Abstract
This article provides a critical and genealogical analysis of the allostatic load research framework. AL research is used as a case study to analyse how the current biosocial context is articulated in the field of health inequalities research. Providing a contemporary analysis of AL studies with a genealogy of the AL concept, we show that the ambition to use biological tools to improve measurements, predictions, and ultimately public health action, is rooted in a history that predates current biosocial entanglements. We analyse the conceptual and methodological grounding of AL studies in relation to the ambitious propositions to address health inequalities they often convey. The difficulties in translating AL research findings into public health policies and the risks of biomedicalisation that could emerge through the use of AL are also addressed. While acknowledging these risks, however, we nuance the risk of depoliticisation associated with the biomedicalisation of social inequalities in health. In light of the historical analysis, we qualify the risks associated to a biologisation of social life that could emerge from AL research: it appears that these risks are more specifically rooted in methodological and epistemological problems that researchers would need to consider in the pursuit of AL research.
Similar content being viewed by others
Introduction
This article is broadly concerned with the relationship between biological and social factors in the development of health inequalities, in the context of growing biosocial research. More specifically, we focus on the developing field of studies which use the allostatic load (hereafter AL) framework. The term refers both to a concept and a subsequent measurement tool, put into use to identify the cumulative physiological impacts of environmental stressors on human health, and tentatively help explain the biological pathways by which social conditions are embodied. The concept is operationalised into a composite score assembling a changing set of biomarkers, which is then correlated with various established measures of social deprivation.
The interest in AL reflects the currently expanding biosocial context, “the present renegotiation of the boundaries between realms commonly demarcated as ‘the social’ and ‘the biological’” (Meloni 2014, p. 593). A vast body of research in various fields aims at understanding how the social environment comes under the skin, shapes individual physiology, and searching for biological mechanisms which govern the embodiment of social conditions.Footnote 1 The quest for molecular mechanisms through which the biological and the social are intimately glued together has garnered increasing attention, notably following research on Developmental Origins of Health and Disease (DoHaD) started in the 1980s and later discoveries in epigenetics. In social epidemiology, the integration of these objectives can be seen in attempts at addressing health disparities by studying the “biology of disadvantage” (Adler and Stewart 2010) or “biology of inequality” (Brunner 1997). In this landscape, AL is construed as a potent tool to unveil the biological mechanisms translating social phenomena into individual and collective physiologies, thus offering results which could help better address health inequalities.
In this article, we use AL research as a case study to explore how biological and social factors are combined in the field of health inequalities research. Our overall argument is articulated around two core propositions:
-
(1)
We analyze the conceptual and methodological grounding of AL studies in relation to the ambitious propositions to address health inequalities they often convey. It is expected that by relating biological measures to other established measurements of social processes, we shall understand how the life-course biological embodiment of social deprivation comes into play in the construction of health inequalities, and that better policies will follow from this improved understanding. We address the difficulties in translating AL research findings into public health policies and the risks of individualistic and reductionistic consequences that could emerge through the use of AL.
-
(2)
At the same time, AL research incorporates a core conceptual genealogy which can be traced back to previous ways of combining the biological and the social that do not necessarily entail those individualistic and reductionist consequences of biomedicalisation. Articulating our contemporary analysis of AL studies with a genealogy of the AL concept, we show that the ambition to use biological tools to improve measurements, predictions, and ultimately public health action, is rooted in a history that predates current biosocial entanglements.
The second section starts with a very brief presentation of AL studies, followed by what we identify as the promises and claims they put forward, and an outline of the risks of biomedicalisation in this field. The third section is dedicated to the historical genealogy of the AL concept, which we use to articulate our analysis of methodological and conceptual issues in AL studies in ‘The narrow path of AL research to meet its social promises’ section.
Allostatic load and the “biosocial turn” in social epidemiology
Allostatic load as an operational measure of stress
The AL concept was introduced by physiologists Bruce McEwen and Eliot Stellar (1993). McEwen’s team, at the Rockefeller University in the USA, alongside collaborators such as Teresa Seeman’s team, at the University of California’s School of Medicine, published in 1997 the first results using AL measurements, based on the MacArthur cohort for ageing studies (Seeman et al. 1997). McEwen expanded the AL conceptual development in an oft-quoted article (McEwen 1998), followed by new promising results based on the same cohort (Seeman et al. 2001). Until the mid-2000s, only a few articles mentioned AL, mostly coming from McEwen’s or Seeman’s teams, sometimes in collaboration with other researchers. Then the field started to expand to new groups of researchers: around 2005 the number of articles grew to ca. 20–30 yearly, and since 2015 to more than a hundred.Footnote 2
Allostatic load refers both to a conceptual framework and to its operationalisation into a measurement tool, taking the form of a multisystem score.Footnote 3 Conceptually, AL can be described as the cumulative impact of environmental stressors on individual physiology. As stress generates adaptive physiological reactions, chronic stress will lead to an alteration of the organism’s response capacity, a “gradual loss of the body’s ability to maintain physiological parameters within normal operating ranges” (Dowd et al. 2009, pp. 1298–1299). The embodiment of this cumulative impact of stressors has been metaphorically described as “wear and tear” in the foundational AL article (McEwen and Stellar 1993, p. 2094), or for other examples as “exact[ing] a toll” (Beckie 2012, p. 312) or a “physiologic stamp on the body” (Szanton et al. 2005, p. 8).
The AL concept thus puts forward a dynamic vision of the interwoven social and biological dimensions of health and disease, rooted in the broad concept of stress. Indeed, the possibility to delineate and grasp this particularly malleable notion is an attractive feature of AL. Stress being an essential cornerstone between the social and the physiological, it seems especially appealing to develop tools to operationalise and quantify it. Empirically, AL is a composite index, which could potentially be described as a meta-biomarker. While partly similar to existing ones such as cardiovascular risk or metabolic syndrome scores, AL is explicitly developed by combining biomarkers from different physiological systems. This multisystem feature is seen as more relevant to quantify the cascading effects of chronic stress on physiological systems. External stressors first generate primary mediators (hypothalamic–pituitary–adrenal axis hormones such as cortisol or epinephrine), which induce the release of secondary metabolic and cardiovascular mediators (blood pressure, glycosylated haemoglobin, or cholesterol). The AL score is constructed with varying sets of biomarkers, measurements, and calculation criteria in different studies. We will return in more detail (‘The narrow path of AL research to meet its social promises’ section) to the methodological issues and criticisms linked to the construction of this composite index.
Current findings and promises of AL studies
AL has been studied in relation to various health outcomes compiled in Guidi et al. (2021). It has been associated with health behaviours (increased AL is linked to smoking or alcohol consumption), or various diseases (linked to increased risk for several cardiovascular diseases, type 2 diabetes, preeclampsia, musculoskeletal disorders, epileptic seizures, chronic migraine, etc.). AL correlations with mental health issues range from higher levels of self-rated stress, depressive and anxiety symptoms (not confirmed by all studies), psychotic disorders and various post-traumatic stress disorders. Adverse childhood experiences have been shown to be associated with high levels of AL in adult life.
Moreover, AL has been associated with various sociodemographic variables (see reviews: Ribeiro et al. 2018; Beckie 2012; Guidi et al. 2021). Studies have shown that higher AL is linked with low socioeconomic status (hereafter SES), low income, living in impoverished neighborhoods or unhealthy environments (traffic, household crowding, low vegetation cover), greater perceived racial or social inequalities. Elevated AL is also correlated in some studies with work-related stress, poor quality jobs, burnout syndrome. Other research revealed racial disparities in AL with higher scores among young and middle-aged Black adults in comparison to Whites at all ages (Geronimus et al. 2006). Place or neighborhood characteristics have also been explored, showing the impact of social deprivation (Prior et al. 2018), environmental exposures, or neighborhoods perception by their inhabitants (van Deurzen et al. 2016).
Exploring these various correlations, researchers voice expectations for the potential outcomes of AL studies. Here we schematically classified the main claims based on the growing number of potential constraints and problems they may bring about. Indeed, while AL offers identifiable opportunities at the biomedical level, complex issues regarding methodological and conceptual robustness arise when moving towards the social dimensions of health and disease.
-
(1)
Improved disease prediction Early studies have shown AL to be a better predictor of mortality than metabolic syndrome components or individual mediators (Seeman et al. 2001). The use of AL as a composite multisystem score could improve the prediction of disease risk in certain contexts, through the identification of subclinical states which are less well detected by using single biomarkers. This results in the “expectation that AL can provide early warning signs for future adverse health outcomes” (Beckie, 2012, p. 341).
-
(2)
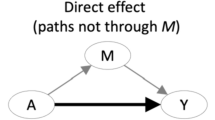
Identifying biological mechanisms of embodiment It is claimed that the use of AL can pave the way for the identification of physiological mechanisms governing the “biological embedding of social conditions” (Delpierre et al. 2016, p. 79) over the life-course, or that it could be a mediating link which may allow to unpack the black box of previous studies reporting social and spatial inequalities in health outcomes (Prior et al. 2018). Indeed, technical advances in the detection of biomarkers provide interesting leads to deepen the study of biosocial mechanisms, and may prompt new collaborations between biologists, epidemiologists, and social scientists (Harris and Schorpp 2018).
-
(3)
Addressing health inequalities It is often claimed that AL studies could help understand and act upon health inequalities. Indeed, as “lower SES environments expose individuals to more stressors while simultaneously providing them with fewer resources to deal with these stressors” (Adler and Stewart 2010, p. 14), AL is seen as a promising tool to design better specific public health interventions. For example, AL should “provide a mechanistic link to understanding health disparities” (Szanton et al. 2005, p. 7). These claims are not uniformly worded: some authors cautiously draw potential perspectives, while others embrace promissory futures that might seem still quite distant. We return to these claims in ‘The narrow path of AL research to meet its social promises’ section, where we address the epistemological and methodological issues currently limiting AL studies, to highlight the decoupling between some of these expectations, and the range of problems which remain to be solved to tentatively reach them.
Solving health inequalities, or biomedicalisation remade?
AL research has to deal with a central ambiguity: the new scientific tools and perspectives offered may help to address important issues in social epidemiology, however, like the other face of a coin, they also clearly fit in the dominant trend of biomedicalisation (Clarke et al. 2010), which could undermine its ambitions for public health. We underline some of the classic criticisms which can be addressed et al. research.
The post-genomic turn, showcasing a renewed focus on the deep porosity between organisms and environments (a notion which dates back to a much longer history, see below), has often been welcomed by social scientists as a new paradigm to finally get rid of the burden of biologisation brought about by the dominance of genetics. However, researchers have pointed out that in some scientific fields the old wine of genetic determinism could still readily be found in the bottles of the new biology (Richardson and Stevens 2015; Richardson 2017; Bliss 2018). By molecularising the biography of individuals (Niewöhner 2011), more precisely by revealing the biological pathways through which social inequalities ‘get under the skin’, the new biology is suspected of maintaining the biologisation of social inequalities, generating a set of interconnected risks: increased dominance of biomedical forms of evidence-making, abandonment of social explanations of socio-economic issues in favor of biological ones, and a focus on individual behaviour rather than on broader structural causes.
Mobilising biomarkers as direct and objective signifiers of mechanisms at work in causal pathways, from exposures to the development of disease, AL studies can easily align with the dominant legitimacy of biomedical sciences. But through this incorporation of biomedical tools in social epidemiology, AL research may well carry some of the risks associated with the biologisation of social phenomena. This has several interconnected consequences.
-
(a)
Epidemiologists get absorbed in ever-growing demands for biological proofs, as biomedical standards of evidence are seen as the main criteria to devise specific, targeted, and cost-effective public health actions in a context of limited funding. This trend can also be found in other fields, such as toxicology and environmental sciences, where an ever-increasing breadth of biological proofs is deemed necessary to take (or delay taking) action (Shostak 2013), and in particular in the emergent field of exposomic research.Footnote 4 Notwithstanding biomarkers’ intrinsic scientific usefulness, they can in this context be used as tools of persuasion for social epidemiologists, allowing them to speak the biomedical language often valued as more innovative, sound and relevant in medical and policymaking circles and funding agencies. Insisting on empirically identifiable biological traces, perceived as objective clues of the existence of direct mechanistic translations of social conditions into individual bodies, might be a strategic way to help convince a larger audience of the concrete physiological impact of social determinants of health, and promote the importance of this research. However, this kind of biomedical legitimisation comes at a cost.
-
(b)
The uptake of biomedical standards of evidence may overshadow intrinsic methods of proof-making in social science (see e.g. Schrecker 2013). The systematic use of biomedical tools and evidence orientates scientific research towards the production of a certain type of potentially useful knowledge, while other types may be ignored or bypassed, as research on agnotology and undone science has amply shown (Proctor and Schiebinger 2008; Frickel et al. 2010; Henry et al. 2021). Thus, approaches seeking to integrate biological factors into the study of social phenomena should assess how to do so without undermining social research’s own methods (in the context of the exposome research, Senier et al. 2017; Kelly-Irving et al. 2022).
-
(c)
As a consequence of (a) and (b), a stronger focus on biological features may run the risk of depoliticising socio-economic health issues. Surely, the scientific endeavor aimed at understanding how social processes biologically translate into health outcomes can hardly be criticised in itself. However, it generates a permanent impulse to devise a growing variety of biological measurements, entailing a risk that social epidemiology could become focused towards the appealing but elusive search for definitive biological mechanisms of embodiment, rather than on the social conditions governing individual and population health at a more structural level.
-
(d)
Finally, AL research could reinforce the search for biomedical solutions to social problems, to merely act upon biological and individual parameters in order to manage the social origins of illness. For example, Catherine Bliss argued that “social justice will increasingly be rendered a biomedical problem, displacing social scientific research as the main branch of disparities research” (Bliss 2015, p. 188), in her case focusing on the incursion of postgenomic sciences into health inequalities research. The same kind of problem could appear in studies seeking to link AL scores with measurements of social conditions. The extended uses of biomarkers may lead to a public health vision focused on individual risk factors, followed by a prioritisation of curative solutions often associated with medical and pharmaceutical intervention. AL research results do seem to offer an improvement in precision and in the capacity to predict future disease, which could lead to more efficient targeting of specific at-risk individuals for treatment or preventive action. However, the focus on an individual score functioning as a meta-biomarker influences the delineation of the normal and the pathological. The identification of subclinical states, determined by cut-off score values (see ‘The narrow path of AL research to meet its social promises’ section), could lead to well-known problems such as generating debated pre-disease categories and then overdiagnosis and potential overtreatment. It could orientate public health policies toward a focus on the health behaviours of at-risk individuals rather than addressing the structural causes of health inequalities, which since decades, social epidemiologists have been advocating for (Marmot 2004). The overarching search for biomedical solutions could keep delaying the use of the full extent of social and epidemiological knowledge already available for transformative public health action.
In sum, some features of AL research may well lead to an individualised, biologised and thus depoliticised vision of health disparities. However, it does not follow that AL studies should only be perceived as mere new items in the already quite full basket of biomedicalisation. In the next sections, we attempt to move beyond this necessary but limited criticism. Indeed, AL also stems from a lesser-known conceptual genealogy in which the social and the biological were differently combined in attempts to understand and address health inequalities. Through this genealogy, we seek to nuance the idea that the molecularisation and biologisation of stress is a by-product of recent orientations of biological research. On the contrary, AL is the product of a long history of research which displayed a biologisation of health inequalities, which made possible the materialisation of causal links between social conditions and diseases. In other words, in view of the history of the field, biologisation is not necessarily a risk of depoliticisation, but also a condition that has enabled social inequalities to become a medical and public health problem in its own right. This does not mean that biologisation cannot be problematic, and notably raises epistemological issues. Thus, we aim to demonstrate that AL is ambivalent and situated on a ridge line: on one side prone to biomedicalisation, but on the other reflecting past and different biosocial entanglements which had currency in social epidemiology.
A genealogy of allostatic load: recovering past biosocial entanglements
From homeostasis to allostatic load: roots of the AL concept in a physiological model of stress and a socio-epidemiological perspective
Even if some do not hesitate to trace the history of research on the environmental and social determinants of health back to Hippocrates, the modern biologisation of social inequalities in health is much more recent and dates back to the first part of the twentieth century. What characterises modern research in this field is the work of the great figures of nineteenth century social medicine or public health activism—Edwin Chadwick, Louis René Villermé, Rudolf Virchow, Friedrich Engels—who laid the foundations for a statistical approach (Waitzkin 1981; Krieger 2011). Then, biological models emerged to give a mechanistic explanation to biostatistics descriptions on social inequalities in health. The notion of stress has been central in addressing the physiological pathways through which social determinants and unhealthy environments affect morbidity and mortality risks and ‘get under the skin’. In his analysis of environmental epigenetics, Jörg Niewöhner mentioned AL as a “molecularised concept of chronic stress” and a “neuropsychoendocrinological re-writing” of “the cumulative impact of all chronic stressors on a given organism” (Niewöhner 2011, p. 281). He also briefly linked the history of chronic stress back to the Harvard physiologist Walter B. Cannon. Indeed, McEwen and Stellar built the AL concept on the previous coinage of the allostasis concept, by American neuroscientist Peter Sterling and epidemiologist Joseph Eyer (Sterling and Eyer 2005[1988]). Allostasis was itself introduced to go beyond the concept of homeostasis, famously built by Cannon in the 1920s as a mechanistic model explaining how health is impacted by social stress. It is precisely this genealogy of the AL concept that we wish to deepen. It requires tracing a complex series of conceptual and experimental developments which lead, from homeostasis to the allostatic load, to apprehend social inequalities in health not only through statistical measures, but, also, through a pathophysiological model based on psychosocial stress.Footnote 5
Cannon is mostly known for having studied the regulation mechanisms maintaining the stability of the organism, which he termed homeostasis (Cannon 1926). Firstly, in “Stresses and Strains of Homeostasis,” he proposed one of the first integrated theory explaining how specific physical or social stresses (Cannon 1935, p. 14) unbalance the body’s regulatory mechanisms, up to the “point at which the stability is ‘significantly altered’” (Cannon 1935, p. 7), making the body vulnerable to a whole gamut of diseases and disorders. Three main features emerge from this paper, in which we can identify future important directions:
-
(1)
the “vitality” of an individual could be measured by establishing a “homeostatic index,”
-
(2)
it should be possible to study when stress significantly alters physiological stability and precipitates the organism into pathology,
-
(3)
the study of the causes of stress (prolonged labour, fatigue, demands of school, infection, insomnia, etc.) should be done with attention to critical periods: childhood, adolescence, old age.
Cannon identifies key periods of development likely to have an impact on vitality. It is precisely this perspective that will be developed later in life-course epidemiology, defined “as the study of long term effects on later health or disease risk of physical or social exposures during gestation, childhood, adolescence, young adulthood and later adult life” (Kuh et al. 2003, p. 778). It is also in a life-course perspective that research in social epidemiology and exposome research using AL are developed (Vineis et al. 2020).
Secondly, Cannon attributes the shift from infectious diseases to a new range of ailments (heart and blood vessels pathologies, angina pectoris or exophthalmic goiter) to the socio-economic context and the successive crises that marked industrial development since the First World War. He underlines that unemployment and poverty could strain individuals and deplored that “reliable statistics are hard to obtain” (Cannon 1936, p. 1454), in order to get epidemiological data to complement laboratory research and clinical observations of diseases caused by emotional/social determinants.
Cannon’s theory of physiological imbalance induced by environmental, psychological, and social conditions had a programmatic influence in the work of microbiologist René Dubos, at Rockefeller University. Microbial agents are present in environments and organisms where they persist without causing disease, until organisms come under “physiological stress” (Dubos 1965, p. 164; see also: Honigsbaum 2017) such as nutritional status, fatigue, overwork, etc. In turn, Dubos’ takeover of Cannon’s model of vulnerability to diseases determined by physiological stress influenced a new generation of scholars, among which was John Cassel (Arminjon 2020b).
In the 1960s, Cassel imported the Cannon/Dubos stress model into social epidemiology (Cassel 1976). This physician and epidemiologist began his career in South Africa, where he developed community medicine centres for the Zulu population. In 1953, he later became director of the Department of Epidemiology School of Public Health at the University of North Carolina and greatly contributed to the development of social epidemiology, playing a pivotal role in the intellectual journey which led from homeostasis to allostasis. For instance, a series of studies he initiated highlighted that the level of social disorganisation is correlated to the incidence of cardiovascular pathologies, especially in the Black American community (Neser et al. 1971).Footnote 6 Results are explained either by Whites benefiting from more psychosocial resources likely to compensate for the physiological effects of stress, or by the effects of social disorganisation having a tenfold effect on the members at the lowest position in the social hierarchy.
The introduction of the allostatic model can be seen as a theoretical extrapolation of this line of work that has helped to demonstrate how psychosocial stress impacts and modulates physiological life. In 1988, Sterling and Eyer developed allostasis to complement and overcome what they saw as homeostasis’ “fixism,” its inability to account for adaptation to stress. The transition from homeostasis to allostasis can be read as a transition from a theory of stress as a potential source of bodily dysfunction, to a theory of physiological adaptation to stress. While homeostasis posits that stability is maintained by keeping physiological parameters fixed, i.e. “through constancy”, allostasis contends that physiological stability is reached “through change” (Sterling and Eyer 2005[1988], p. 636). Allostasis “exemplifies a critical principle of physiology: to maintain stability an organism must vary all the parameters of its internal milieu and match them appropriately to environmental demands” (Sterling and Eyer 2005[1988], p. 636). The two concepts are nevertheless tightly linked, most notably regarding the study of psychosocial stress as a determinant of disease.
The allostatic model came at the climax of Eyer’s 1970s research in social epidemiology. Eyer alone, then with Sterling, published several papers which attest to the rooting of the allostatic model in the study of psychosocial determinants of chronic diseases, with a special emphasis on hypertension (Eyer 1975, 1977; Eyer and Sterling 1977). They endorse a critical perspective influenced by Marxism (historical materialism), seeking to demonstrate how both normal and pathological physiologies are shaped by social organisations (Arminjon 2016). For example, Eyer showed that mortality rate does not reach its maximum in times of economic depression, but that mortality due to heart disease, stroke, cancer, cirrhosis, diabetes, accidents, influenza-pneumonia, ulcers, actually increase during economic booms, while suicides and homicides decrease. These correlations are interpreted to support the thesis that diseases are associated with the stress induced by increased working hours, migration and community disorganisation (Eyer 1977). These results were integrated in the 1988 definition of allostasis.
Sterling and Eyer built on programmatic ideas that Cannon only imagined at the end of his career. While homeostasis designates the regulatory mechanisms allowing the body to maintain stable physiological parameters in daily situations, the allostatic model differs most clearly by trying to demonstrate, from an epidemiological populational perspective, the variability of physiological parameters resulting from the adaptation to socio-cultural environments. The foundational objective of the model aimed at drawing all the implications of chronic and cumulative stress, through a critical and comparative examination of how stress factors were linked to specific socio-cultural determinants, particularly those of capitalist societies. For instance, for Sterling and Eyer (1977, p. 5), cross-cultural epidemiology indicated that hypertension in the general population was a psychosocial adaptation to industrialised societies, and that social and racial discrimination amplified this trend in the African-American community (Arminjon 2020b).Footnote 7
We can now highlight an epistemological shift between the allostatic model and the allostatic load/overload model. When McEwen and Stellar introduced the AL concept (‘Allostatic load as an operational measure of stress’ section), they did stay in line with Sterling and Eyer by defining AL as “the cost of chronic exposure to fluctuating or heightened neural or neuroendocrine response resulting from repeated or chronic environmental challenge that an individual reacts to as being particularly stressful” (McEwen and Stellar 1993, p. 2093). But later on, they departed from Sterling and Eyer. As said above, for the latter, a condition like hypertension is not a dysfunction, but an adaptation. If every condition is an adaptation, it becomes difficult for the allostatic model to determine whether, and under what conditions, a long-term adaptation to the environment can be stated as dysfunctional or pathological. McEwen and Wingfield (2003), thus distinguish how brief or sustained AL can lead to two types of allostatic overload: “Type 1 allostatic overload occurs when energy demand exceeds supply, resulting in activation of the emergency life history stage” and “Type 2 allostatic overload begins when there is sufficient or even excess energy consumption accompanied by social conflict and other types of social dysfunction” (McEwen and Wingfield 2003, p. 2). Type 1 allostatic overload overlaps with the kind of situation occurring in a “natural environment” (lack of food, hibernation, migration etc.) requiring the organism to get into survival mode. Type 2 rather refers to the consequences of stress caused by modern life: the neurophysiological processes activated during chronic stress (HPA axis, autonomic nervous system), and the coping behaviours (over-consumption of alcohol, tobacco, junk food) which in sedentary life may lead to pre-diabetic state, atherosclerotic plaque, left ventricular hypertrophy, etc. While the allostatic model leads to defining adaptation as a neutral process in the distinction between the normal and the pathological, the allostatic load/overload model thus designates a theoretical approach making it possible to think of adaptation as pathological when it designates an increased risk of disease that could, in principle, be measured.
Through the definition of AL as the cumulative strain on the body produced by chronic stress, McEwen and collaborators (Seeman et al. 1997; Seeman et al. 2001) actually revived Cannon’s idea to create a “vitality index”: the opportunity to create an “allostatic load index”, defined as “a cumulative index of risk for disease” (Seeman et al. 1997, p. 2266). Using longitudinal data—the cohort of the MacArthur studies of successful ageing from 1988 to 1991—they developed a measure of AL based on ten physiologic parameters tied to different regulatory systems. Results revealed that higher AL scores predicted poorer cognitive and physical functioning, higher reduction in cognitive and physical functioning, and increased risk of cardiovascular disease. However, in the limitations of the study, the authors mention that the AL index they used may not include all relevant aspects of physiologic functioning. McEwen and Wingfield later concluded that “an independent measure of allostatic load (…) is key, and only then will the concept be tested objectively” (McEwen and Wingfield 2003, p. 11). In other words, the question of which parameters should be included in the AL index does not seem unreachable but is still not resolved. Today, a significant amount of research in the field is aimed at varying parameters to improve existing AL scores. We will see in ‘Methodological issues related to the operationalisation of AL in social epidemiology’ section. that the creation of such indexes still raises several important epistemological and methodological challenges.
Bio-social entanglement in the history of AL
At first sight, the AL model could be interpreted as a return to a physiological model of stress, without taking into account the socio-epidemiological roots of the allostasis concept. As pointed out above, this apparent shift in investigation from social to biological pathways might contribute to the depoliticisation and individualisation of public health problems, and seems consistent with the idea that an excessive focus on biological rather than socio-epidemiological evidence is bound to contribute to a biomedicalisation of health inequalities. However, this genealogy leads us to qualify such a conclusion, from both political and epistemic standpoints.
At first, the genealogy of AL could be interpreted as an oscillation between the biological side (Cannon and homeostasis) and the social side (Cassel and Eyer) of a same coin that is intrinsically the biosocial framework. When the orientation veers towards the social end, hypotheses are tested to determine what kind of social factors or organisation is more or less likely to induce stress and consequently diseases. When the focus is rather on biological characteristics, hypotheses are tested to determine which physiological pathways are involved in psychosocial stress. Indeed, Cannon’s approach could be read as pertaining to a biosocial framework. The homeostatic model, one of the first physiological models of stress, was intended to understand the physiological pathways of the social determination of health. On an epistemological standpoint, Cannon was explicitly aware that his research could not be conceived solely from a biological point of view. He clearly pointed out that socio-epidemiological data would, if readily available, contribute to more accurate causal determinations. In other words, Cannon precisely pointed at the risks of reducing the social to the biological, and programmatically called for a multi-level and interdisciplinary approach to the social determinants of health. On a political standpoint, Cannon never hid that his scientific program was related to political activism, as he promoted social protection and economic interventionism inspired from the social ‘experience’ the USSR was developing at the time (Cannon 1939, 1945). Thus, Cannon definitely advocated for a biologisation of the study of social determinants of health, but in a form that one cannot suspect of reinforcing any individualistic conception of health. The same can be said about researchers such as Cassel, personally affected by issues of racial health inequalities, as well as Sterling and Eyer who claimed their radical orientations. Their involvement in the ‘science for the people’ movement, in the struggle for civil rights, and their concern for health inequalities affecting the African American communities, show that approaches linking the biological and the social may lead to other paths than conservative sociobiology or neoliberal biomedicalisation.
Secondly, it should be emphasised that the allostatic model (and its adaptationist conceptual framework) relies on the homeostasis model (and its functionalist physiological framework). The homeostatic model was intended to provide an experimental basis for clinical observations (Cannon 1916, 1935, 2020), since Cannon spent most of his career studying the role of stress and its physiological pathways in the development of diseases. Then, the allostatic model is also a physiological model, conceived as a general theory of adaptation to stress, but Eyer and Sterling did not develop it from laboratory experiments. In their model, the physiology of stress is taken for granted, and mobilised as a causal explanation for statistical correlations, which were discovered following hypotheses drawn not from clinical, but epidemiological and sociological rationales.
Thirdly, the AL model is part of a psychosocial trend which uses biological means to overcome the limits and social reductionism of the materialist trend in social epidemiology. This psychosocial trend of social epidemiology could be understood as a way to expand the study of structural determinants of health. As pointed out by Cassel, the theory of the host’s susceptibility makes a distinction between exposure to physicochemical pathogens and exposure to psychosocial factors. The former have a direct adverse effect on organ structure and function, whereas the latter exert an indirect pathogenic action by disturbing the homeostatic balance (Cassel 1974). The issues involved in distinguishing between direct and indirect effects can be illustrated with the debates opposing advocates of the psychosocial model like Michael Marmot (Marmot and Wilkinson 2001) to the supporters of materialist approaches, either the one adopted by the authors of the Black Report (Black 1980) in the United Kingdom or defended by neo-materialists (Lynch 2000). Materialist approaches assume that social inequalities in health mainly affect people living below the poverty threshold, so that an increase in living standards, education, hygiene, etc., would eventually eradicate inequalities. However, for the proponents of the psychosocial approach, this explanation is contradicted by the social gradient, i.e. that health inequalities can be measured all along the social hierarchy (Marmot 2004). To psychosocial epidemiologist, material conditions fail to explain health inequalities above a certain standard of living, and at this level the health status is rather determined by the perception of one's social position and the stress factors associated with status (control over one’s life, number of friends, social support, quality of hobbies, etc.). Most importantly, to psychosocial epidemiologists, only neuroendocrine pathways can account for how psychosocial factors make hosts more susceptible to disease through stress. Thus, in the psychosocial model, biologisation does not represent an individualisation and a depoliticisation of health problems. On the contrary, it is the condition for extending the study of the structural determinants of health beyond sole material determinants.
To conclude, the apparent return to a physiological model operated by AL researchers must be situated in a broader context. The project of uncovering biological mechanisms is not new and does not necessarily compete with, but may complement documenting social determinants at the epidemiological level. In other words, the biological and social sides of social epidemiology are historically, politically, and epistemologically inseparable as two sides of a same coin, and both may contribute to shape a collective (i.e., not individualistic) representation of health.
This historical section thus shows that there is no systematic or intrinsic risk of reductionism or depoliticisation to be associated with the biologisation of social inequalities in health: since its inception, social epidemiology actually integrated a biosocial approach associated with some explicit political agendas. From the diverse approaches at their origin, recent developments on the biological embodiment of health inequalities based on the AL concept inherited a tension, or ambivalence, in the orientation of research that can lean towards a more biological or a more social side. The way this tension takes place in the context of AL-based research has been nicely put into light by Gustaffson (2016) and can also be interpreted as diverging thought styles on embodiment, between “biological embedding” on one side and the “embodiment of social experiences” on the other (Louvel and Soulier 2022). In the last section, we analyse a series of epistemological and methodological issues raised by the specific biosocial approach conveyed by the AL concept.
The narrow path of AL research to meet its social promises
The constitutive conceptual ambivalence of AL leads to question its potential uses and the extent to which the claims and promises put forward in this research field could be realised. In ‘Allostatic load and the “biosocial turn” in social epidemiology’ section, we mentioned three main categories of promises made in AL studies: (1) improved disease prediction, (2) identification of biological mechanisms of embodiment, (3) addressing and explaining health inequalities. In this section we return to these promises in light of the genealogical background developed above. We will see that the conceptual ambivalence of the AL concept is echoed by a practical heterogeneity in the operational construction of AL scores. This heterogeneity is problematic for the three categories of promises. We highlight a tension between the promise of better prediction and that of better explanation. The variable and unstable relationship between AL and social conditions over time and place limits the representativeness and comparability of results.Footnote 8
Methodological issues related to the operationalisation of AL in social epidemiology
The core difficulties in AL research arise from its operationalisation as a meta-biomarker, while trying to obtain “an independent measure of allostatic load” which is seen as “key”, since “only then will the concept be tested objectively” (McEwen and Wingfield 2003, p. 11). As we have seen, this amounts to finding a practical way to reach Cannon’s earlier goal to develop a “vitality index.”
Despite the extension of AL research, there is still no consensus on a general method to construct this index. This raises issues of reproducibility and comparability, which have been identified and debated in the AL field. Reviewers have noted that “researchers have not taken a consistent approach to the way they have operationalised the concept” (Johnson et al. 2017, p. 67) and that “the central issue […] was the enormous heterogeneity in the biomarkers, cut-off values, control for medication intake, and mode of calculation used for the assessment of AL. Such heterogeneity makes it difficult to compare the studies and draw overall conclusions” (Ribeiro et al. 2018, p. 10). Indeed, a growing number of variables are used in different combinations. Since the original study which used a set of ten markers (Seeman et al. 1997), other markers have been tried, their choice being often dictated by the availability of samples in a specific cohort. Early on, reviewers already criticised variations in the “strength of justification for inclusion of variables beyond the original ten” (Szanton et al. 2005, p. 11).
Once a specific set of markers has been determined, the next methodological choice in order to construct an AL index lies in establishing cut-off values for each marker, which determines high- or low-risk ranges. A score is then attributed to the measurement in the sample, depending on the risk zone in which it is situated. The AL score consists in the addition of scores obtained for all chosen biomarkers. The choice of cut-offs values also varies between studies (for example: higher quartile, or higher 10%, to determine the high-risk zone for a specific biomarker). Ensuing debates on the appropriate cut-offs to be chosen for each parameter are linked to the idea that AL should allow to detect pre-diseased states in individuals with cumulative risks, despite the absence of any symptoms. Thus, if the cut-offs are too large, they will be imprecise and lead to classify as high-risk people who will not develop any disease, but if they are too narrow, they will only allow the identification of very-high-risk individuals.
The issue of comparability is even greater for AL studies seeking to correlate AL scores with measures of social conditions which are also very diverse, in terms of dimensions (occupation, education, income, SES, gender, race, social deprivation, etc.) or levels (individual or population). This may lead to confounding effects. For example, the use of general social indicators such as income and education could be problematic for AL studies because it “obscure[s] the specific dimensions of SES that are most related to stress and the health impacts of stress” (Dowd et al. 2009, p. 1306). Moreover, the relationship between AL and social conditions is mediated through multiple indirect pathways of health-related behaviours, physical factors (pollution, degradation, etc.) and social stressors (unsafety, discrimination, lack of support, etc.). The heterogeneity of these social variables, and their multiple possible interactions with AL, adds up to the intrinsic heterogeneity of AL scores. In the end, these issues of reproducibility and comparability could “[hinder] a better understanding of the biological mechanisms underlying poorer health amongst those of a lower [SES]” (Johnson et al. 2017, pp. 70–71), which is nevertheless one of the main initial goal of AL research as visible in the second category of promises identified above.
A second set of issues in some AL studies lies in the loosening of the conceptual tie with the notion of stress when translating the AL concept into an operational index. We saw that the concept is historically rooted in the psychosocial model in which the physiology of stress is central. Nevertheless, reviewers pointed out that “HPA axis biomarkers were absent from nearly half of studies, which contradicts McEwen and Stellar’s initial conceptual framework emphasising the importance of HPA axis biomarkers as primary mediators,” and strongly stated that “the substantial inconsistency in biomarkers used to operationalise AL and the lack of fidelity to its original conception, as an index that captures the biological response to psychosocial stress is striking. This suggests that the empirical literature on AL is intrinsically flawed and without a strong conceptual basis” (Johnson et al. 2017, p. 70).
Indeed, the decoupling from stress seems to break away from the historical and conceptual roots of AL, and its overall purpose. Original AL studies grounded its capacity to improve the prediction of disease, compared to other multi-biomarker indexes, in considering the multi-system impacts of stressors. When removing stress-associated markers, the main difference between AL and other composite scores is largely lost. The malleability of this foundational link between concept and tool questions the capacity of studies moving away from stress to significantly articulate the biological and the social, especially if stress, in the psychosocial model, is the condition for extending the structural determinants having a negative impact on health.
A third important problem lies in the difficult trade-offs and explanative costs associated with a composite measure. A synthetic score is useful as a predictive tool but entails a loss of information and precision regarding the causal contribution of each specific marker. The construction of combined index scores with several parameters has been tried with cardiovascular disease or metabolic syndrome for example. Seminal AL studies have shown an improvement of “the prediction of mortality and declining physical functioning compared to the MetS [metabolic syndrome] and the primary mediators alone” (Beckie 2012, p. 313). In theory, as a combination of multi-system markers, the advantage of AL as a synthetic biomarker of stress is to offer the possibility to largely embrace the diverse effects of stressors on different physiological systems. However, “combining different physiological systems into a single empirical index rather than taking a system-specific approach involves important trade-offs” (Dowd et al. 2009, p. 1305), which are heavily debated, as it “inevitably leads to a loss of biological specificity” (Harris and Schorpp 2018, pp. 11–12). In a combined score, information is lost in understanding the specific contribution from each biomarker to overall risk (Beckie 2012, p. 341). This issue has led to the rather paradoxical option of going back to the specific markers: “summing scores on a diverse panel of biomarkers may obscure significant heterogeneity in dysregulation across individuals, physiological systems, and types of stressors. (…) a recent trend toward disentangling the components of allostatic load to explore their unique associations with health outcomes of interest (…) reflect the conceptual tension between cumulative vs. system-specific attempts to quantify the impact of social contexts on physiological function and health” (McDade 2008, p. 521).
These issues in the practical application of AL concept into a workable tool show that the ideal of improving knowledge of the mechanisms governing the physiological impacts of stress, as already advocated a long time ago by Cannon, is hard to reach. While it may be reasonably stated that using AL gives added visibility to the concrete biological impact of social determinants, the details of biological mechanisms may still remain quite obscure. The uncertainty in reaching these elusive mechanisms should invite us to proceed with caution in thinking about potential gains when including biological tools into the study of social life and when seeking precise biological pathways (see Link and Phelan 1995).
Moreover, a tension occurs here between the two promises of (1) improving prediction, and (2) better identifying the biological mechanisms of embodiment. The gains brought by such a synthetic meta-marker in the prediction of disease risk could finally be a loss in precise mechanistic explanation. This situates issues about AL research in the straight continuity of the epistemological and methodological issues raised by biomarkers (see e.g. Pearce et al. 1995; Strimbu and Tavel 2010; Tabb and Lemoine 2021), and the exact conceptual status of AL is often hard to sort out: are AL scores and biomarkers that compose them thought of as proxies in the prediction of disease risks? Or are they understood as providing a causal mechanism explaining the pathways between the social and the biological in the production of disease?
The variable and unstable relationship between AL and social conditions
There are several additional issues that arise when AL is implemented into the study of health inequalities, though it is an explicit objective of most of AL studies as stated in the third category of promises we identified above. It could seem like a logical step to consider assessing social conditions using AL. In the same manner that social deprivation indexes have been built in the 1980s by using social data at the population level as a proxy (Townsend 1987; Carstairs and Morris 1989), AL could be considered as a new way to overcome the lack of social data at the individual level and as a potential gold standard proxy to assess individual social deprivation through biomarkers, and to bring more precision to the study of the mechanistic pathway of health inequalities. However, the relationship between AL and social factors is largely variable, and difficult to standardise between studies.
Indeed, studies presenting AL as a mediator linking social conditions and health outcomes may convey the belief that this link is universal. However, it appears that the two-way causal chain (social conditions-AL and AL-health outcomes) is not univocal. This relationship is dependent on cultural, geographical, and temporal contexts, which can be unveiled through comparisons at the population level or/and thanks to ethnographic studies (see e.g. Niewöhner and Lock 2018). For example, studies done in Taiwan showed no significant link between AL biomarkers and SES gradient in health, which could “plausibly suggest a different biological pathway linking SES and health in Taiwan than in Western countries” (Beckie 2012, p. 322). The various forms of social deprivation, and ways to measure it according to specific national or regional settings, limit the capacity to integrate heterogeneous social data in international studies. Thus, useful epidemiological comparisons across populations living in diverse social, cultural, and ecological settings “raise additional challenges for [AL]”, mostly because “it cannot be assumed that the relationship between various biomarkers and health outcomes (e.g., between [AL] and mortality risk) will be the same across populations” (McDade 2008, p. 522). For example, the physiological effects of social isolation will be different according to the importance of collective life in each culture. Moreover, the association between social deprivation measures and AL could be itself mediated by confounding factors such as “detrimental behaviours, stress and anxiety feelings caused by the neighbourhood conditions and […] the poor social and physical environments found in impoverished areas” (Ribeiro et al. 2018, p. 10). Another multilevel longitudinal study, in China, reports that “AL was lower among people with university-level compared with no education, but higher in counties with higher mean education years.” Authors conclude: “AL in China is patterned geographically. The degree of association between AL and person-level education seems to be dependent on area-level education” (Mao et al. 2019, p. 1).
Finally, the assessment of life-course cumulative exposures implies dealing with the temporal evolution of social conditions. For example, educational level has improved markedly since the mid-twentieth century in developed countries, and a high school diploma is no longer considered a high-level diploma as it once was. In a life-course perspective, the association between social conditions, AL and gradients in health outcomes should then be carefully assessed and adjusted over time.
The interest of AL in the study of health inequalities could be to compensate for the various meanings and availability of social variables in different contexts by biological measures supposed to be more accurate and universal. However, the variable and unstable relationship between AL and social conditions makes it illusory to think that AL score represents a reliable stand-alone marker to measure social conditions and deal with the complexity of social measure and their interaction with health outcomes. These results, revealing the complex link between social conditions and AL scores, stand in agreement with the medical anthropological proposition that universalisation cannot be realised in view of situated “local biologies” (Niewöhner and Lock 2018). Moreover, all these data claim for further dedicated research to improve the precise measurement of social conditions in health studies.
AL does not seem to reduce complexity in the study of health inequalities, which leads to asking how results could be operationalised into preventive interventions. While it is undoubtedly scientifically worthwhile to gain further insight on the mechanisms governing the biological embodiment of social life and the bodily imprinting of cumulative risks over the life-course, better public health action will not automatically follow. Indeed, another claim of usefulness of the AL model to address health inequalities is based on the idea that improving the identification of biological mechanisms will necessarily translate into better targeted public health interventions, both at the populational and individual level. Yet, the risk here is to conflate the cause of cases (individual-level causation) and the cause of cause or cause of incidence (Rose 1992). Following Geoffrey Rose, we argue that there is no necessary relationship between understanding biological mechanisms of social embodiment at the individual level, and understanding social mechanisms leading to health inequalities, through which biological and health outcomes are progressively differentiated at the population level. Moreover, we already have social categories (with their limitations) with numerous validated associations in terms of health inequalities, which offer many levers for public health policies. As pointed out above, studies linking AL scores and social data might lead to excessively focus on interventions at the individual level based on the detection of biomedical risk characteristics (“high-risk preventive strategy” in the vocabulary of Rose), while many more general and non-medical preventive actions (“population strategy”) are still waiting to be effectively deployed against health inequalities.
Moving beyond the focus on associating social conditions and AL scores at the individual level, and thus using AL to better understand the construction of health inequalities, would require mobilising biological measures in a more longitudinal and populational approach in order to assess the life-course differentiation of health outcomes at the population level. Longitudinal approaches are needed to identify how AL can be situated in and help understand the causal chain between social characteristics and health outcomes (Prior 2021). Researchers plead to repeatedly collect biological samples in available cohorts in order to “represent the dynamic nature of AL” (Delpierre et al. 2016). Linking this to the development of AL cohorts with exhaustive social data and increased follow-up would support this populational approach.
Conclusion
Our aim in this paper was to help identify the potential costs and risks associated with AL studies. We started by situating AL in the ‘biosocial turn’ in social epidemiology, its promises, and in relation to criticisms raised by social scientists against the biomedicalisation of social inequalities in health. AL runs into a similar set of risks and might reinforce the search for biomedical solutions to social problems. In adopting the biomedical standards of evidence, the limited human and economic resources dedicated to research might be absorbed in ever-growing demands for biological evidence, at the expense of proper methods of evidence-making in social science. The search for definitive biological causal mechanisms of embodiment might lead to lose sight of “fundamental causes” (Link and Phelan 1995), the social conditions governing individual and population health, and thus to bypass other ways of explaining social mechanisms and existing public health strategies dedicated to preventing the impact of social inequalities on health. This biomedicalisation of social inequalities in health can well be seen as the expression of a political neoliberal moment which finds advantage in individualising and depoliticising social problems (Lynch 2017).
In order to qualify and precise this kind of criticism, we took a detour through the historical development of social epidemiology and the genealogy of the AL model, to show that the biologisation of social inequalities in health extends historically well beyond recent scientific developments and the current political situation. The genealogy of the allostatic model must be inscribed in the history of social epidemiology, which gives a central role to how psychosocial factors impact the physiology of stress. From Cannon’s first works to the recent development of the AL score, social epidemiology articulated its approach to social inequalities in health from two sides of the same coin—socio-epidemiological and biological—which appear to be both complementary and intricate, and also non-reducible to each other. From a historical perspective, the biologisation of social inequalities in health is therefore not new, and is not realised, in epistemological terms, at the expense of socio-epidemiological research. Biology delivers plausible mechanistic explanations of statistically established epidemiological correlations, just as it makes it possible to justify why specific biomarkers—i.e., blood pressure, diabetes or various markers put together in the AL score—are indeed relevant for research on health inequalities. But most importantly, we have also seen that the distinction between exposure to pathogens, as in materialist approaches, and psychosocial factors that modulate host susceptibility, allows social epidemiologists to extend the range of the structural determinants of health beyond the material ones. To psychosocial epidemiologists, the physiology of stress leads to a better understanding of the factors that determine social inequalities in health all along the social gradient and even in rich industrialised countries. Therefore, in such a context, biologisation cannot be associated with an individualisation and a depoliticisation of health.
The history of the AL concept shows that thinking together and articulating the biological and the social was present since the origins of researching the relationships between health and social conditions, as mediated through stress. This allows us to understand that the tension and risks associated with AL come less from its potential for reductionism, in the sense of reducing the social to the biological, than from overly focusing on one direction of their relationship in the chain which links social conditions and health outcomes. Easing this tension lies in finding equilibrium between these directions. Historicising the uses of biology in social epidemiology shows that biological tools and concepts could be used to help social epidemiology answer the structural question of how the social organisation itself distributes disease and health inequalities. In this sense, social epidemiology should use biological tools with a focus on what they can bring to possible interventions. From there, uses of the biological in social epidemiology may be seen not necessarily as a Trojan horse of biomedicalisation, but also as possibly opening ways to support ambitious radical propositions for progressive public health action.
Nevertheless, we emphasise several limitations in the operationalisation of AL in biosocial studies that question its capacity to effectively meet its social promises. First, the complexity and the heterogeneity of both measures of AL and social conditions hinder the comparability of results of biosocial studies using AL, which prevents from extending conclusions that can be drawn from them. Second, the translation of the AL concept into an operational index ends in loosening its conceptual tie with the notion of stress. Moreover, the literature reports a variable and unstable relationship between AL and social conditions according to cultural, geographical, and temporal contexts, which runs contrary to the view of AL as a potential standard marker of social conditions and stresses the importance of “situating biologies”. Finally, the use of AL in biosocial studies reinforces the perceived imbalance in the availability and accuracy of data to trace biological mechanisms on the one hand and social mechanisms on the other. While AL studies hope to advance the understanding of health inequalities through the intensive use of biomedical data, to achieve this aim they will still require the difficult extensive collection of precise social information over the life-course, which is a classic issue in social epidemiology.
Data availability
No datasets were generated or analysed during the current study.
Notes
Survey based on a PubMed search for “allostatic load” in the Title/Abstract section. In 2021 alone, 187 articles have been published, for a current total of 1431 (December 2022). Out of this large search, we extracted all the review articles to access the main issues debated in the research community which uses this tool. Additional empirical articles have been selected to address specific points regarding the studies that connect AL with socio-economic status.
Following Johnson et al. (2017, p. 67), we mention ‘AL index’ or ‘score’ when referring specifically to the quantifiable variable.
The aim of this emergent field of research is to develop an integrative and comprehensive approach of individual exposures influencing health over the life-course. But the main focus of the field is currently on the internal exposome (Giroux et al. 2021; Giroux, forthcoming 2023). The aim is to “deliver a correspondingly comprehensive analysis for the environment that fits into the biomedical framework” (Miller 2021).
These studies used the Harvey Smith index, which included the percentages of single-parent families, males sentenced to prison, separated couples, etc. Here, the methodological creation of a composite index was established using social parameters only, to identify which affected health the most.
For a detailed genealogy of the cross-cultural epidemiology of hypertension particularly in the African American community, see Arminjon (2016, 2020b) and Pollock (2012, Chaps. 3–4). See also Kuzawa and Sweet (2009) for a convincing review highlighting the developmental mechanisms of cardiovascular disease disparities, and thus the ‘embodiment of race’ as a social condition, against explanations leaning on genetics.
While AL studies share a common conceptual and methodological backbone, they should not be regarded as an entirely homogeneous field.
References
Adler, N.E., and J. Stewart. 2010. Health disparities across the lifespan: Meaning, methods, and mechanisms. Annals of the New York Academy of Sciences 1186 (1): 5–23.
Arminjon, M. 2016. Birth of the allostatic model: From Cannon’s biocracy to critical physiology. Journal of the History of Biology 49 (2): 397–423. https://doi.org/10.1007/s10739-015-9420-9.
Arminjon, M. 2020a. Homéostasie, stress et société : Walter Cannon aux fondements des déterminants sociaux de la santé. In Walter B. Cannon. Conférences sur les émotions et l’homéostasie, Paris, 1930, ed. M. Arminjon, 13–115. Lausanne: BHMS.
Arminjon, M. 2020b. The American roots of social epidemiology and its transnational circulation. Gesnerus 77: 35–43. https://doi.org/10.24894/Gesn-en.2020.77002.
Beckie, T.M. 2012. A systematic review of allostatic load, health, and health disparities. Biological Research for Nursing 14 (4, SI): 311–346. https://doi.org/10.1177/1099800412455688.
Black, S.D. 1980. Inequalities in health: The black report. London: Department of Health and Social Security (DHSS).
Bliss, C. 2015. Defining health justice in the postgenomic era. In Postgenomics: Perspectives on biology after the genome, ed. S.S. Richardson and H. Stevens, 174–191. Durham: Duke University Press.
Bliss, C. 2018. Social by nature: The promise and peril of sociogenomics. Stanford: Stanford University Press.
Brunner, E. 1997. Stress and the biology of inequality. BMJ 314 (7092): 1472–1476. https://doi.org/10.1136/bmj.314.7092.1472.
Cannon, W.B. 1916. Some disorders supposed to have an emotional origin. New York Medical Journal 104: 870–873.
Cannon, W.B. 1926. Physiological regulation of normal states: Some tentative postulates concerning biological homeostatics. In A Charles Richet: Ses amis, ses collègues, ses élèves, ed. A. Pettit, 91–93. Paris: Editions Médicales.
Cannon, W.B. 1935. Stresses and strains of homeostasis. Journal of the Medical Sciences 189 (1): 13–14.
Cannon, W.B. 1936. The role of emotion in disease. Annals of Internal Medicine 9 (11): 1453–1465.
Cannon, W.B. 1939. The wisdom of the body. New York: W.W. Norton, cop.
Cannon, W.B. 1945. The way of an investigator. A scientist’s experience in medical research. New York: W.W Norton.
Cannon, W.B. 2020. Walter B. Cannon, Paris, 1930. Conférences sur les émotions et l’homéostasie. Précédées d’une introduction critique, ed. M. Arminjon. Lausanne: BHMS.
Cantor, D., and E. Ramsden, eds. 2014. Stress, shock, and adaptation in the twentieth century. Rochester: University of Rochester Press.
Carstairs, V., and R. Morris. 1989. Deprivation: Explaining differences in mortality between Scotland and England and Wales. BMJ 299 (6704): 886–889.
Cassel, J. 1974. Psychosocial processes and “stress”: Theoretical formulation. International Journal of Health Services 4 (3): 471–482. https://doi.org/10.2190/WF7X-Y1L0-BFKH-9QU2.
Cassel, J. 1976. The contribution of the social environment to host resistance. American Journal of Epidemiology 104 (2): 107–123.
Clarke, A.E., et al. (eds.). 2010. Biomedicalization: Technoscience, Health, and Illness in the U.S. Durham, NC: Duke University Press.
Delpierre, C., et al. 2016. Origins of heath inequalities: The case for Allostatic Load. Longitudinal and Life Course Studies 7 (1): 79–103. https://doi.org/10.14301/llcs.v7i1.325.
Dowd, J.B., A.M. Simanek, and A.E. Aiello. 2009. Socio-economic status, cortisol and allostatic load: A review of the literature. International Journal of Epidemiology 38 (5): 1297–1309. https://doi.org/10.1093/ije/dyp277.
Dubos, R. 1965. Man adapting. New Haven: Yale University Press.
Eyer, J. 1975. Hypertension as a disease of modern society. International Journal of Health Service 5 (4): 539–558. https://doi.org/10.2190/UT72-3RTX-V0KN-64AF.
Eyer, J. 1977. Prosperity as a cause of death. International Journal of Health Services 7 (1): 125–150. https://doi.org/10.2190/9WA2-RVL3-MT9D-EL9D.
Eyer, J., and P. Sterling. 1977. Stress-related mortality and social organization. The Review of Radical Political Economics 9 (1): 1–44.
Frickel, S., et al. 2010. Undone science: Charting social movement and civil society challenges to research agenda setting. Science, Technology, & Human Values 35 (4): 444–473.
Geronimus, A., et al. 2006. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. American Journal of Public Health 96 (5): 826–833. https://doi.org/10.2105/AJPH.2004.060749.
Giroux, E. In press 2023. A critical assessment of exposures integration in exposome research. In Integrative approaches in environmental health and exposome research: Epistemological and practical issues, eds. E. Giroux, Y. Fayet, and F. Merlin. Springer-Palgrave.
Giroux, E., Y. Fayet, and T. Serviant-Fine. 2021. L’exposome, tensions entre holisme et réductionnisme. Medical Sciences (Paris) 37 (8–9): 774–778. https://doi.org/10.1051/medsci/2021092.
Guidi, J., et al. 2021. Allostatic load and its impact on health: A systematic review. Psychotherapy and Psychosomatics 90 (1): 11–27. https://doi.org/10.1159/000510696.
Gustaffson, P.E. 2016. Commentary. In Delpierre C. et al. Origins of health inequalities: The case for allostatic load. Longitudinal and Life Course Studies 7 (1): 79–103 https://doi.org/10.14301/llcs.v7i1.325.
Harris, K.M., and K.M. Schorpp. 2018. Integrating biomarkers in social stratification and health research. Annual Review of Sociology 44: 361–386. https://doi.org/10.1146/annurev-soc-060116-053339.
Henry, E., et al. 2021. Introduction: Beyond the production of ignorance: The pervasiveness of industry influence through the tools of chemical regulation. Science, Technology, & Human Values 46 (5): 911–924. https://doi.org/10.1177/01622439211026749.
Honigsbaum, M. 2017. René Dubos, tuberculosis, and the “ecological facets of virulence.” History and Philosophy of the Life Sciences 39 (3): 15. https://doi.org/10.1007/s40656-017-0142-5.
Jackson, M. 2013. The age of stress: Science and the search for stability. Oxford: Oxford University Press.
Jackson, M., ed. 2015. Stress in post-war Britain, 1945–85. London: Pickering & Chatto.
Johnson, S.C., F.L. Cavallaro, and D.A. Leon. 2017. A systematic review of allostatic load in relation to socioeconomic position: Poor fidelity and major inconsistencies in biomarkers employed. Social Science & Medicine 192: 66–73. https://doi.org/10.1016/j.socscimed.2017.09.025.
Kelly-Irving, M. 2022. Falling down the rabbit hole? Methodological, conceptual and policy issues in current health inequalities research. Critical Public Health. https://doi.org/10.1080/09581596.2022.2036701.
Krieger, N. 2011. Epidemiology and the people’s health: Theory and context. New York: Oxford University Press.
Kuh, D., et al. 2003. Life course epidemiology. Journal of Epidemiology & Community Health 57 (10): 778–783. https://doi.org/10.1136/jech.57.10.778.
Link, B.G., and J. Phelan. 1995. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior 35: 80–94.
Louvel, S., and A. Soulier. 2022. Biological embedding vs. embodiment of social experiences: How these two concepts form distinct thought styles around the social production of health inequalities. Social Science & Medicine 314: 115470. https://doi.org/10.1016/j.socscimed.2022.115470.
Lynch, J.W. 2000. Income inequality and mortality: Importance to health of individual income, psychosocial environment, or material conditions. British Medical Journal 320 (7243): 1200–1204. https://doi.org/10.1136/bmj.320.7243.1200.
Lynch, J. 2017. Reframing inequality? The health inequalities turn as a dangerous frame shift. Journal of Public Health 39 (4): 653–660. https://doi.org/10.1093/pubmed/fdw140.
Mao, F., et al. 2019. Social and spatial inequalities in allostatic load among adults in China: A multilevel longitudinal study. BMJ Open. https://doi.org/10.1136/bmjopen-2019-031366.
Marmot, M. 2004. Status syndrome: How your social standing directly affects your health and life expectancy. London: Bloomsbury Publications.
Marmot, M., and R.G. Wilkinson. 2001. Psychosocial and material pathways in the relation between income and health: A response to Lynch et al. British Medical Journal 322 (7296): 1233–1236.
McDade, T.W. 2008. Challenges and opportunities for integrative health research in the context of culture: A commentary on Gersten. Social Science & Medicine 66 (3): 520–524. https://doi.org/10.1016/j.socscimed.2007.09.005.
McEwen, B. 1998. Stress, adaptation, and disease—allostasis and allostatic load. Annals of the New York Academy of Sciences 840 (1): 33–44. https://doi.org/10.1111/j.1749-6632.1998.tb09546.x.
McEwen, B.S., and E. Stellar. 1993. Stress and the individual: Mechanisms leading to disease. Archives of Internal Medicine 153 (18): 2093–2101. https://doi.org/10.1001/archinte.1993.00410180039004.
McEwen, B.S., and J.C. Wingfield. 2003. The concept of allostasis in biology and biomedicine. Hormones and Behavior 43 (1): 2–15. https://doi.org/10.1016/S0018-506X(02)00024-7.
Meloni, M. 2014. How biology became social, and what it means for social theory. Sociological Review 62 (3): 593–614.
Meloni, M., et al. (eds.). 2018. The Palgrave handbook of biology and society. London: Palgrave.
Meloni, M., S. Williams, and P. Martin, eds. 2016. Biosocial matters: Rethinking sociology-biology relations in the twenty-first century. The Sociological Review 64 (1_suppl), 7–25.
Miller, G. 2021. Exposome: A new field, a new journal. Exposome 1 (1): 1–2. https://doi.org/10.1093/exposome/osab001.
Neser, W.B., H.A. Tyroler, and J.C. Cassel. 1971. Social disorganization and stroke mortality in the black population of the North California. American Journal of Epidemiology 93 (3): 166–175.
Niewöhner, J. 2011. Epigenetics: Embedded bodies and the molecularisation of biography and milieu. BioSocieties 6 (3): 279–298.
Niewöhner, J., and M. Lock. 2018. Situating local biologies: Anthropological perspectives on environment/human entanglements. BioSocieties 13 (4): 681–697. https://doi.org/10.1057/s41292-017-0089-5.
Pearce, N., et al. 1995. Limitations of biomarkers of exposure in cancer epidemiology. Epidemiology 6 (2): 190–194. https://doi.org/10.1097/00001648-199503000-00020.
Pollock, A. 2012. Medicating race: Heart disease and durable preoccupations with difference. Durham: Duke University Press.
Prior, L. 2021. Allostatic load and exposure histories of disadvantage. International Journal of Environmental Research and Public Health 18 (14): 7222. https://doi.org/10.3390/ijerph18147222.
Prior, L., D. Manley, and K. Jones. 2018. Stressed out? An investigation of whether allostatic load mediates associations between neighbourhood deprivation and health. Health & Place 52: 25–33. https://doi.org/10.1016/j.healthplace.2018.05.003.
Proctor, R.N., and L. Schiebinger. 2008. Agnotology: The making and unmaking of ignorance. Stanford: Stanford University Press.
Ribeiro, A.I., et al. 2018. Neighborhood socioeconomic deprivation and allostatic load: A scoping review. International Journal of Environmental Research and Public Health. https://doi.org/10.3390/ijerph15061092.
Richardson, S.S. 2017. Plasticity and programming: Feminism and the epigenetic imaginary. Signs: Journal of Women in Culture and Society 43 (1): 29–52.
Richardson, S.S., and H. Stevens, eds. 2015. Postgenomics: Perspectives on biology after the genome. Durham: Duke University Press.
Rose, G. 1992. The strategy of preventive medicine. Oxford: Oxford University Press.
Schrecker, T. 2013. Can health equity survive epidemiology? Standards of proof and social determinants of health. Preventive Medicine 57 (6): 741–744. https://doi.org/10.1016/j.ypmed.2013.08.013.
Seeman, T., et al. 1997. Price of adaptation—Allostatic load and its health consequences—MacArthur studies of successful aging. Archives of Internal Medicine 157 (19): 2259–2268.
Seeman, T., et al. 2001. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. PNAS 98 (8): 4770–4775. https://doi.org/10.1073/pnas.081072698.
Senier, L., et al. 2017. The socio-exposome: Advancing exposure science and environmental justice in a post-genomic era. Environmental Sociology 3 (2): 107–121. https://doi.org/10.1080/23251042.2016.1220848.
Shostak, S. 2013. Exposed science: Genes, the environment, and the politics of population health. Berkeley: University of California Press.
Sterling, P., and J. Eyer. 2005 [1988]. Allostasis: A new paradigm to explain arousal pathology. In Handbook of life stress, cognition and health, ed. S. Fisher and J. Reason, 629–649. Chichester: Wiley.
Strimbu, K., and J.A. Tavel. 2010. What are biomarkers? Current Opinion in HIV and AIDS 5 (6): 463–466. https://doi.org/10.1097/COH.0b013e32833ed177.
Szanton, S., J. Gill, and J. Allen. 2005. Allostatic load: A mechanism of socioeconomic health disparities? Biological Research for Nursing 7 (1): 7–15. https://doi.org/10.1177/1099800405278216.
Tabb, K., and M. Lemoine. 2021. The prospects of precision psychiatry. Theoretical Medicine and Bioethics 42 (5–6): 193–210. https://doi.org/10.1007/s11017-022-09558-3.
Townsend, P. 1987. Deprivation. Journal of Social Policy 16 (2): 125–146. https://doi.org/10.1017/S0047279400020341.
van Deurzen, I., et al. 2016. Neighborhood perceptions and allostatic load: Evidence from Denmark. Health & Place 40: 1–8. https://doi.org/10.1016/j.healthplace.2016.04.010.
Vineis, P., et al. 2020. Health inequalities: Embodied evidence across biological layers. Social Science & Medicine 246: 112781. https://doi.org/10.1016/j.socscimed.2019.112781.
Waitzkin, H. 1981. The social origins of illness: A neglected history. International Journal of Health Services 11 (1): 77–103. https://doi.org/10.2190/5CDV-P4FE-Y6HN-JACD.
Acknowledgements
All authors equally contributed to the research, conceptualization and writing of the article. T. Serviant-Fine additionally coordinated the writing. The authors would like to thank the Institut François Rabelais (ANR-17-CONV-0002 PLASCAN) for funding and supporting the EPIEXPO project which allowed for this research. Mathieu Arminjon’s contribution to this work is also supported by a grant from the Swiss National Science Foundation (SNSF), project “Acknowledging and Invisibilising Social Inequalities in Health: The Reception of World Health Organization Strategies in Switzerland and France from the 1970s to the present day” (Project No. 200460).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
The manuscript is comprised of original material and is not under review elsewhere. The research has been subjected to appropriate ethical review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Serviant-Fine, T., Arminjon, M., Fayet, Y. et al. Allostatic load: historical origins, promises and costs of a recent biosocial approach. BioSocieties (2023). https://doi.org/10.1057/s41292-023-00303-0
Accepted:
Published:
DOI: https://doi.org/10.1057/s41292-023-00303-0