-
PDF
- Split View
-
Views
-
Cite
Cite
Rabiya S. Tuma, Split Prostate Cancer Four Ways, Willett Says, JNCI: Journal of the National Cancer Institute, Volume 98, Issue 14, 19 July 2006, Pages 959–960, https://doi.org/10.1093/jnci/djj317
Close - Share Icon Share
Researchers recognize that aggressive and slow-growing prostate cancers are probably different entities, and data suggest that the risk factors for developing the two types differ as well. Now, Walter Willett , M.D., Dr.P.H., and colleagues are proposing that the causes of prostate cancer in younger men differ from the causes of the disease in older men. If their hypothesis is correct, then researchers will have to divide prostate cancer cases four ways—aggressive versus nonaggressive and younger versus older age of onset—to identify risk factors associated with the disease.
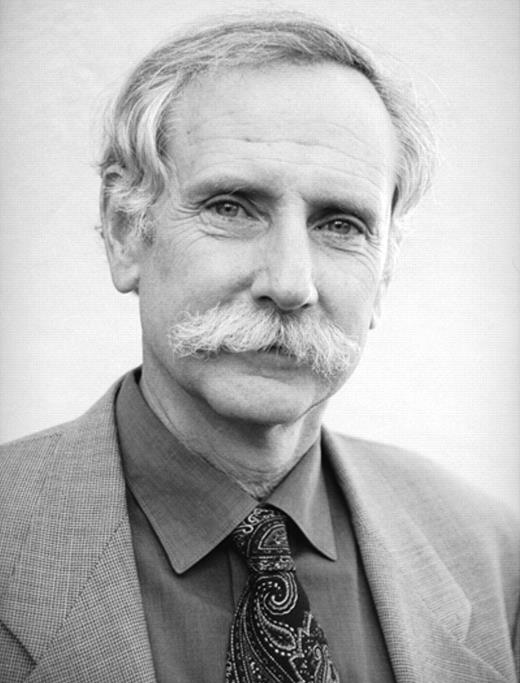
Walter Willett
Historical data and results from the ongoing Health Professionals Follow-Up Study already suggest that the cause of the disease differs between these younger and older men, said Willett, chairman of the department of nutrition and professor of medicine at Harvard School of Public Health in Boston. For example, several studies have suggested that high dairy consumption or calcium intake increases the risk of aggressive disease, but it has no effect on the risk of organ-confined disease. Moreover, researchers have found that a high body mass index protects against prostate cancer during a man's early years, producing as much as a 50% reduction in risk of disease when a man's body mass index at age 21 is considered, but it is associated with a modest increase in risk of disease in men more than age 60.
Looking at this sort of data and recognizing that a man's physiology changes dramatically with increasing age, Willett and Edward Giovannucci, M.D., Sc.D., professor of nutrition and epidemiology at the Harvard School of Public Health, hypothesize that hormones play a substantial role in disease that occurs in younger men, whereas inflammation is more important in cancers that occur later in a man's life.
“For better or worse, aging is like a slow castration process. Our endogenous hormones, particularly our anabolic hormones like testosterone and insulin-like growth factor, decline,” said Willett, while presenting the hypothesis at the American Association for Cancer Research annual meeting earlier this year.
Other facts also support this model. As men age, they carry more fat, which secretes inflammatory factors. And moderate exercise, which can improve insulin resistance and thus inflammation, lowers an older man's risk of disease but appears to have little or no benefit in younger men. Not all risk factors have such dramatically different effects on young and old men. For example, men of all ages may benefit from taking the antioxidant lycopene, with the risk of disease dropping with increased consumption. However, men over 65 appear to derive more benefit than men younger than that age, according to Willett and colleagues' studies (relative risk = 0.67 for older men and 0.89 for younger men). Because lycopene helps reduce damage caused by inflammation, these data further support the idea that inflammation plays a larger role in late-onset disease than early-onset cases, Willet said.
“I would have thought it was the opposite,” said William Nelson, M.D., Ph.D., professor of oncology and associate director of translational research at Johns Hopkins University in Baltimore. He thinks that inflammation probably plays a role in whether prostate cancer develops at all, whereas androgen hormones might determine the aggressiveness of the disease. Moreover, it is not clear to him what role age plays in the disease. For example, he said, one series of autopsies showed that as many as 30% of 30-year-old men have evidence of prostate cancer.
Implications for Study Design
Even if Willett's hypothesis is correct, demonstrating it will not be straightforward. One problem is that knowing exactly at what age to divide the data is not clear. In breast cancer, a disease that differs substantially between younger and older patients, researchers and clinicians use menopause as the distinguishing marker. Men don't have a clear sign of hormonal changes, however, making the cutoff age for young versus old disease somewhat arbitrary. Also, Gleason score and tumor stage, which are often used to identify aggressive cases in case–control studies, are not perfect markers. What researchers really want to know is which cancers will become life threatening. For that, patients need to be followed up for years after diagnosis, an approach that has not traditionally been included in case-control studies of prostate cancer. Also, if patients would need to be split into four groups rather than just two, studies may have to be larger to maintain adequate power.
“The big problem is that there is this sea of prostate cancer out there, the vast majority of which are nonaggressive cases. If something is primarily seen in the aggressive cases, which are the ones we care about most, we will very often miss it,” Willett said. Some risk factors may increase the likelihood of aggressive disease in both young and old men, whereas other factors may affect only one age group or the other. If that is the case, then “cutting the data in one dimension would be adequate for some risk factors, but not for others,” he said.
Cutting up the data might have one advantage in picking out the factors that increase the risk of early-onset disease. As it stands now, almost all cases are identified in older men, so a factor affecting younger men's risk could be diluted. In that situation, dividing the study population may actually enhance the power because the effect is not masked by the older-onset cases.
“I think having these hypotheses out there is important. This is the perfect time to have these debates,” Nelson said.
Data from the Health Professionals Follow-Up Study, which includes more than 52,000 men, and from SELECT (the Selenium and Vitamin E Cancer Prevention Trial), which includes nearly 36,000 men, should help answer some of these questions. Both trials include dietary data, and the Health Professionals study allows case patients to be monitored after diagnosis.
Willett says that monitoring patients after diagnosis is key in epidemiological studies of prostate cancer. Not only is it the best way to know which cases are truly aggressive, but it could enable researchers to identify behavioral risk factors that drive the disease to an aggressive state. With prostate-specific antigen detection, physicians identify prostate cancer early in the disease process. That means that if researchers can identify behaviors and risk factors associated with an increased likelihood of disease progression, they might be able to intervene in the disease course, after the initial diagnosis. “We have a huge window of time to make a difference,” Willett said. To take advantage of that opportunity, Willett and others need to first identify the risk factors involved, in both young and old men.