-
PDF
- Split View
-
Views
-
Cite
Cite
Dominik Berliner, Johann Bauersachs, New drugs: big changes in conservative heart failure therapy?, European Journal of Cardio-Thoracic Surgery, Volume 55, Issue Supplement_1, June 2019, Pages i3–i10, https://doi.org/10.1093/ejcts/ezy421
Close - Share Icon Share
Summary
During the last 20 years, the prognosis for heart failure (HF) with reduced ejection fraction has steadily improved due to advances in drug treatment and the consistent implementation of guideline-recommended evidence-based drug therapy. Nevertheless, the morbidity and mortality rates of patients with HF can still be improved. The prevalence of HF is high and continues to increase steadily. Thus, timely and efficient drug treatment plays a central role in improving the quality of life and prognosis for patients with HF. Current therapeutic concepts combine inhibition of the renin–angiotensin–aldosterone system with blockage of the sympathetic system. New therapeutic approaches such as selective heart rate reduction, attenuation of the degradation of natriuretic peptides by neutral endopeptidase inhibition and treatment of comorbidities (e.g. iron deficiency, diabetes mellitus, hyperkalaemia) have led to a further improvement in the survival, time-out-of hospital and quality of life of affected patients. The goal of this article was to give an overview of the current standard drug therapy for HF and the value of new therapeutic approaches implemented in recent years.
SCOPE OF THE PROBLEM
Heart failure (HF) is one of the most frequent causes of death and hospital admissions in developed countries. The prevalence of HF is estimated to be 1–2% in the western world, and the incidence approaches 5–10 per 1000 persons per year [1]. Numbers estimating the occurrence of HF in the developing world are scarce. The prevalence of HF increases with age from <1% in the age group <55 years to approximately 10% in octogenarians [1]. A substantial increase of the prevalence of HF is predicted in the coming years.
If HF is left untreated, the prognosis is disastrous [2]. The introduction of new drugs and the consequent implementation of evidence-based recommendations of the HF guidelines have led to a reduction in mortality rates and in the frequency of hospitalizations in patients with HF with reduced ejection fraction (HFrEF) during the past few years [3]. However, the outcome of patients with HFrEF can still be improved: approximately 50% of people diagnosed with HF die within 5 years [4]. Furthermore, European data from the European Society of Cardiology (ESC)-HF pilot study show a 17% 12-month all-cause mortality rate and a 44% 12-month rehospitalization rate for hospitalized patients with HF [5].
Three different types of HF have to be distinguished based on the left ventricular ejection fraction (LVEF) because evidence for therapy in HF depends on the respective form [3]:
HFrEF: LVEF <40%,
HF with midrange ejection fraction: LVEF 40–49% and signs of diastolic dysfunction and
HF with preserved ejection fraction: LVEF ≥50% and signs of diastolic dysfunction.
All types of HF are associated with a deterioration of stroke volume and of cardiac output. There is no clear recommendation for the treatment of patients with HF with midrange ejection fraction in the current guidelines because of a lack of studies on the topic. Furthermore, to date no treatment strategies have shown significant improvement in outcome in patients with HF with preserved ejection fraction.
HF describes a complex clinical syndrome that is characterized by the heart’s inability to pump enough blood to ensure the body’s metabolic requirements or only at the cost of abnormally elevated diastolic volumes or pressures [6].
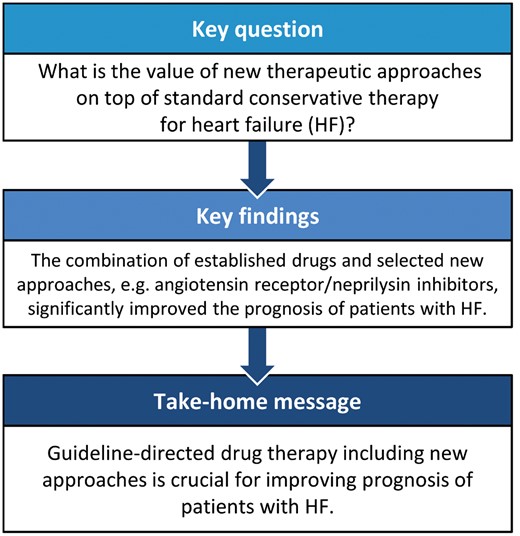
As a result of an ‘initial’ cardiac injury, structural, neurohumoral, cellular and molecular mechanisms are activated to maintain haemodynamic functioning, which leads to volume overload, increased sympathetic activity, cardiac remodelling and inflammatory processes that result in a vicious circle with a constantly aggravating progression. The aim of pharmacological management of HF is to interrupt those deleterious maladaptive processes. Apart from treating the underlying causes (e.g. with valvular surgery), the basic principle of HFrEF treatment is neurohumoral inhibition by means of angiotensin converting enzyme (ACE)-inhibitors (ACEi), angiotensin-II receptor blockers (ARB), or angiotensin receptor/neprilysin inhibitors (ARNI), as well as mineralocorticoid receptor antagonists (MRA) and beta-blockers (Fig. 1). Many randomized trials have demonstrated the efficacy of these therapeutic approaches.
Therapeutic algorithm for a patient with symptomatic heart failure with reduced ejection fraction according to the current guidelines from the European Society of Cardiology (from [3]); green indicates a class I recommendation; yellow indicates a class IIa recommendation. aSymptomatic New York Heart Association class II–IV. bHFrEF LVEF <40%. cIf ACEi not tolerated/contraindicated, use ARB. dIf MR antagonist not tolerated/contraindicated, use ARB. eWith a hospital admission for HF within the last 6 months or with elevated natriuretic peptides (BNP >250 pg/ml or NT-proBNP >500 pg/ml in men and 750 pg/ml in women). fWith an elevated plasma natriuretic peptide level (BNP ≥150 pg/ml or plasma NT-proBNP ≥600 pg/ml, or if HF hospitalization within recent 12 months, plasma BNP ≥100 pg/ml or plasma NT-proBNP ≥400 pg/ml). gIn doses equivalent to enalapril 10 mg twice daily. hWith a hospital admission for HF within the previous year. iCRT is recommended if QRS ≥130 ms and left bundle branch block (in sinus rhythm). jCRT should/may be considered if QRS ≥130 ms with non-left bundle branch block (in sinus rhythm) or for patients in atrial fibrillation provided a strategy to ensure biventricular capture in place (individualized decision). ACEi: angiotensin-converting enzyme inhibitor; ARB: angiotensin receptor blocker; ARNI: angiotensin receptor-neprilysin inhibitor; BNP: B-type natriuretic peptide; CRT: cardiac resynchronization therapy; HF: heart failure; HFrEF: heart failure with reduced ejection fraction; H-ISDN: hydralazine and isosorbide dinitrate; HR: heart rate; ICD: implantable cardioverter-defibrillator; LVAD: left ventricular assist device; LVEF: left ventricular ejection fraction; MR: mineralocorticoid receptor; NT-proBNP: N-terminal pro-B type natriuretic peptide; OMT: optimal medical therapy; VF: ventricular fibrillation; VT: ventricular tachycardia. This image/content is not covered by the terms of the Creative Commons licence of this publication. For permission to reuse, please contact the rights holder.
INHIBITION OF THE RENIN–ANGIOTENSIN–ALDOSTERONE SYSTEM
Low cardiac output activates the renin–angiotensin–aldosterone system (RAAS), which in combination with activation of the adrenergic system, aims for maintenance of blood pressure and reabsorption of sodium and water: renin is released by activation of the baroreceptors in the renal vasculature and induces the conversion from angiotensinogen to angiotensin-I, which is cleaved to angiotensin-II (AT-II) by the ACE [6]. AT-II is a potent vasoconstrictor and leads to an excessive increase in systemic resistance. In addition, it causes an increased release of norepinephrine from the adrenergic nervous system. Furthermore, AT-II may lead to the direct modification of the myocardial structure and function. Also, it is a potent stimulator of various signalling pathways among others involved in the regulation of the extracellular matrix formation [6].
The synthesis of aldosterone is regulated by AT-II and by plasma potassium. Aldosterone causes reabsorption of sodium and plays an important role in cardiac remodelling, development of myocardial hypertrophy, ventricular remodelling, myocardial ischaemia, reduced coronary blood flow, fibroblast proliferation and collagen deposition [6, 7]. These changes increase the passive stiffness of the ventricle, interact with the ventricular filling and reduce arterial compliance [6]. ACEi and MRA inhibit those deleterious effects.
Angiotensin-converting enzyme inhibitors and angiotensin-II receptor antagonists
The positive effects of ACEi on mortality and morbidity in patients with HFrEF have been repeatedly shown in several studies [e.g. CONSENSUS (Cooperative North Scandinavian Enalapril Survival Study) [8], SOLVD (Studies of Left Ventricular Dysfunction) [9]]. Therefore, ACEi have been established in the HF guidelines for many years and are recommended for every patient with HFrEF (class IA indication). Data from the ATLAS (Assessment of Treatment with Lisinopril and Survival) trial [10] indicated that a high dose has a positive impact on the frequency of hospitalizations. Lately, the results of the BIOSTAT-CHF (BIOlogy Study to TAilored Treatment in Chronic Heart Failure) trial [11] confirmed the effect of adequate dosages beyond showing a positive impact on the mortality rate. Despite the explicit recommendation for up-titration to the target dose (Table 1) or the maximum tolerated dose, real-life doses are frequently below the recommended doses [12].
Overview of the recommended dosages for evidence-based heart failure drugs in the current guidelines of the European Society of Cardiology (from [3])
| . | Starting dose (mg) . | Target dose (mg) . |
|---|---|---|
| ACEi | ||
| Captopril | 6.25 t.i.d. | 50 t.i.d. |
| Enalapril | 2.5 b.i.d. | 10–20 b.i.d. |
| Lisinopril | 2.5–5.0 o.d. | 20–35 o.d. |
| Ramipril | 2.5 o.d. | 10 o.d. |
| Trandolapril | 0.5 o.d. | 4 o.d. |
| Beta-blockers | ||
| Bisoprolol | 1.25 o.d. | 10 o.d. |
| Carvedilol | 3.125 b.i.d. | 25 b.i.d. |
| Metoprolol succinate (CR/XL) | 12.5–25 o.d. | 200 o.d. |
| Nebivolol | 1.25 o.d. | 10 o.d. |
| ARBs | ||
| Candesartan | 4–8 o.d. | 32 o.d. |
| Valsartan | 40 b.i.d. | 160 b.i.d. |
| Losartan | 50 o.d. | 150 o.d. |
| MRAs | ||
| Eplerenone | 25 o.d. | 50 o.d. |
| Spironolactone | 25 o.d. | 50 o.d. |
| ARNI | ||
| Sacubitril/valsartan | 49/51 b.i.d. | 97/103 b.i.d. |
| If-channel blocker | ||
| Ivabradine | 5 b.i.d. | 7.5 b.i.d. |
| . | Starting dose (mg) . | Target dose (mg) . |
|---|---|---|
| ACEi | ||
| Captopril | 6.25 t.i.d. | 50 t.i.d. |
| Enalapril | 2.5 b.i.d. | 10–20 b.i.d. |
| Lisinopril | 2.5–5.0 o.d. | 20–35 o.d. |
| Ramipril | 2.5 o.d. | 10 o.d. |
| Trandolapril | 0.5 o.d. | 4 o.d. |
| Beta-blockers | ||
| Bisoprolol | 1.25 o.d. | 10 o.d. |
| Carvedilol | 3.125 b.i.d. | 25 b.i.d. |
| Metoprolol succinate (CR/XL) | 12.5–25 o.d. | 200 o.d. |
| Nebivolol | 1.25 o.d. | 10 o.d. |
| ARBs | ||
| Candesartan | 4–8 o.d. | 32 o.d. |
| Valsartan | 40 b.i.d. | 160 b.i.d. |
| Losartan | 50 o.d. | 150 o.d. |
| MRAs | ||
| Eplerenone | 25 o.d. | 50 o.d. |
| Spironolactone | 25 o.d. | 50 o.d. |
| ARNI | ||
| Sacubitril/valsartan | 49/51 b.i.d. | 97/103 b.i.d. |
| If-channel blocker | ||
| Ivabradine | 5 b.i.d. | 7.5 b.i.d. |
ACEi: angiotensin-converting enzyme inhibitor; ARB: angiotensin receptor blocker; ARNI: angiotensin receptor-neprilysin inhibitor; b.i.d.: twice daily; MRA: mineralocorticoid receptor antagonist; o.d.: once daily; t.i.d.: 3 times a day. This content is not covered by the terms of the Creative Commons licence of this publication. For permission to reuse, please contact the rights holder.
Overview of the recommended dosages for evidence-based heart failure drugs in the current guidelines of the European Society of Cardiology (from [3])
| . | Starting dose (mg) . | Target dose (mg) . |
|---|---|---|
| ACEi | ||
| Captopril | 6.25 t.i.d. | 50 t.i.d. |
| Enalapril | 2.5 b.i.d. | 10–20 b.i.d. |
| Lisinopril | 2.5–5.0 o.d. | 20–35 o.d. |
| Ramipril | 2.5 o.d. | 10 o.d. |
| Trandolapril | 0.5 o.d. | 4 o.d. |
| Beta-blockers | ||
| Bisoprolol | 1.25 o.d. | 10 o.d. |
| Carvedilol | 3.125 b.i.d. | 25 b.i.d. |
| Metoprolol succinate (CR/XL) | 12.5–25 o.d. | 200 o.d. |
| Nebivolol | 1.25 o.d. | 10 o.d. |
| ARBs | ||
| Candesartan | 4–8 o.d. | 32 o.d. |
| Valsartan | 40 b.i.d. | 160 b.i.d. |
| Losartan | 50 o.d. | 150 o.d. |
| MRAs | ||
| Eplerenone | 25 o.d. | 50 o.d. |
| Spironolactone | 25 o.d. | 50 o.d. |
| ARNI | ||
| Sacubitril/valsartan | 49/51 b.i.d. | 97/103 b.i.d. |
| If-channel blocker | ||
| Ivabradine | 5 b.i.d. | 7.5 b.i.d. |
| . | Starting dose (mg) . | Target dose (mg) . |
|---|---|---|
| ACEi | ||
| Captopril | 6.25 t.i.d. | 50 t.i.d. |
| Enalapril | 2.5 b.i.d. | 10–20 b.i.d. |
| Lisinopril | 2.5–5.0 o.d. | 20–35 o.d. |
| Ramipril | 2.5 o.d. | 10 o.d. |
| Trandolapril | 0.5 o.d. | 4 o.d. |
| Beta-blockers | ||
| Bisoprolol | 1.25 o.d. | 10 o.d. |
| Carvedilol | 3.125 b.i.d. | 25 b.i.d. |
| Metoprolol succinate (CR/XL) | 12.5–25 o.d. | 200 o.d. |
| Nebivolol | 1.25 o.d. | 10 o.d. |
| ARBs | ||
| Candesartan | 4–8 o.d. | 32 o.d. |
| Valsartan | 40 b.i.d. | 160 b.i.d. |
| Losartan | 50 o.d. | 150 o.d. |
| MRAs | ||
| Eplerenone | 25 o.d. | 50 o.d. |
| Spironolactone | 25 o.d. | 50 o.d. |
| ARNI | ||
| Sacubitril/valsartan | 49/51 b.i.d. | 97/103 b.i.d. |
| If-channel blocker | ||
| Ivabradine | 5 b.i.d. | 7.5 b.i.d. |
ACEi: angiotensin-converting enzyme inhibitor; ARB: angiotensin receptor blocker; ARNI: angiotensin receptor-neprilysin inhibitor; b.i.d.: twice daily; MRA: mineralocorticoid receptor antagonist; o.d.: once daily; t.i.d.: 3 times a day. This content is not covered by the terms of the Creative Commons licence of this publication. For permission to reuse, please contact the rights holder.
ARB are an alternative for patients who do not tolerate ACEi due to cough or angioedema.
Direct renin inhibition
A few years ago, the idea surfaced to directly inhibit renin and thus prevent RAAS activation. In the ASTRONAUT (Aliskiren Trial on Acute Heart Failure Outcomes) trial [13], the value of aliskiren, a direct renin inhibitor, in the treatment of HFrEF was analysed. The addition of aliskiren on top of standard HF medication did not reduce cardiovascular mortality or HF rehospitalizations compared to placebo in patients after hospitalization for HF. In the ATMOSPHERE (Aliskiren Trial to Minimize Outcomes in Patients with Heart Failure) trial [14] treatment with aliskiren was compared to therapy with enalapril and to the combination of both in patients with stable chronic HF. The combination of aliskiren and enalapril led to more adverse events. Furthermore, the authors were not able to prove that aliskiren alone was non-inferior in comparison to enalapril. Therefore, aliskiren is currently not recommended for HF therapy.
Mineralocorticoid receptor antagonists
The first trials on MRA inpatients with HF included patients with advanced symptoms [New York Heart Association (NYHA) class III–IV, RALES (Randomized Aldactone Evaluation Study) [15]] or after myocardial infarction [EPHESUS (Eplerenone Post-AMI Heart Failure Efficacy and Survival) trial [16]] and showed significant benefits for such patients. Following publication of the EMPHASIS-HF (Eplerenone in Mild Patients Hospitalization and Survival Study in Heart Failure) trial [17], which enrolled patients with mild symptoms (NYHA class II) and which was able to show significantly lower rates of cardiovascular mortality and hospitalizations in the group receiving eplerenone compared to placebo, the indication for use of MRA was extended to all symptomatic patients with HFrEF [3].
Different MRA have different affinities for the mineralocorticoid receptor, the glucocorticoid receptor, the androgen receptor and the progesterone receptor and thus, different side effects: in contrast to eplerenone, spironolactone is a non-selective MRA that additionally activates progesterone and androgen receptors, leading to gynaecomastia, impotence and menstrual disorders, which are frequent causes of non-adherence [18]. In addition, the blood pressure-lowering effect is stronger with spironolactone than with eplerenone. In addition, finerenone is a new non-steroidal MRA with high selectivity for the mineralocorticoid receptor whose impact in HF treatment has to be determined in suitable trials [19].
Angiotensin receptor-neprilysin inhibitor
ARNI combine the established inhibition of the RAAS with the inhibition of the degradation of endogenously released natriuretic peptides (NP). NP are released to the circulation as cardiomyocytes are stretched. Typically, they
raise intracellular cyclic guanosine monophosphate (cGMP),
increase natriuresis,
reduce renin secretion in the kidneys and
attenuate AT-II induced hypertrophic signalling in cardiomyocytes [20].
LCZ696 is a combination of the ARB valsartan and the neprilysin inhibitor sacubitril. Neprilysin (syn. neutral endopeptidase, NEP) is an endopeptidase that degrades natriuretic peptides and several other vasoactive substances (e.g. bradykinin, endothelin-1, adrenomedullin).
The efficacy of this concept was proven by the PARADIGM-HF (Prospective comparison of ARNI with ACEi to Determine Impact on Global Mortality and morbidity in Heart Failure) trial. The main inclusion criteria consisted of symptomatic HFrEF (NYHA II–IV; LVEF ≤40%, during the course of the study changed to ≤35%); brain natriuretic peptide (BNP) ≥150 pg/ml or N-terminal proBNP (NT-proBNP) ≥600 pg/ml (≥100, respectively, 400 pg/ml with an HF hospitalization in the previous 12 months); and estimated glomerular filtration rate ≥30 ml/min/1.73 m2.
A total of 8442 ambulatory patients with HFrEF were randomized to either sacubitril/valsartan or enalapril [21]. Treatment with sacubitril/valsartan led to a significant reduction in the primary end point-cardiovascular deaths and HF hospitalizations (−20%). In addition, cardiovascular deaths (−20%), all-cause deaths (−16%) and HF hospitalizations (−21%) were significantly improved [21].
In the current ESC guidelines, sacubitril/valsartan is recommended for all patients who would have met the inclusion criteria and who remain symptomatic despite treatment with an ACEi (or ARB), a beta-blocker and a MRA (class IB recommendation) [3].
When changing from an ACEi to sacubitril/valsartan, intake of the ACEi should be stopped at least 36 h before the first intake of sacubitril/valsartan because both substances, neprilysin and ACEi, degrade bradykinin. So, simultaneous intake of an ACEi and sacubitril might result in the accumulation of bradykinin and thus the occurrence of severe angioedema. Switching from an ARB to sacubitril/valsartan can be done without delay.
Because neprilysin also degrades amyloid-β [20], its inhibition might result in the accumulation of amyloid-β isoforms and increase the risk of contracting Alzheimer disease. Genetic mutations in the NEP gene have been shown to be associated with an increase in the incidence of Alzheimer disease [22]. Subanalyses of the PARADIGM-HF trial did not indicate any increased risk for the development of dementia [23]. In this regard, a new trial is in the recruiting phase: the PERSPECTIVE (Efficacy and Safety of LCZ696 Compared to Valsartan on Cognitive Function in Patients With Chronic Heart Failure and Preserved Ejection Fraction) trial will clarify whether or not the 2 investigational drugs (LCZ696 and valsartan) have a different effect on brain power and memory.
Recent subanalyses of the PARADIGM-HF trial indicate that the incidence of repeated hospitalizations for worsening HF is reduced by sacubitril/valsartan [24] as well as by the incidence of overt diabetes [25] and hyperkalaemia [26]. Another trial revealed that the rate of ventricular tachyarrhythmias was lower in patients taking sacubitril/valsartan compared to standard angiotensin inhibition (ACEi or ARB) [27]. Furthermore, even in patients with low blood pressure during treatment with sacubitril/valsartan, prognosis was better than during treatment with enalapril [28]. Quality of life is significantly better with treatment with sacubitril/valsartan [29]. In fact, it was recently shown that this effect occurs early after the treatment is switched (Khariton Y. et al., Heart Failure 2018 and World Congress on Acute Heart Failure, Late breaking clinical trials—not yet published).
Hyperkalaemia as a side effect of renin–angiotensin–aldosterone system inhibition
A typical side effect, especially in elderly patients undergoing therapy with RAAS inhibitors and MRA, is the onset of hyperkalaemia. MRA should be used carefully in patients with advanced renal dysfunction or existing hyperkalaemia (potassium >5.0 mmol/l). Renal markers and electrolytes should be supervised regularly. Nevertheless, also older patients (≥75 years) and patients with moderately impaired renal function benefit from treatment with eplerenone [17, 30].
Recurrent hyperkalaemia in some patients prevents reaching target doses of the ACEi or ARB and/or to start or continue treatment with an MRA. The new potassium binder patiromer was recently introduced. Patiromer is a polymer that is not absorbed and acts as an ion exchanger in the colon. Potassium is exchanged with calcium and secreted with the faeces. Thus, patiromer might help in establishing and maintaining adequate levels of HF medication with both ACEi and MRA.
The PEARL-HF (Evaluation of Patiromer in Heart Failure Patients) study enrolled a total of 105 patients with hyperkalaemia who had discontinued HF medications or were unable to achieve adequate doses of HF medications. With the additional intake of patiromer, the potassium levels were significantly lowered and the target dosages of HF medications were achieved significantly more frequently than with placebo [31]. The effect was confirmed in patients with chronic kidney disease and with HFrEF [32]. Additional studies are now required to further define the role of patiromer in the treatment of HF.
INHIBITION OF THE ADRENERGIC SYSTEM AND HEART RATE REDUCTION
As a result of reduced cardiac output in HF, sympathetic activation is induced that leads to a short period of improved peripheral perfusion because of an increased heart rate and enhanced contractility [6]. Prolonged sympathetic activation, however, is typically characterized by several deleterious effects (from [6]):
induction of tachyarrhythmia,
tachycardia (subendocardial ischaemia, reduced diastolic filling time, negative inotropy),
increased renin secretion,
altered myocardial metabolism,
left ventricular and myocyte remodelling (myocardial hypertrophy, fibroblast hyperplasia),
abnormal transduction of the beta-adrenergic signal,
altered myocardial gene expression and
acceleration of myocyte death.
To prevent continuing deterioration of myocardial structure and function due to ongoing sympathetic activation, treatment with a beta-blocker is recommended in all patients with HFrEF.
Beta-blocker
Several studies have shown the efficacy of beta-blocker therapy in HFrEF with respect to mortality and HF hospitalizations, e.g. for bisoprolol [CIBIS II (Cardiac Insufficiency Bisoprolol Study II) trial [33]], carvedilol [COPERNICUS (Carvedilol Prospective Randomized Cumulative Survival) trial [34]], metoprolol succinate [MERIT-HF (Metoprolol CR/XL Randomized Intervention Trial in Congestive Heart Failure) [35]] and nebivolol [SENIORS (Study of the Effects of Nebivolol Intervention on Outcomes and Rehospitalisations in Seniors with Heart Failure) trial [36]]. Similar to RAAS, inhibition dosages of beta-blocker should be increased to the recommended target dose (Table 1). The aforementioned BIOSTAT-CHF trial has shown the positive effects of such a strategy [11].
Beta-blockers are contraindicated in patients with relevant bradycardia and second- or third-degree heart block (without a pacemaker) and bronchial asthma. Stable chronic obstructive lung disease is usually not a contraindication to treatment with a beta-blocker.
In a recent analysis concerning the impact of beta-blockade on mortality, no significant differences were found among the varying substances [bisoprolol versus carvedilol: hazard ratio (HR) 0.90, 95% confidence interval (CI) 0.76–1.06; P = 0.20; bisoprolol versus metoprolol succinate HR 1.10, 95% CI 0.93–1.31; P = 0.24; carvedilol versus metoprolol succinate HR 1.08, 95% CI 0.95–1.22; P = 0.26] [37].
If-channel inhibitor ivabradine
Ivabradine acts through inhibition of the If-channel, highly expressed in the sinoatrial node in a dose-dependent manner [38]. Inhibition of the If-channel leads to deceleration of the heart rate.
In the SHIFT trial (NYHA classes II–IV, LVEF ≤35%, sinus rhythm with heart rate ≥70 bpm), treatment with ivabradine in addition to guideline-recommended HF therapy including a beta-blocker led to a significant reduction in the primary end point (HF hospitalizations and cardiovascular deaths) [39]. Beyond that, a substudy of the SHIFT (Systolic Heart Failure Treatment with the If inhibitor ivabradine) trial revealed a significant enhancement in left ventricular function and reduction in left ventricular volumes [40] in patients receiving ivabradine. Furthermore, quality of life was significantly improved [41].
In the current ESC guidelines, ivabradine is recommended for patients with HFrEF (LVEF ≤35%) in sinus rhythm with a heart rate ≥70 bpm and persisting symptoms despite therapy with an ACEi (or ARB), a beta-blocker and a MRA [3].
Cardiac glycosides
Cardiac glycosides have been part of HF therapy for decades, but their status in modern HF management is uncertain. One randomized trial analysing their role in HF was performed in the 1990s—which means before the implementation of the current standard in HF therapy. The results of the DIG (Digitalis Investigation Group) trial [42] were interpreted as neutral because the total number of deaths, the prespecified primary end point, was not influenced by therapy with digoxin (HR 0.99, 95% CI 0.91–1.07; P = 0.80). However, treatment with digoxin led to a significant reduction in HF hospitalizations (HR 0.72, 95% CI 0.66–0.79; P < 0.001) and a trend towards fewer HF-associated deaths (HR 0.88, 95% CI 0.77–1.01; P = 0.06). Later subgroup analyses demonstrated a mortality benefit for patients with lower serum levels of digoxin (0.5–0.9 ng/ml) compared to patients with high levels, who had an increased mortality rate [43].
Digoxin is excreted mainly by the kidneys; thus, digoxin accumulates in patients with moderate or advanced renal dysfunction. The alternative cardiac glycoside digitoxin is less dependent on kidney function. Therefore, therapy with digitoxin seems advisable in patients with impaired renal function due to the narrow therapeutic range of glycosides [44]. To date, there are no data on the impact of digitoxin in the context of HF. A large randomized study investigating the role of digitoxin in patients with HF on contemporary drug therapy is under way: the DIGIT-HF trial (DIGitalis to Improve OuTcomes in patients with advanced systolic chronic Heart Failure, EudraCT-Nr.: 2013-005326-38).
Besides, there are no data from randomized trials regarding the value of either digoxin or digitoxin in patients with HF and concomitant atrial fibrillation. Because there was an indication in the DIG trial of an increased mortality at high levels of digitalis, the corresponding serum level should be determined approximately 4–6 weeks after the patient starts therapy with a cardiac glycoside (target level: 0.5–0.9 ng/ml for digoxin and 8–18 ng/ml for digitoxin) [3, 44]. An improved prognosis in patients with HF taking digoxin at currently recommended dosages may not be related to its inotropic effect but to a beneficial neurohumoral modulation [44].
GENERAL CONSIDERATIONS
The significance of the aforementioned therapies and their combinations has just been investigated in a meta-analysis [45]. The most effective combinations of drugs used to treat patients with HFrEF were a mixture of ARNI, a beta-blocker and MRA (62% reduction in the mortality rate versus that with placebo) and a mixture of ACEi, a beta-blocker, MRA and ivabradine (59% reduction in the mortality rate versus that with placebo). An overview of the impact of the different therapies and their combinations on outcome is summarized in Table 2. Overall, the use of combinations of HF drugs has significantly improved outcomes in patients with HFrEF. Current recommendations of the ESC for the treatment of patients with HFrEF with drugs are depicted in Fig. 1.
Impact of heart failure medications and their combinations on outcome (treatment effect versus placebo; from [45] with permission)
| . | All-cause mortality . | Cardiovascular mortality . | All-cause hospitalization . | Hospitalization for HF . |
|---|---|---|---|---|
| ARNI + BB + MRA | 0.38 (0.20–0.65) | 0.36 (0.16–0.71) | 0.58 (0.36–0.92) | 0.27 (0.07–1.07) |
| ACEi + BB + MRA + IVA | 0.41 (0.21–0.70) | 0.41 (0.19–0.82) | 0.58 (0.36–0.92) | 0.25 (0.07–0.99) |
| ACEi + BB + MRA | 0.44 (0.27–0.67) | 0.45 (0.25–0.75) | 0.65 (0.45–0.93) | 0.34 (0.13–0.91) |
| ARB + BB | 0.48 (0.24–0.86) | 0.50 (0.19–1.12) | 0.79 (0.47–1.21) | 0.31 (0.07–1.29) |
| ACEi + ARB + BB | 0.52 (0.32–0.80) | 0.47 (0.24–0.82) | 0.74 (0.46–1.04) | 0.42 (0.16–1.23) |
| ACEi + BB | 0.58 (0.42–0.73) | 0.56 (0.37–0.75) | 0.75 (0.54–0.92) | 0.34 (0.17–0.56) |
| ACEi + MRA | 0.58 (0.36–0.90) | 0.56 (0.31–0.95) | 0.69 (0.45–0.96) | 0.36 (0.12–0.96) |
| BB | 0.58 (0.34–0.95) | 0.62 (0.27–1.32) | 0.86 (0.59–1.18) | 0.45 (0.13–1.39) |
| ACEi + ARB | 0.83 (0.52–1.23) | 0.80 (0.43–1.33) | NA | 0.26 (0.08–0.57) |
| ACEi | 0.84 (0.67–1.01) | 0.81 (0.60–1.04) | 0.89 (0.71–1.05) | 0.52 (0.32–0.76) |
| ARB | 0.89 (0.61–1.27) | 0.85 (0.51–1.28) | 0.81 (0.56–1.01) | 0.53 (0.26–1.03) |
| . | All-cause mortality . | Cardiovascular mortality . | All-cause hospitalization . | Hospitalization for HF . |
|---|---|---|---|---|
| ARNI + BB + MRA | 0.38 (0.20–0.65) | 0.36 (0.16–0.71) | 0.58 (0.36–0.92) | 0.27 (0.07–1.07) |
| ACEi + BB + MRA + IVA | 0.41 (0.21–0.70) | 0.41 (0.19–0.82) | 0.58 (0.36–0.92) | 0.25 (0.07–0.99) |
| ACEi + BB + MRA | 0.44 (0.27–0.67) | 0.45 (0.25–0.75) | 0.65 (0.45–0.93) | 0.34 (0.13–0.91) |
| ARB + BB | 0.48 (0.24–0.86) | 0.50 (0.19–1.12) | 0.79 (0.47–1.21) | 0.31 (0.07–1.29) |
| ACEi + ARB + BB | 0.52 (0.32–0.80) | 0.47 (0.24–0.82) | 0.74 (0.46–1.04) | 0.42 (0.16–1.23) |
| ACEi + BB | 0.58 (0.42–0.73) | 0.56 (0.37–0.75) | 0.75 (0.54–0.92) | 0.34 (0.17–0.56) |
| ACEi + MRA | 0.58 (0.36–0.90) | 0.56 (0.31–0.95) | 0.69 (0.45–0.96) | 0.36 (0.12–0.96) |
| BB | 0.58 (0.34–0.95) | 0.62 (0.27–1.32) | 0.86 (0.59–1.18) | 0.45 (0.13–1.39) |
| ACEi + ARB | 0.83 (0.52–1.23) | 0.80 (0.43–1.33) | NA | 0.26 (0.08–0.57) |
| ACEi | 0.84 (0.67–1.01) | 0.81 (0.60–1.04) | 0.89 (0.71–1.05) | 0.52 (0.32–0.76) |
| ARB | 0.89 (0.61–1.27) | 0.85 (0.51–1.28) | 0.81 (0.56–1.01) | 0.53 (0.26–1.03) |
ACEi: angiotensin-converting enzyme inhibitor; ARB: angiotensin receptor blocker; ARNI: angiotensin receptor-neprilysin inhibitor; BB: beta-blocker; HF: heart failure; IVA: ivabradine; MRA: mineralocorticoid receptor antagonist; NA: not available. This content is not covered by the terms of the Creative Commons licence of this publication. For permission to reuse, please contact the rights holder.
Impact of heart failure medications and their combinations on outcome (treatment effect versus placebo; from [45] with permission)
| . | All-cause mortality . | Cardiovascular mortality . | All-cause hospitalization . | Hospitalization for HF . |
|---|---|---|---|---|
| ARNI + BB + MRA | 0.38 (0.20–0.65) | 0.36 (0.16–0.71) | 0.58 (0.36–0.92) | 0.27 (0.07–1.07) |
| ACEi + BB + MRA + IVA | 0.41 (0.21–0.70) | 0.41 (0.19–0.82) | 0.58 (0.36–0.92) | 0.25 (0.07–0.99) |
| ACEi + BB + MRA | 0.44 (0.27–0.67) | 0.45 (0.25–0.75) | 0.65 (0.45–0.93) | 0.34 (0.13–0.91) |
| ARB + BB | 0.48 (0.24–0.86) | 0.50 (0.19–1.12) | 0.79 (0.47–1.21) | 0.31 (0.07–1.29) |
| ACEi + ARB + BB | 0.52 (0.32–0.80) | 0.47 (0.24–0.82) | 0.74 (0.46–1.04) | 0.42 (0.16–1.23) |
| ACEi + BB | 0.58 (0.42–0.73) | 0.56 (0.37–0.75) | 0.75 (0.54–0.92) | 0.34 (0.17–0.56) |
| ACEi + MRA | 0.58 (0.36–0.90) | 0.56 (0.31–0.95) | 0.69 (0.45–0.96) | 0.36 (0.12–0.96) |
| BB | 0.58 (0.34–0.95) | 0.62 (0.27–1.32) | 0.86 (0.59–1.18) | 0.45 (0.13–1.39) |
| ACEi + ARB | 0.83 (0.52–1.23) | 0.80 (0.43–1.33) | NA | 0.26 (0.08–0.57) |
| ACEi | 0.84 (0.67–1.01) | 0.81 (0.60–1.04) | 0.89 (0.71–1.05) | 0.52 (0.32–0.76) |
| ARB | 0.89 (0.61–1.27) | 0.85 (0.51–1.28) | 0.81 (0.56–1.01) | 0.53 (0.26–1.03) |
| . | All-cause mortality . | Cardiovascular mortality . | All-cause hospitalization . | Hospitalization for HF . |
|---|---|---|---|---|
| ARNI + BB + MRA | 0.38 (0.20–0.65) | 0.36 (0.16–0.71) | 0.58 (0.36–0.92) | 0.27 (0.07–1.07) |
| ACEi + BB + MRA + IVA | 0.41 (0.21–0.70) | 0.41 (0.19–0.82) | 0.58 (0.36–0.92) | 0.25 (0.07–0.99) |
| ACEi + BB + MRA | 0.44 (0.27–0.67) | 0.45 (0.25–0.75) | 0.65 (0.45–0.93) | 0.34 (0.13–0.91) |
| ARB + BB | 0.48 (0.24–0.86) | 0.50 (0.19–1.12) | 0.79 (0.47–1.21) | 0.31 (0.07–1.29) |
| ACEi + ARB + BB | 0.52 (0.32–0.80) | 0.47 (0.24–0.82) | 0.74 (0.46–1.04) | 0.42 (0.16–1.23) |
| ACEi + BB | 0.58 (0.42–0.73) | 0.56 (0.37–0.75) | 0.75 (0.54–0.92) | 0.34 (0.17–0.56) |
| ACEi + MRA | 0.58 (0.36–0.90) | 0.56 (0.31–0.95) | 0.69 (0.45–0.96) | 0.36 (0.12–0.96) |
| BB | 0.58 (0.34–0.95) | 0.62 (0.27–1.32) | 0.86 (0.59–1.18) | 0.45 (0.13–1.39) |
| ACEi + ARB | 0.83 (0.52–1.23) | 0.80 (0.43–1.33) | NA | 0.26 (0.08–0.57) |
| ACEi | 0.84 (0.67–1.01) | 0.81 (0.60–1.04) | 0.89 (0.71–1.05) | 0.52 (0.32–0.76) |
| ARB | 0.89 (0.61–1.27) | 0.85 (0.51–1.28) | 0.81 (0.56–1.01) | 0.53 (0.26–1.03) |
ACEi: angiotensin-converting enzyme inhibitor; ARB: angiotensin receptor blocker; ARNI: angiotensin receptor-neprilysin inhibitor; BB: beta-blocker; HF: heart failure; IVA: ivabradine; MRA: mineralocorticoid receptor antagonist; NA: not available. This content is not covered by the terms of the Creative Commons licence of this publication. For permission to reuse, please contact the rights holder.
SYMPTOMATIC THERAPY AND TREATMENT OF COMORBIDITIES
Diuretics
In addition to this evidence-based therapy, symptom-oriented therapy with diuretics should be used. The goal is to achieve symptom relief (e.g. dyspnoea, oedema, pulmonary congestion) as well as better exercise capacity and quality of life [4]. Loop diuretics are preferred for patients with HFrEF. The goal of diuretic therapy is to achieve and maintain euvolaemia at the lowest possible dose [46]. The possibility of reducing the dosage should be checked regularly. In recent years, the impact of the comorbidities of HF has gained attention. Two comorbidities are of particular interest because of the new drugs.
Iron supplements
Iron deficiency is common in patients with chronic HF [47]. It is an independent risk factor for poor prognosis and is associated with poor performance [3, 48]. A lack of iron causes dysfunction of important proteins in the (cardiac) muscle and leads to anaemia. In patients with HFrEF, several mechanisms seem to lead to an iron deficit, including lack of oral uptake and reduced gastrointestinal absorption as well as increased iron loss [47]. Two clinical trials [FAIR-HF (Ferinject® Assessment in Patients With IRon Deficiency and Chronic Heart Failure) and CONFIRM-HF (Ferric CarboxymaltOse evaluatioN on perFormance in patients with IRon deficiency in coMbination with chronic Heart Failure)] have shown that symptomatic patients with HFrEF with proven iron deficiency (ferritin <100 mg/l or ferritin 100–299 µg/l and transferrin saturation <20%) benefit from iron substitution in terms of quality of life and exercise capacity [49, 50]. The effect was independent from concomitant anaemia [50]. Large randomized studies on the effect on prognosis are not yet available, but in a recent meta-analysis intravenous iron substitution was shown to be associated with a lower risk of hospitalizations in patients with HF [51]. In the current guidelines, intravenous iron therapy is recommended in symptomatic patients with HF with proven iron deficiency [3].
Empagliflozin
Diabetes mellitus is a frequent comorbidity in patients with HFrEF that may adversely affect the course of the disease [52]. Empagliflozin selectively blocks the sodium-glucose cotransporter-2 in the proximal tubule system in the kidneys. Therefore, glucose secretion and thus diuresis are increased. Furthermore, loss of glucose leads to weight loss [53]. Empagliflozin reduces blood pressure via the diuretic effect, has positive effects on the vascular system, reduces low-density lipoprotein cholesterol and can also be used in patients with reduced renal function [53]. In the EMPA-REG-Outcome [(Empagliflozin) Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients] trial, cardiovascular deaths were reduced by treatment with empagliflozin by 38% in patients with diabetes with an increased cardiovascular risk compared to placebo [54]. Besides, the empagliflozin group showed a significantly lower risk of hospitalization for HF (HR 0.65, 95% CI 0.5–0.85; P = 0.002). A subgroup analysis revealed similar results for patients with pre-existing HF [55], so empagliflozin is a promising substance for treatment of patients with HF and concomitant diabetes. In the ongoing EMPEROR programme, empagliflozin is under investigation for treatment of HFrEF and HF with preserved ejection fraction in patients with and without diabetes (ClinicalTrials.gov Identifier: NCT03057951, NCT03057977).
THERAPEUTIC APPROACHES WITH PROMISING BUT NOT YET PROVEN POTENTIAL
Riociguat is a stimulator of the soluble guanylate cyclase (sGC), which is successfully used in the therapy of pulmonary hypertension. Vericiguat also stimulates the activity of the enzyme and thus enhances the production of the signalling molecule cyclic guanosine monophosphate (cGMP) and is actually tested as a potential drug to treat HF. In HF, nitric oxide (NO)-activated sGC and thus also cGMP synthesis are not sufficiently stimulated due to limited NO bioavailability—with unfavourable consequences for vascular function [56]. Therefore, a correction of this deficit by an oral sGC stimulator such as vericiguat might have a clinically favourable effect on HF. In a first trial in patients with worsening chronic HF and reduced LVEF, vericiguat did not have a statistically significant effect on the change in NT-proBNP levels at 12 weeks compared with placebo but was well tolerated [57]. Further clinical trials of vericiguat have to determine the impact of sGC stimulators in the treatment of HF.
Another promising therapeutic approach is the myosin activator omecamtiv mecarbil. Omecamtiv mecarbil extends the cycle-dependent interaction of myosin with actin, thus prolonging the duration of systole and improving cardiac contractility without changing cellular calcium concentration or increasing myocardial oxygen consumption. In the COSMIC-HF (Chronic Oral Study of Myosin Activation to Increase Contractility in Heart Failure) trial, the authors found a significant increase in stroke volume and a decrease in left ventricular end-systolic diameter, left ventricular end-diastolic diameter and N-terminal pro B-type natriuretic peptide concentration in plasma in patients receiving omecamtiv mecarbil compared to placebo [58]. Further studies must elucidate the impact of this drug in the environment of modern HF therapy.
CONCLUSION
The prognosis of patients with HF has been significantly improved due to the combined use of evidence-based drugs during the last 20 years. Therefore, applying these treatment options in patients with HFrEF is crucial. Standard therapy consists of ACEi, a beta-blocker and, in most cases, an MRA as well as diuretics for improvement of symptoms. New concepts like treatment with ARNI have further improved prognosis in patients with HFrEF. The significance of digitalis has actually been elucidated in a large clinical trial. The consequent treatment of comorbidities might lead to a further improvement in outcome in patients with HF.
Funding
This paper was published as part of a supplement supported by an educational grant from Medtronic.
Conflict of interest: Dominik Berliner received honoraria and/or travel support from the following companies and/or is a member of their advisory boards: Novartis, Abbott, Orion Pharma, Daiichi Sankyo, Bayer and Boehringer Ingelheim. Johann Bauersachs received honoraria for lectures and advice from Novartis, Pfizer, Vifor, Bayer, Servier, Orion, CVRx, Abbott and Medtronic and research support from Zoll, CVRx, Bayer, Vifor, Abiomed and Medtronic.
REFERENCES
The CONSENSUS Trial Study Group.
The SOLVD Investigators.
CIBIS-II Investigators and Committees.
Digitalis Investigation Group.



![Therapeutic algorithm for a patient with symptomatic heart failure with reduced ejection fraction according to the current guidelines from the European Society of Cardiology (from [3]); green indicates a class I recommendation; yellow indicates a class IIa recommendation. aSymptomatic New York Heart Association class II–IV. bHFrEF LVEF <40%. cIf ACEi not tolerated/contraindicated, use ARB. dIf MR antagonist not tolerated/contraindicated, use ARB. eWith a hospital admission for HF within the last 6 months or with elevated natriuretic peptides (BNP >250 pg/ml or NT-proBNP >500 pg/ml in men and 750 pg/ml in women). fWith an elevated plasma natriuretic peptide level (BNP ≥150 pg/ml or plasma NT-proBNP ≥600 pg/ml, or if HF hospitalization within recent 12 months, plasma BNP ≥100 pg/ml or plasma NT-proBNP ≥400 pg/ml). gIn doses equivalent to enalapril 10 mg twice daily. hWith a hospital admission for HF within the previous year. iCRT is recommended if QRS ≥130 ms and left bundle branch block (in sinus rhythm). jCRT should/may be considered if QRS ≥130 ms with non-left bundle branch block (in sinus rhythm) or for patients in atrial fibrillation provided a strategy to ensure biventricular capture in place (individualized decision). ACEi: angiotensin-converting enzyme inhibitor; ARB: angiotensin receptor blocker; ARNI: angiotensin receptor-neprilysin inhibitor; BNP: B-type natriuretic peptide; CRT: cardiac resynchronization therapy; HF: heart failure; HFrEF: heart failure with reduced ejection fraction; H-ISDN: hydralazine and isosorbide dinitrate; HR: heart rate; ICD: implantable cardioverter-defibrillator; LVAD: left ventricular assist device; LVEF: left ventricular ejection fraction; MR: mineralocorticoid receptor; NT-proBNP: N-terminal pro-B type natriuretic peptide; OMT: optimal medical therapy; VF: ventricular fibrillation; VT: ventricular tachycardia. This image/content is not covered by the terms of the Creative Commons licence of this publication. For permission to reuse, please contact the rights holder.](https://oup.silverchair-cdn.com/oup/backfile/Content_public/Journal/ejcts/55/Supplement_1/10.1093_ejcts_ezy421/1/m_ezy421f1.jpeg?Expires=1716388823&Signature=10FNG7QuxONdu8HH5JVlYf3sliG~EX-ROy3R1u8hSlaTi4UiTEzItT5dFJisGZtPvnbbFs6c8gTMQggH3q9LL5EFKexKVxd4eJPfapu3PDOLUAzzWhPQSbNsXZa6jQpnVOoe0tjI9MHbLBd3R6rg9XWHLo4KC1WzMHu0swYwKNtQDnj0Nvt753-zNJdjzoLy~EHR8AJHUqqPSyWywHgkeNtX6jzwPVirTOiMZy2pZQS3kccDglolvpXkp0WXoCi-jeyXHHDyLnarpxvf5yIEeRBwdI5KNi0zLMvDSHfuuRl~1mt26cbd-y6usYLi7CcaPuCmtSgZDqlqr343yaxK~Q__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
