Abstract
ABO blood types are putatively associated with the risk of venous thromboembolism (VTE), but it is not proved in Chinese people. A large population of Han Chinese patients discharged from Peking Union Medical College Hospital between January 2010 and June 2016 were retrospectively analyzed in a case-control study. A total of 1412 VTE patients were identified from 200,660 discharged Han Chinese patients, including 600 patients with deep vein thrombosis (DVT), 441 patients with pulmonary embolism, and 371 patients with both DVT and pulmonary embolism. The prevalence of non-O blood type was weakly but statistically higher in VTE patients compared with 199,248 non-VTE patients, with an odds ratio (OR) of 1.362 (95% confidence interval [CI], 1.205–1.540). Subgroup analysis showed that the OR for non-O blood type was still increased. It was greater in pre-hospital VTE (OR = 1.464) than that in hospital-acquired VTE (OR = 1.224), and greater in unprovoked VTE (OR = 1.859) than that in provoked VTE (OR = 1.227). The OR for non-O blood type decreased with age in subgroup analysis. These results suggest a weak but statistically significant correlation between non-O blood type and risk of VTE in Han Chinese people.
Similar content being viewed by others
Introduction
Venous thromboembolism (VTE), which encompasses both deep vein thrombosis (DVT) and pulmonary embolism, is an important cause of morbidity and mortality1. Both genetic and environmental factors contribute to the pathogenesis of VTE. Among genetic factors, ABO blood types profoundly influence hemostasis and are putatively associated with VTE2,3,4,5. Hospital- and blood donor-based studies have shown that people with non-O blood types have a greater risk of developing VTE than people with type O. This is likely due to the higher blood concentrations of factor VIII and von Willebrand factor in those with non-O blood types6,7. However, most hospital-based studies have been limited by small sample size, varying quality, and inconsistent outcomes. Hence, a hospital-based study with a large-scale population is imperative to corroborate previous findings.
The genetic profile for thrombosis of Chinese people differs from that of Caucasians. In particular, factor V Leiden and prothrombin G20210A are major risk factors of VTE in Caucasians, but are not detected in Chinese populations8. Therefore, it should be investigated whether ABO blood types are associated with the risk of VTE in Chinese people. In this study, we investigated a link between ABO blood types and VTE in a Han Chinese population by referencing a database of more than 200,000 patients who had been discharged from a tertiary hospital in China.
Results
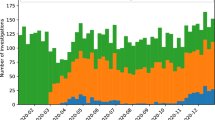
The data of 200,660 discharged Han patients who had been discharged between January 2010 and June 2016 were collected from the hospital database for this study. ABO blood type was determined from the ABO blood type database for each of these patients. From the Medical Record First Page (MRFP) database, 1443 (0.72%) of these patients had received a diagnosis of VTE. A review of these medical records excluded 31 patients. Therefore, 1412 patients with VTE were included in the case group, consisting of 600 DVT-only patients, 441 pulmonary embolism-only patients, and 371 patients with both DVT and pulmonary embolism. The remaining 199,248 patients were set as the control group. The mean age of all discharged patients was 47.5 years, but patients in the VTE group was much older (mean age, 57.3 years). Men constituted 45.1% of all VTE patients. In regard to precipitating factors, infection, cancer, surgery, arrhythmia, fracture, antiphospholipid syndrome and pregnancy accounted for 41.4%, 32.7%, 22.5%, 6.4%, 4.2%, 3.9% and 0.4% of all VTE patients, respectively.
Regarding the distribution of blood types, blood type O was the second-most prevalent phenotype (B > O > A > AB; Fig. 1) in non-VTE patients. However, blood type O was the third-most prevalent phenotype in VTE patients (B > A > O > AB).
The prevalence of non-O blood types was statistically higher in VTE patients compared with all the discharged non-VTE patients (Table 1), with an odds ratio (OR) of 1.362 (95% confidence interval [CI], 1.205–1.540). Adjusted OR was unchanged after adjustment for gender and age. Furthermore, in VTE patients when the non-O group was subclassified as blood types A, B, and AB, the ORs between each of these blood types and the O type were comparable to that between the general non-O group and the O group. Pairwise comparisons of the A, B, and AB blood types of the VTE patients and non-VTE patients revealed no statistical differences in ORs.
Subgroup analyses were listed in Table 2. The discharged VTE patients were stratified into DVT and pulmonary embolism subgroups. The prevalence of non-O blood type was statistically higher in both the DVT subgroup (OR = 1.484) and the pulmonary embolism subgroup (OR = 1.288). According to the time when VTE was diagnosed, VTE patients were stratified into patients with pre-hospital VTE and patients with hospital-acquired VTE. The prevalence of non-O blood type was statistically higher in patients with pre-hospital VTE (OR = 1.464) and in patients with hospital-acquired VTE (OR = 1.224). When precipitating factors were considered, VTE patients could be classified into unprovoked VTE and provoked VTE. Both these two subgroups had statistically increased ORs for non-O blood type, but OR was greater in unprovoked VTE patients (OR = 1.859) than that in provoked VTE patients (OR = 1.227). The OR of non-O blood type for VTE was also assessed in discharged male and female patients separately, and the value was unchanged. When VTE patients were stratified based on age, OR for non-O blood type decreased gradually with age, from 1.987 in patients <39 years, to 1.468 in patients 40–59 years, and then 1.157 in patients >60 years. Statistical difference was noted in patients <60 years, but not in patients >60 years. In subgroups with pre-hospital and hospital-acquired VTE cases, and with unprovoked and provoked VTE cases, when the mean ages were compared, a decreased OR was noted in the subgroup with an older mean age.
Discussion
In this case-control study, we analyzed the distribution of ABO blood types in a large-scale database containing more than 200,000 discharged Han Chinese patients, and found that the prevalence of non-O blood type was statistically higher in patients with VTE compared with non-VTE patients. This suggests that non-O blood types may carry a greater risk of VTE in Han Chinese people. To our best knowledge, this is the largest and probably only study reporting the association between ABO blood types and the risk of VTE in a population with a pure ethnic group.
A multitude of factors, genetic and environmental, contribute to the development of VTE. The ABO blood types have a substantial effect on hemostasis, and previously a number of studies have attempted to prove the association between ABO blood types and risk of developing VTE. Most of the studies were hospital-based or blood donor-based, and had small sample size, varying quality, and inconsistent outcomes. Two meta-analyses performed in 2008 and 2012 both showed increased ORs (1.79 and 2.09, respectively) for non-O blood types in VTE patients compared with non-VTE controls3,9. Vasan et al.10 recently revealed an association between ABO blood types and the risk of VTE, based on 1.5 million blood donors. However, blood donors differed from the general population in environmental variables and genetic factors11. Therefore, the association between ABO blood types and the risk of VTE still requires verification in other large-scale populations. To our best knowledge, this study is the largest hospital-based study to investigate a correlation between ABO blood types and the risk of VTE, and further provides evidence that non-O blood types increase the risk of VTE compared with blood type O.
When subgroups were analyzed, the most impressive result was that the OR of non-O blood type for VTE decreased with age, not only in discharged patients stratified by age, but also in subgroups with pre-hospital and hospital-acquired VTE cases, and with unprovoked and provoked VTE cases, indicating that age is a confounder in this study. It is already known that ABO blood types are associated with the risk of VTE not only in unprovoked cases12, but also in provoked cases, such as cancer13,14, pregnancy15, trauma16 or post-surgery17,18. Meta-analysis showed that the prevalence of non-O blood types is higher in unprovoked VTE cases (OR = 1.88) than in provoked cases (OR = 1.33)3. ORs in our present study in regard to precipitating factors were similar to that described in the literature. The finding that ABO blood type was more associated with unprovoked VTE further proves its role as a genetic risk factor. How precipitating factors influence the association between ABO blood types and the risk of VTE are still unknown. Because provoked VTE patients have an older mean age, and age seems to be a confounder in this study, the difference between provoked and unprovoked VTE subgroups may be explained, at least partially, by age. We also found that non-O blood type was associated with VTE more in patients with pre-hospital VTE than that in patients with hospital-acquired VTE. Since hospitalized patients are usually older and have more precipitating factors than pre-hospital cases, this finding seems scientifically understandable.
Individuals with a non-O blood type have higher levels of factor VIII and von Willebrand factor compared with individuals with blood type O6,7. Elevated factor VIII or von Willebrand factor has been shown to be a moderate risk factor for VTE19. Therefore, factor VIII and von Willebrand factor are potentially involved in the correlation between ABO blood types and development of VTE. However, some studies have shown that a non-O blood type carries a risk of VTE, independent of factor VIII20,21. Other possible mechanisms include the influence of genetic variation in the ABO locus on serum levels of inflammatory markers22,23,24. Hence, the exact mechanisms underlying a higher risk of VTE in non-O blood types are complicated and need further exploration.
In the present study, we noted that the proportion of non-O blood types in the Han Chinese population was about 70%, which is much higher than that of Caucasians (50–60%)10,20,25,26. Thus, theoretically a higher proportion of VTE should occur in Chinese people, since non-O blood types are a risk factor. However, on the contrary, incidences of VTE in the Chinese subjects of this study and in the literature were much lower than that reported for Caucasians27,28,29,30. Therefore, it can be deduced that some risk factors other than ABO blood types also contribute significantly to the development of VTE in Caucasians. It is already known that the genetic profile for hemostasis and thrombosis in Chinese people is quite different from that of Caucasians8, and it is likely that the genetic difference other than ABO blood types between Chinese and Caucasians contributes to the lower incidence of VTE in Chinese. Furthermore, environmental factors such as dietary habit may also contribute to the risk of VTE and cause the different incidence of VTE in different ethnic groups. A similar phenomenon was also observed between Caucasians and African Americans20.
In the present investigation, the following measures were taken to enhance the credibility of the results. First, we used the clinical laboratory to obtain ABO blood type data, as the records for blood type were more accurate than those recorded in the MRFP database. Second, in the analysis phase, VTE patients were further analyzed with a multivariable logistic regression model adjusted for gender and age. Besides, five categories of subgroups were analyzed separately. The prevalence of non-O blood type remains unchanged in regression analysis and in subgroup analysis, further confirming the credibility of the results.
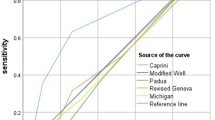
It needs attention that although compression venous ultrasonography, computed tomographic pulmonary angiography, and ventilation-perfusion scintigraphy are widely used in the diagnosis of DVT and pulmonary embolism in our hospital, underreporting of VTE patients still may exist in this study. However, such possible underreporting would not be associated with genetic ABO blood types. Thus, VTE patients with non-O and O blood types are equally likely to be underreported. When the actual OR is >1, the OR in the presence of underreporting is less than the actual OR (see Supplementary Fig. S1). In other words, the actual OR should be larger than the OR presented here.
In brief, this study utilized a hospital-based database of more than 200,000 discharged patients to confirm a weak but statistically significant association between ABO blood types and the risk of VTE in a Han Chinese population. The implications of this association and its predictive value in VTE warrant further exploration.
Methods
Data sources
Data were retrieved from 2 databases at Peking Union Medical College Hospital, Beijing, China. One is MRFP database, located in the medical records room. For each discharged patient, the MRFP contains the following: name; gender; date of birth; ethnic group; dates and departments of admission and discharge; up to 20 discharge diagnoses based on the International Statistical Classification of Diseases and Related Health Problems Tenth Revision (ICD-10); and surgical procedures. The other database, in the clinical laboratory, contains the ABO blood types of all patients tested for blood type.
Study design
This was a retrospective case-control study. The main objective was to analyze the association between ABO blood types and the risk of VTE before and during hospitalization. The MRFP database was searched for diagnostic codes indicating DVT or pulmonary embolism in all discharged patients with diagnoses between January 2010 and June 2016. For patients with multiple admissions, only the first was considered. Medical records were then reviewed to verify the diagnosis of VTE. DVT was confirmed by compression venous ultrasonography or computed tomographic venography, and pulmonary embolism was confirmed by computed tomographic pulmonary angiography or ventilation-perfusion scintigraphy. Following details in VTE patients were also retrieved for subgroup analysis: (1) the time when VTE developed; and (2) precipitating factors for VTE, including infection, cancer, surgery, fracture, pregnancy, cardiac arrhythmia, and antiphospholipid syndrome.
Because the distribution of ABO blood type groups differs among ethnicities, in the present study the ethnic group was restricted to Han Chinese, which constitutes 90% of the total population in China. The ABO type of each patient was retrieved from the ABO blood type database. Therefore, the case group consisted of Han Chinese individuals with known blood types, who had received a diagnosis of DVT or pulmonary embolism and who had been discharged from Peking Union Medical College Hospital between January 2010 and June 2016.
The control group consisted of all hospitalized non-VTE Han patients with determined blood types between January 2010 and June 2016; for subjects with multiple admissions, only the first was considered. Age and gender were retrieved for every discharged patient.
The study was approved by the Ethical Committee of Peking Union Medical College Hospital (Reference Number: S-K150). Due to the retrospective nature of the study and no identifying information relating to participants was included, written informed consent was waived. All experiments protocols were conducted according to the Strengthening the Reporting of Observational Studies in Epidemiology guidelines.
Statistical analysis
Subjects with diagnoses of both DVT and pulmonary embolism contributed to both of the outcome categories. Demographic characteristics were described as mean + standard deviation (SD) for continuous variables and as percentages for categorical variables. Means or prevalence for baseline variables of interest were compared between VTE cases and controls, using independent sample t-tests or chi-squared (χ2) tests. ORs with 95% CIs for certain blood types in VTE patients were assessed with logistic regression models. All data were analyzed using the Statistical Package for the Social Sciences software (SPSS, version 19.0; SPSS, Chicago, Illinois, USA). P-values < 0.05 were considered statistically significant.
Additional Information
How to cite this article: Sun, X. et al. ABO blood types associated with the risk of venous thromboembolism in Han Chinese people: A hospital-based study of 200,000 patients. Sci. Rep. 7, 42925; doi: 10.1038/srep42925 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Cohen, A. T. et al. Venous thromboembolism (VTE) in Europe. The number of VTE events and associated morbidity and mortality. Thromb Haemost 98, 756–764 (2007).
Preston, A. E. & Barr, A. The Plasma Concentration of Factor Viii in the Normal Population. Ii. The Effects of Age, Sex and Blood Group. Br J Haematol 10, 238–245 (1964).
Dentali, F. et al. Non-O blood type is the commonest genetic risk factor for VTE: results from a meta-analysis of the literature. Semin Thromb Hemost 38, 535–548, doi: 10.1055/s-0032-1315758 (2012).
Dentali, F., Sironi, A. P., Ageno, W., Crestani, S. & Franchini, M. ABO blood group and vascular disease: an update. Semin Thromb Hemost 40, 49–59, doi: 10.1055/s-0033-1363460 (2014).
Franchini, M. & Liumbruno, G. M. ABO blood group: old dogma, new perspectives. Clinical chemistry and laboratory medicine 51, 1545–1553, doi: 10.1515/cclm-2013-0168 (2013).
Souto, J. C. et al. Functional effects of the ABO locus polymorphism on plasma levels of von Willebrand factor, factor VIII, and activated partial thromboplastin time. Arteriosclerosis, thrombosis, and vascular biology 20, 2024–2028 (2000).
Schleef, M. et al. Relationship between ABO and secretor genotype with plasma levels of factor VIII and von Willebrand factor in thrombosis patients and control individuals. Brit J Haematol 128, 100–107, doi: 10.1111/j.1365-2141.2004.05249.x (2005).
Wang, C., Zhai, Z., Shen, Y. H. & Zhao, L. Clinical and genetic risk factors for venous thromboembolism in Chinese population. Front. Med. China 4, 29–35 (2010).
Wu, O., Bayoumi, N., Vickers, M. A. & Clark, P. ABO(H) blood groups and vascular disease: a systematic review and meta-analysis. J Thromb Haemost 6, 62–69, doi: 10.1111/j.1538-7836.2007.02818.x (2008).
Vasan, S. K. et al. ABO Blood Group and Risk of Thromboembolic and Arterial Disease: A Study of 1.5 Million Blood Donors. Circulation 133, 1449–1457, discussion 1457, doi: 10.1161/CIRCULATIONAHA.115.017563 (2016).
Golding, J., Northstone, K., Miller, L. L., Davey Smith, G. & Pembrey, M. Differences between blood donors and a population sample: implications for case-control studies. International journal of epidemiology 42, 1145–1156, doi: 10.1093/ije/dyt095 (2013).
Canonico, M. et al. Synergism between non-O blood group and oral estrogen in the risk of venous thromboembolism among postmenopausal women: The ESTHER study. Thromb Haemost 99, 246–248, doi: 10.1160/TH07-09-0536 (2008).
Streiff, M. B., Segal, J., Grossman, S. A., Kickler, T. S. & Weir, E. G. ABO blood group is a potent risk factor for venous thromboembolism in patients with malignant gliomas. Cancer 100, 1717–1723, doi: 10.1002/cncr.20150 (2004).
Li, D. et al. ABO non-O type as a risk factor for thrombosis in patients with pancreatic cancer. Cancer Med 4, 1651–1658, doi: 10.1002/cam4.513 (2015).
Larsen, T. B. et al. ABO blood groups and risk of venous thromboembolism during pregnancy and the puerperium. A population-based, nested case-control study. J Thromb Haemost 3, 300–304, doi: 10.1111/j.1538-7836.2005.01195.x (2005).
Muellner, S. K., Haut, E. R., Streiff, M. B., Holcomb, J. B. & Cotton, B. A. ABO blood group as a potential risk factor for venous thromboembolism in acutely injured patients. Thromb Haemost 105, 5–13, doi: 10.1160/TH10-08-0504 (2011).
Kodama, J. et al. D-dimer level as a risk factor for postoperative venous thromboembolism in Japanese women with gynecologic cancer. Annals of oncology: official journal of the European Society for Medical Oncology/ESMO 21, 1651–1656, doi: 10.1093/annonc/mdq012 (2010).
Wang, J. K. et al. Non-O blood type is associated with an increased risk of venous thromboembolism after radical cystectomy. Urology 83, 140–145, doi: 10.1016/j.urology.2013.08.046 (2014).
Martinelli, I. von Willebrand factor and factor VIII as risk factors for arterial and venous thrombosis. Seminars in hematology 42, 49–55 (2005).
Ohira, T. et al. ABO blood group, other risk factors and incidence of venous thromboembolism: the Longitudinal Investigation of Thromboembolism Etiology (LITE). J Thromb Haemost 5, 1455–1461, doi: 10.1111/j.1538-7836.2007.02579.x (2007).
Tirado, I. et al. The ABO blood group genotype and factor VIII levels as independent risk factors for venous thromboembolism. Thromb Haemost 93, 468–474, doi: 10.1160/TH04-04-0251 (2005).
Pare, G. et al. Novel association of ABO histo-blood group antigen with soluble ICAM-1: results of a genome-wide association study of 6,578 women. PLoS genetics 4, e1000118, doi: 10.1371/journal.pgen.1000118 (2008).
Melzer, D. et al. A genome-wide association study identifies protein quantitative trait loci (pQTLs). PLoS genetics 4, e1000072, doi: 10.1371/journal.pgen.1000072 (2008).
Barbalic, M. et al. Large-scale genomic studies reveal central role of ABO in sP-selectin and sICAM-1 levels. Human molecular genetics 19, 1863–1872, doi: 10.1093/hmg/ddq061 (2010).
Garratty, G., Glynn, S. A., McEntire, R. & Retrovirus Epidemiology Donor, S. ABO and Rh(D) phenotype frequencies of different racial/ethnic groups in the United States. Transfusion 44, 703–706, doi: 10.1111/j.1537-2995.2004.03338.x (2004).
Wolpin, B. M. et al. Prospective study of ABO blood type and the risk of pulmonary embolism in two large cohort studies. Thromb Haemost 104, 962–971, doi: 10.1160/TH10-05-0312 (2010).
Holcomb, C. N., DeRussy, A., Richman, J. S. & Hawn, M. T. Association Between Inpatient Surveillance and Venous Thromboembolism Rates After Hospital Discharge. JAMA Surg 150, 520–527, doi: 10.1001/jamasurg.2015.35 (2015).
Proctor, M. C., Wainess, R. M., Henke, P. K., Upchurch, G. R. & Wakefield, T. W. Venous thromboembolism: regional differences in the nationwide inpatient sample, 1993 to 2000. Vascular 12, 374–380 (2004).
Gallerani, M., Reverberi, R. & Manfredini, R. ABO blood groups and venous thromboembolism in a cohort of 65,402 hospitalized subjects. European journal of internal medicine 25, e27–28, doi: 10.1016/j.ejim.2013.10.002 (2014).
Cheuk, B. L., Cheung, G. C. & Cheng, S. W. Epidemiology of venous thromboembolism in a Chinese population. The British journal of surgery 91, 424–428, doi: 10.1002/bjs.4454 (2004).
Acknowledgements
This study was supported by the Ministry of Science and Technology of China “Precision Medicine Project” 2016YFC0905603.
Author information
Authors and Affiliations
Contributions
X. Sun, J. Feng: study conception and design, data collection, analysis and interpretation, paper writing; W. Wu, M. Peng: study design, data collection and critical revision; J. Shi: study conception and design, data interpretation and critical revision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Sun, X., Feng, J., Wu, W. et al. ABO blood types associated with the risk of venous thromboembolism in Han Chinese people: A hospital-based study of 200,000 patients. Sci Rep 7, 42925 (2017). https://doi.org/10.1038/srep42925
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep42925
This article is cited by
-
Association of blood group and red blood cell transfusion with the incidence of antepartum, peripartum and postpartum venous thromboembolism
Scientific Reports (2019)
-
Association of the CYP4V2 polymorphism rs13146272 with venous thromboembolism in a Chinese population
Clinical and Experimental Medicine (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.