISNs (Veterans Integrated Service Networks), across the VHA. With their focus on research, education, and clinical innovation, the GRECC network has made major contributions to the advancement of aging-related research, geriatric training across diverse professions, and clinical care within and outside the VHA (Supiano et al., 2012). In 2014, the VHA Office of Geriatrics and Extended Care and the VHA Office of Rural Health established the GRECC Connect clinical demonstration project. GRECC Connect leverages the VHA’s existing telehealth technologies and the geriatric expertise of the GRECC network to meet the health-care needs of older veterans in rural areas.
The clinical goal of GRECC Connect is to improve access to geriatric consultative care for older rural veterans with complex medical issues who are at increased risk for institutionalization and have limited access to care. The project is implemented using a “hub and spoke” model, where urban VHA medical center hub sites (Figure 1) are connected to VHA community-based outreach clinic spokes that primarily serve veterans in rural communities. Each hub site partners with an average of six clinics (range 3–16), each of which is an average distance of 93 miles from the hub VA medical center (range 19.5–406.4 miles; Pimentel et al., 2019). By FY2019, GRECC Connect had implemented telehealth modalities for geriatric care from 16 hub VA medical center sites to reach 107 spoke clinics.
GRECC Connect hub locations, as of October 2019. GRECC Connect links geriatrics specialists from GRECCs, located at VHA medical centers, with rural areas through clinical video telehealth, electronic consultation, and educational teleconferences. The current list is available at https://www.gerischolars.org/mod/page/view.php?id=1066. GRECC = Geriatric Research, Education and Clinical Center; VHA = Veterans Health Administration.
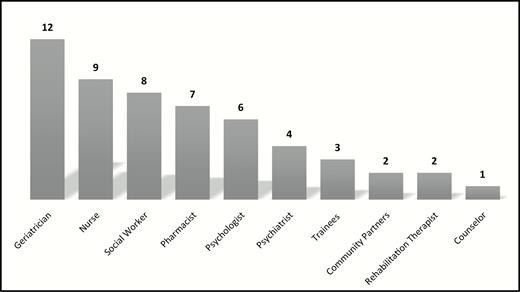
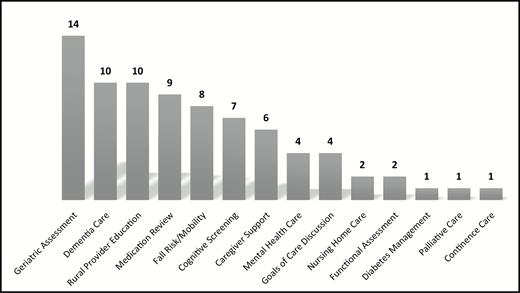
GRECC Connect provides interprofessional, telehealth-based consultative support to rural primary care providers through diverse geriatric teams (Figure 2). Consultations between GRECC Connect teams and rural VHA primary care providers address various aspects of geriatric care, ranging from broad concerns to sub-specialty areas of geriatric medicine. Tailored to the needs of rural VHA providers and veterans, as well as the clinical expertise of each hub site, clinical geriatrics services through GRECC Connect are diverse, addressing a wide array of issues common to older adults, such as dementia, falls and mobility, multiple chronic diseases, and polypharmacy (Figure 3). Hubs also provide caregiver support through telehealth, including home-based clinical video telehealth.
Number of GRECC Connect hubs with each professional represented (n = 12 sites). GRECC = Geriatric Research, Education and Clinical Center.
Number of GRECC Connect hubs that provide each type of geriatric service (n = 12 sites). GRECC = Geriatric Research, Education and Clinical Center.
Impact of Geriatric Research Education and Clinical Centers Connect
In 2019, a national cross-site evaluation of GRECC Connect was conducted by professional evaluators and researchers affiliated with the Eastern Colorado GRECC and New England GRECC. The evaluation was guided by the RE-AIM (Reach, Effectiveness, Adoption, Implementation and Maintenance) framework (Belza, Toobert, & Glasgow, 2007), as mandated by Office of Rural Health for the evaluation of enterprise-wide dissemination projects. Since its inception in 2014, the GRECC Connect project has provided direct clinical support to more than 6,000 veterans, of whom approximately 50% were seen for a cognition-related issue. In FY2018, an estimated 1,622 veterans were served, saving a total of 179,121 miles in travel (an average of 106 miles/veteran, corresponding to an out-of-pocket savings of $58/veteran in travel costs). Through the program, geriatrics consultation was available to older, rural veterans who otherwise would find travel to urban centers prohibitive. Veterans described high satisfaction with telehealth consultation and a preference for visits at a distance instead of traveling, which reduced stresses related to city driving, parking, and wayfinding. Ongoing evaluations are addressing potential benefits or burdens for subgroups of veterans, such as those with cognitive concerns.
Based on interviews with interprofessional geriatrics providers at GRECC Connect hubs, specific telehealth outcomes have included increased quality of life for veterans and caregivers; improved access to resources for veterans and caregivers, including durable medical equipment and medical supplies; increased physical functioning; decreased caregiver burdens; and timely discussions of diagnoses, prognosis, and future care planning. Providers described benefits from access to geriatric expertise, such as from a geriatrician, geropsychologist, geriatric social worker, nurse care manager, or pharmacist, through clinical video telehealth or electronic consultation. Geriatric telehealth consultations helped identify additional care needs for older veterans, such as additional support needs of veterans with dementia at home and linkage to care through VHA or non-VHA home care programs. Consultation with GRECC Connect teams also led to improved use of medications by identifying and stopping potentially inappropriate medications. Approximately 60% of veterans seen through GRECC Connect had medication changes, with an average of 2.2 medication changes per veteran. These data highlight the direct impact of GRECC Connect on rural, older veterans and caregivers. Providers also benefitted from expanded access to geriatric-specific expertise and education, to increase the local capacity to care for older veterans with complex health-care needs.
Lessons Learned from Geriatric Research Education and Clinical Centers Connect Implementation
In a rapid four-year scale-up, GRECC Connect successfully established a national network and enhanced relationships between GRECC-based clinical teams at hub VA medical centers and rural, spoke, clinic-based teams. The cross-site evaluation focused on exploring implementation facilitators and barriers, and extrapolating lessons that might inform other health-care system or policy initiatives designed to reach older, rural veterans. Successful implementation strategies included direct outreach to and engagement of staff at rural community-based outpatient clinics, to develop new or leverage existing relationships with providers, and responding to providers’ needs and local contexts. Examples of the latter included providing geriatric expertise to help care for patients with complex problems, help with patient loads, and integrate telehealth support into existing clinic workflows to make the referral process as seamless as possible. A surprising finding was the extent to which GRECC Connect hubs leveraged relationships with former trainees to support implementation, in an example of the integration of GRECC educational and clinical service missions. Other strategies included engaging leaders and staff at different levels (from administrative leaders and service chiefs to front-line primary care staff and telehealth staff). Despite the geographic distances, two GRECC Connect hubs specifically mentioned doing annual face-to-face meetings with rural clinics in order to maintain relationships, ensure staff had information about telehealth services, and share data about the impacts on patient populations.
GRECC Connect implementation also encountered multiple barriers. The initial start-up is intensive, with the logistics of establishing telehealth services (i.e., sufficient staffing capacity and training, coordination between hub and spoke teams, establishing the consult and documentation in the electronic health record, and identifying necessary telehealth equipment) all requiring significant time and effort, as well as multi-level buy-ins from facility leadership, multiple service lines, and team members. Once established, hubs consistently reported that the degree of turnover at rural facilities among providers and staff was an ongoing challenge that made it more difficult to build momentum or sustain success. GRECC Connect hubs also reported that it was challenging to engage primary care providers, particularly those further away or those affiliated with another VA health-care system. In contrast, providers with a specific need, such as an anesthesiologist interested in instituting comprehensive cognitive assessments prior to older veterans undergoing elective surgery, tended to be more receptive to the GRECC hub team’s efforts to partner in care. When referrals from rural clinics were infrequent, some hubs leveraged the existence of a shared VHA electronic health record between the hubs and spoke clinics to implement case-finding strategies to reach older veterans with geriatrics needs (i.e., polypharmacy, multiple care transitions, falls, osteoporosis management).
Policy Implications Related to Telehealth for Older Rural Veterans
The VHA is the largest single provider of health care services in the United States and provides a significant proportion of health care for older veterans who live in rural and frontier areas. The GRECC Connect project provides a robust example of how VHA telehealth approaches can implement and sustain coordinated access to care that is otherwise scarce. The rural-urban distribution of providers with geriatric expertise and older adults results in a mismatch of needs and available resources. Thus, it is necessary to identify solutions to bring geriatric care to rural areas. Even with the expansion of access for veterans who seek community-based care outside of the VHA, the MISSION Act cannot address the paucity of providers with geriatric expertise. The tensions of supply and demand will persist regardless of geography or the health-care system in which individuals seek care. Through partnerships between several VHA programs, including the Office of Rural Health, the Office of Connected Care, and VA Telehealth Services, the GRECC Connect program demonstrates the benefits of telehealth as a way to assist with meeting the needs of rural older adults. The success of the GRECC Connect program is directly related to the VHA’s policies and forward-thinking investment in telehealth technology, training and technical support, and innovative implementation efforts through the support of telehealth clinical demonstration projects using multiple telehealth modalities.
As an integrated health-care system, the VHA has unique advantages that are readily leveraged by the inclusion of telehealth as part of health-care delivery services. A single electronic health record enables communication and sharing of necessary health information. VHA reimbursement is broader and far more inclusive of telehealth modalities than current rules for Medicare. Clinical staff receive workload credits for telehealth visits through established VHA reimbursement mechanisms that are equivalent to in-person visits. As an integrated system, VHA staff on both the consulting and receiving ends of telehealth consultations share a similar mission, culture, and training to serve veterans. There is also an established structure that can be leveraged to deliver telehealth specifically, a network of VHA medical centers, affiliated community-based outpatient clinics, and other associated facilities which share telehealth and other relevant policies. Importantly, the VHA is strongly positioned to provide veterans with health care anywhere to anywhere through a VHA policy that enables health-care providers to provide care to veterans across state lines, overcoming state-specific credentialing policies that apply outside the VHA.
Future Directions
To optimize clinical video telehealth, there are opportunities to redesign reimbursement systems to mitigate challenges to adoption. Under Medicare Part B, clinical telehealth visit reimbursement remains limited to once monthly. For telehealth services to be broadly available outside of the VHA, Medicare and other payers will need to address several policy levers, including breaking down barriers for reimbursement, establishing shared electronic health information systems, and ensuring patients have access to reliable and secure telehealth technology (including technical support). Implementation will also require systematic training in telehealth technology and expanded knowledge of the health and social services that are proximal to the patient. Telehealth competencies are rarely part of the health-care professionals’ curricula, and there are few educational resources to train providers on the use of telehealth. Notably, more than 60 VHA requirements exist regarding the establishment of telehealth programs, and they are often beyond the competency of most individual VA staff (Institute of Medicine, 2012). Therefore, VHA training and support infrastructure provides system-wide training and staff to assist front-line clinical teams.
As the VHA and other health-care systems adopt telehealth services, evaluations of clinical effectiveness and quality monitoring, as well as adequate staff training, are essential. The VHA has national databases, reports, and analyses for metrics of performance and the quality of telehealth programs at the levels of the local VA medical center, the VHA networks, and nationwide. As telehealth services are increasingly utilized, analyses that include VHA and non-VHA health care clinical data can estimate the quality and impact of telehealth, while also evaluating the overall health outcomes of the population served.
Conclusion
As a national VHA clinical dissemination project, GRECC Connect has demonstrated that it is both feasible and effective to provide specialty geriatric consultations to older, rural veterans through telehealth. Key benefits include improved access to health care, timelier diagnoses and improved management of complex conditions, reductions in drive times, and reduced transportation costs. In the context of the VHA system, important implementation lessons can be applied to other telehealth or rural-based dissemination efforts. In particular, VHA investments in telehealth infrastructure, training, and shared policies, along with significant attention to building clinical relationships to establish new teams, were important for the integration of geriatric telehealth services into existing clinical workflows to transcend turnover. Because the population is aging and experiencing increased medical complexity, access to appropriate and coordinated care, especially in rural and frontier areas, is essential to addressing health disparities. Effective telehealth services that facilitate the delivery of scarce health-care services to wherever they are most needed may begin to help address this gap.
Funding
None declared.
Conflict of Interest
We have no conflicts of interest to disclose.
Acknowledgements
This manuscript was supported by the US Department of Veterans Affairs Office of Rural Health for the Geriatric Research Education and Clinical Center (GRECC) Connect clinical demonstration project.
The views expressed are those of the authors and do not necessarily reflect the positions or policies of the US Department of Veterans Affairs or the United States Government.
The authors thank each of the 15 GRECC Connect hub sites for their contributions to the cross-site evaluation. Additionally, they thank Shatice Jones and Eileen Dryden, PhD, for assistance with the RE-AIM (Reach, Effectiveness, Adoption, Implementation and Maintenance) evaluation and Elizabeth Staton for assistance with manuscript revisions.