Abstract
Targeting myeloid differentiation protein 2 (MD-2) or Toll-like receptor 4 (TLR4) with small molecule inhibitor rescues the systemic inflammatory response syndrome (SIRS) in sepsis due to infection with Gram-negative bacteria but not other microbes. Herein, we provided IκB kinase β (IKKβ) in innate immune process as a molecular target of caffeic acid cyclohexylamide (CGA-JK3) in the treatment of polymicrobial TLR agonists-induced lethal inflammation. CGA-JK3 ameliorated E. coli lipopolysaccharide (LPS, MD-2/TLR4 agonist)-induced endotoxic shock, cecal ligation and puncture (CLP)-challenged septic shock or LPS plus D-galactosamine (GalN)-induced acute liver failure (ALF) in C57BL/6J mice. As a molecular basis, CGA-JK3 inhibited IKKβ-catalyzed kinase activity in a competitive mechanism with respect to ATP, displaced fluorescent ATP probe from the complex with IKKβ, and docked at the ATP-binding active site on the crystal structure of human IKKβ. Furthermore, CGA-JK3 inhibited IKKβ-catalyzed IκB phosphorylation, which is an axis leading to IκB degradation in the activating pathway of nuclear factor-κB (NF-κB), in macrophages stimulated with TLR (1/2, 2/6, 4, 5, 7, 9) agonists from Gram-positive/negative bacteria and viruses. CGA-JK3 consequently interrupted IKKβ-inducible NF-κB activation and NF-κB-regulated expression of TNF-α, IL-1α or HMGB-1 gene, thereby improving TLRs-associated redundant inflammatory responses in endotoxemia, polymicrobial sepsis and ALF.
Similar content being viewed by others
Introduction
Sepsis, a manifestation of SIRS, has been refined as a life-threatening organ dysfunction caused by a dysregulated host response to infection with bacteria most commonly, but also viruses or fungi1. Pharmacotherapy of sepsis patients remains elusive. In particular, lipid A derivative Eritoran and non-lipid chemical TAK-242 have completed clinical trials in the treatment of severe sepsis but failed to improve survival rates of sepsis patients; however, the clinical trials recruited patients based on a risk of death but did not consider the etiology of infected pathogens2,3,4. Eritoran antagonizes LPS binding to the receptor MD-2 associated with TLR4, and TAK-242 interacts with the Cys-747 residue on intracellular domain of TLR4, thereby blocking inflammatory responses in sepsis specially due to Gram-negative bacterial infection but not other microbes5,6. Therefore, novel therapeutic target responding to TLR pathogens from Gram-positive bacteria and viruses, affecting redundant SIRS pathways other than MD-2 or TLR4, is required in the alternative treatment of sepsis patients.
Mammalian TLRs sense not only pathogen-associated molecular patterns from microbes but also danger-associated molecular pattern molecules from dying host cells. They transmit the innate immune responses via intracellular adaptor molecules such as myeloid differentiation factor 88 (MyD88) and toll/IL-1 receptor-containing adaptor inducing interferon (IFN)-β (TRIF)7. For immune responses, MyD88 is recruited to several TLRs including TLR1/2, 2/6, 4, 5, 7/8, and 9, while TRIF is specific to TLR3 and 47. TLR/MyD88-dependent pathway stimulates auto-phosphorylation of IL-1 receptor-associated kinase 4 (IRAK-4) and subsequently TGF-β-activating kinase 1 (TAK1)8. In turn, TAK1 phosphorylates IKK complex in the activating pathway of NF-κB or stimulates mitogen-activated protein kinases such as JNK and p38 for transcriptional activity of activating protein 1 (AP-1)9. Transcription factor NF-κB or AP-1 triggers expression of inflammatory genes encoding TNF-α, IL-1α, HMGB-1 or inducible nitric oxide (NO) synthase (iNOS)10. On the other hand, TLR/TRIF-dependent pathway activates transcription factor IRF3 via TNF receptor (TNFR)-associated factor family member-associated NF-κB activator-binding kinase 1 (TBK1), which up-regulates expression of IFN-β or IP-10 gene11.
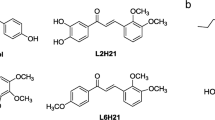
Caffeic acid derivatives are enriched in numerous medicinal plants. They protect from sepsis-related disorders in rodents12,13,14,15. In particular, lonicerae flos extract containing caffeic acid quinate (chlorogenic acid) as a major anti-inflammatory constituent is undergoing clinical trial for sepsis treatment. However, their mechanisms remain to be clarified. In the current study, we focused on molecular basis of caffeic acid cyclohexylamide (CGA-JK3, Supplementary Fig. 1A) in the treatment of TLRs-associated redundant inflammatory responses in endotoxemia, polymicrobial sepsis or ALF, and proposed IKKβ inhibition as a potential therapeutic target.
Results
CGA-JK3 rescues endotoxic or septic mice
C57BL/6J mice were intraperitoneally (i.p.) injected with LPS (40 mg/kg) for endotoxic shock or challenged with CLP for polymicrobial sepsis, and treated with vehicle, CGA-JK3 or TAK-242 intravenously (i.v.) at 1 h after LPS or CLP challenge. TAK-242, a drug candidate with molecular mechanism of TLR4 inhibition, was used as a positive control agent3,6. LPS alone-injected mice that developed endotoxic shock were time-dependently sacrificed (Fig. 1A). Treatment with CGA-JK3 decreased mortality rates of endotoxic mice, as did TAK-242 (Fig. 1A,B). CLP alone-challenged mice were time-dependently died due to polymicrobial sepsis (Fig. 1C). The CGA-JK3 (100 mg/kg)-treated group showed 80% survival rate, as compared to <15% survival in the vehicle alone-treated group (Fig. 1C,D), indicating that CGA-JK3 treatment also rescued the septic mice. On the other hand, TAK-242 as a positive control agent showed much lower effectiveness on CLP model than on endotoxemia model (Fig. 1B,D), suggesting different mode of action from CGA-JK3. In endotoxic mice, blood levels of TNF-α increased to maximal values at 2 h after LPS intoxication (Fig. 1E), IL-1α levels at 6 h (Fig. 1F), and HMGB-1 levels at 10 h (Fig. 1G). Treatment with CGA-JK3 attenuated LPS-induced TNF-α, IL-1α or HMGB-1 levels in the blood (Fig. 1E–G), thus improving the cytokine storm in vivo.
C57BL/6J mice (each group, n = 9–12) were intraperitoneally injected with LPS (40 mg/kg) for endotoxic shock or challenged with CLP for polymicrobial sepsis, and treated with vehicle, CGA-JK3 or TAK-242 intravenously at 1 h after each intoxication. Survival rates were examined until 4 days after LPS challenge (A,B) or 6 days after CLP challenge (C,D). Blood samples were collected at 2 h, 6 h or 10 h after LPS challenge, and sera were then loaded onto ELISA kits. Systemic levels TNF-α (E), IL-1α (F) or HMGB-1 (G) are expressed as a solid circle (⦁) in the LPS plus vehicle alone-treated group, and an open circle (о) in the LPS plus CGA-JK3 (100 mg/kg)-treated group. Data are mean ± SEM. *P < 0.05 vs. LPS- or CLP alone-challenged group.
CGA-JK3 ameliorates ALF in mice
LPS plus GalN (LPS/GalN)-induced ALF is also known as a TLR-associated lethal disorder with apoptotic death of hepatocytes in the liver, but differs from the multi-organ injury in sepsis or endotoxemia that involves necrosis with minimal apoptosis16,17. LPS (10 μg/kg)/GalN (500 mg/kg)-injected mice were time-dependently died as a result of ALF, while LPS (10 μg/kg)- or GalN (500 mg/kg) alone-injected mice did not (Fig. 2A). C57BL/6J mice were injected with LPS/GalN (i.p.) for ALF, and treated with vehicle, CGA-JK3 or silymarin (i.v.) at 1 h after LPS/GalN intoxication. Silymarin, a hepatoprotective drug that contains flavolignans, was used as a positive control agent18. Treatment with CGA-JK3 or silymarin reduced mortality rates of LPS/GalN-challenged mice with ALF, such that about 70% of the mice survived in the CGA-JK3 (100 mg/kg)- or silymarin (50 mg/kg)-treated group, while most of them died in the vehicle alone-treated group (Fig. 2A,B). LPS/GalN-challenged mice drastically increased aspartate aminotransferase (AST) or bilirubin levels in the blood, which are known as biochemical markers of severe liver injury (Supplementary Fig. 1B,C). Treatment with CGA-JK3 decreased AST or bilirubin levels in the blood of ALF-induced mice (Supplementary Fig. 1B,C). Concurrently, CGA-JK3 or silymarin ameliorated LPS/GalN-induced tissue injury, especially congestion and parenchymal degeneration in the hepatic lobules (Fig. 2C).
C57BL/6J mice (each group, n = 9–12) were intraperitoneally injected with LPS (10 μg/kg) plus GalN (500 mg/kg) for ALF, and treated with vehicle, CGA-JK3 or silymarin intravenously at 1 h after LPS/GalN intoxication. (A,B) Survival rates were examined until 24 h after LPS, GalN or LPS/GalN challenge. (C) Hepatic lobules were fixed in formalin and embedded in paraffin. The specimens were sectioned serially, and stained with hematoxylin and eosin. The scale bars are 100 μm. Hepatic injury index were scored as described in Methods. Data are mean ± SEM. #P < 0.05 vs. vehicle alone-injected group. *P < 0.05 vs. LPS/GalN alone-injected group. (D) Cell extracts were prepared from the liver tissues, and subjected to Western blot analysis (WB) with paired antibodies against p-NF-κB p65 and total NF-κB, p-c-Jun and total c-Jun or p-IRF3 and total IRF3. (E) Total RNAs were prepared from the liver tissues, and subjected to RT-PCR analysis to determine mRNA levels of TNF-α, IL-1α or IFN-β with β-actin as an internal control.
To understand whether CGA-JK3 affected TLR-associated immune process, we examined the active indexes via specific phosphorylation of NF-κB p65 at the Ser-536 residue, c-Jun at the Ser-63 residue or IRF3 at the Ser-396 residue19,20. Treatment with CGA-JK3 decreased phospho (p)-NF-κB p65 levels in the liver with LPS/GalN-induced ALF, but not p-c-Jun and p-IRF3 levels (Fig. 2D). Moreover, treatment with CGA-JK3 suppressed mRNA levels of NF-κB-target genes encoding TNF-α and IL-1α in the liver, but not those of IRF3-target IFN-β gene (Fig. 2E). On the other hand, silymarin as a positive control agent inhibited LPS/GalN-induced phosphorylation of c-Jun or IRF3 in addition to NF-κB p65, and suppressed mRNA levels of TNF-α, IL-1α and IFN-β (Fig. 2D,E), suggesting different mechanism from CGA-JK3.
CGA-JK3 inhibits IκBα phosphorylation in macrophages
CGA-JK3 showed no effect on binding of fluorescent LPS probe (LPS-FITC) to extracellular MD-2 associated with transmembrane TLR4 in macrophages, whereas lipid IVa (MD-2 antagonist) resulted in inhibition of the binding (Fig. 3A), thus excluding the possibility of direct effect of CGA-JK3 on the receptor or LPS scavenging. To elucidate a molecular mechanism of CGA-JK3, we examined the phosphorylation of IκBα at the Ser-32 and Ser-36 residues, a cellular substrate of IKKβ, because it decreased protein or mRNA levels of NF-κB-target genes in vivo (Figs 1E–G and 2D,E). CGA-JK3 inhibited LPS-induced IκBα phosphorylation in mouse peritoneal macrophages or RAW 264.7 monocytic cells (Fig. 3B,C). CGA-JK3 also inhibited Pam3CSK4 (TLR1/2 agonist mimicking the triacylated lipoprotein from Gram-positive bacteria)-, FSL-1 (TLR2/6 agonist mimicking the diacylated lipoprotein from Mycoplasma fermentans)-, flagellin (TLR5 agonist from bacterial flagellar filament)-, ssRNA (TLR7 agonist mimicking the viral RNAs)- or CpG ODN (TLR9 agonist mimicking the bacterial or viral unmethylated CpG DNA)-induced IκBα phosphorylation in RAW 264.7 cells (Fig. 3D). Furthermore, CGA-JK3 inhibited TNF-α-, IL-1α- or HMGB-1-induced IκBα phosphorylation in the cells (Fig. 3E).
(A) RAW 264.7 cells were incubated with LPS-FITC (1 μg/ml) for 30 min in the presence of CGA-JK3 (30 μM) or lipid IVa (100 nM). After washing, the cells were subjected to flow cytometric analysis. Mouse peritoneal macrophages (B) or RAW 264.7 cells (C) were pretreated with CGA-JK3 for 2 h and stimulated with LPS for 10–20 min in the presence of CGA-JK3. RAW 264.7 cells were pretreated with CGA-JK3 for 2 h and stimulated with TLR agonists (D) or cytokines (E) for 10–20 min in the presence of CGA-JK3. Cell extracts were subjected to Western blot analysis (WB) with anti-p-IκBα or anti-IκBα antibody.
However, CGA-JK3 showed no effect on the Pam3CSK4- or LPS-stimulated auto-phosphorylation of IRAK-4 at the Thr-345 and Ser-346 residues in RAW 264.7 cells or the TNF-α- or LPS-stimulated auto-phosphorylation of TAK1 at the Thr-184 and Thr-187 residues, in which IS409 (IRAK-1/4 inhibitor) and LLZ 1640–2 (TAK1 inhibitor) were used as positive control agents (Supplementary Fig. 2A,B). CGA-JK3 at concentrations up to 30 μM did not disturb the viability of RAW 264.7 cells (Supplementary Fig. 2C), excluding the possibility of nonspecific cytotoxicity. The results suggested that CGA-JK3 inhibited IKKβ-catalyzed IκBα phosphorylation in macrophages stimulated with various TLR agonists from bacteria and viruses or with endogenous cytokines, while it did not affect TLR- or TNFR-recruited early signal transducers, including IRAK-4 and TAK1, that are located upstream from IKKβ.
CGA-JK3 is an ATP-competitive inhibitor of IKKβ-catalyzed kinase activity
To understand whether CGA-JK3 directly inhibited the kinase activity of IKKβ, catalytically active rhIKKβ was treated with CGA-JK3 in cell-free reactions and then reacted with IKK substrate peptide (IKKtide) in the presence of [γ-32P]ATP probe. CGA-JK3 dose-dependently inhibited the rhIKKβ-catalyzed kinase activity, as did sulfasalazine and BMS 345541 as positive control agents (Fig. 4A). Sulfasalazine, a FDA-approved drug for rheumatoid arthritis or inflammatory bowel disease with chronic inflammation, is an ATP-competitive inhibitor of IKKβ activity, and BMS 345541 is an allosteric inhibitor21,22. In a kinetic study, rhIKKβ exhibited a Km value of 0.93 μM and a Vmax value of 13,400 Δcpm/min with varying concentrations of ATP (Fig. 4B,C). Treatment with CGA-JK3 increased the Km value but did not alter the Vmax value of IKKβ-catalyzed kinase activity (Fig. 4B), suggesting a competitive mechanism with respect to ATP. Sulfasalazine as a positive control agent also increased the Km value without altering the Vmax value, as did CGA-JK3, but BMS 345541 changed both Km and Vmax values (Fig. 4C). However, CGA-JK3 did not inhibit the kinase activities of cell-free rhIRAK-4, rhJNK or rhTBK1 that are also associated with TLR-dependent immune process, in which IS409, SP 600125 and amlexanox were used as positive control agents (Fig. 4D–F). SP 600125 is an ATP-competitive inhibitor of JNK activity and amlexanox is an ATP-competitive inhibitor of TBK1 activity23,24.
Catalytically active rhIKKβ (A–C), rhIRAK-4 (D), rhJNK (E) or rhTBK1 (F) was treated with CGA-JK3 for 10 min in cell-free reactions. In vitro kinase assay was then monitored by incorporation of [32P] from the probe [γ-32P]ATP onto IKKtide (A–C) or MBP (D–F) as exogenous substrate. Data are mean ± SEM from three independent experiments using the average values of triplicate in each experiment. *P < 0.05 vs. rhIKKβ- or other protein kinase alone-containing group. (B,C) Kinetic data of rhIKKβ-catalyzed kinase activity are represented as mean values of 1/V, an inverse of the initial increase of cpm values per min (Δcpm/min), from three independent experiments with varying concentrations of ATP.
To clarify whether CGA-JK3 interacted with the ATP-binding site of IKKβ, fluorescent ATP probe (2′,3′-O-(2,4,6-trinitrophenyl)adenosine triphosphate, ATP-TNP) was pre-incubated with rhIKKβ in cell-free reactions to achieve stable fluorescence intensity, and then treated with CGA-JK3. The fluorescence intensity of ATP-TNP was markedly increased following its binding to rhIKKβ (Fig. 5A). Post-treatment with CGA-JK3 dose-dependently decreased rhIKKβ-enhanced fluorescence values of ATP-TNP (Fig. 5A), indicating displacement of ATP-TNP from the complex with rhIKKβ. However, non-fluorescent CGA-JK3 did not alter basal fluorescence values of ATP-TNP in the absence of rhIKKβ (Fig. 5B). Consistent with in vitro kinase assays (Fig. 4E,F), CGA-JK3 did not affect ATP-TNP binding to rhJNK or rhTBK1, in which SP 600125 and amlexanox were used as positive control agents (Fig. 5C,D).
(A) ATP-TNP (3 μM) was pre-incubated with rhIKKβ (100 ng) for 2 h in cell-free reactions to achieve stable fluorescence values under excitation at 400 nm, and then treated with CGA-JK3 for another 2 h. Emission spectra at 500–610 nm are represented as relative fluorescence units (RFU). ATP-TNP was pre-incubated with rhIKKβ (B), rhJNK (C) or rhTBK1 (D) for 2 h in cell-free reactions and then treated with CGA-JK3 for another 2 h. Fluorescence values are represented as RFU under excitation at 400 nm and emission at 550 nm. Data are mean ± SEM from three independent experiments using the average values of triplicate in each experiment. #P < 0.05 vs. ATP-TNP alone-containing group. *P < 0.05 vs. ATP-TNP plus rhIKKβ- or ATP-TNP plus other protein kinase alone-containing group. (E) Docking arrangement of CGA-JK3 to the crystal structure of human IKKβ was carried out with the Surflex-Dock program. CGA-JK3 is represented as a green color, catalytic residues on the ATP-binding active site of IKKβ as a grey color, and the other IKKβ backbone as a violet color. Hydrogen bonding between CGA-JK3 and IKKβ is indicated as a yellow dotted line.
Based on the evidences showing that CGA-JK3 inhibited the kinase activity of IKKβ in a competitive mechanism with respect to ATP and displaced fluorescent ATP probe from the complex with IKKβ, we conducted molecular docking with the crystal structure of human IKKβ25. CGA-JK3 was well fitted into the ATP-binding active site of IKKβ with close contacts to the Val-29, Val-74, Cys-99, Asp-103 and Ile-165 residues under the most energetically favorable simulation (Fig. 5E). Hydrogen bonding was achieved between the amide carbonyl group of CGA-JK3 and the peptidyl amino backbone of Cys-99 residue, and between the phenolic hydroxyl group of CGA-JK3 and the peptidyl amino backbone of Asp-103 residue (Fig. 5E). The cyclohexyl moiety of CGA-JK3 was exposed to a hydrophobic environment consisting with Val-29, Val-74 and Ile-165 (Fig. 5E). Moreover, the docking simulation of CGA-JK3 overlapped with that of endogenous ligand, ATP bound to IKKβ (Supplementary Fig. 3).
CGA-JK3 suppresses the transcriptional activity of NF-κB but not AP-1 or IRF3
In Pam3CSK4- or LPS-activated RAW 264.7 cells, treatment with CGA-JK3 sequentially inhibited IκBα degradation (Fig. 6A), nuclear import of NF-κB p65 (Fig. 6B), and transcriptional activity of NF-κB (Fig. 6C), which are located downstream from IKKβ-catalyzed IκBα phosphorylation in the NF-κB activating pathway10. To determine whether the effect of CGA-JK3 on NF-κB activation was reversible. RAW 264.7 cells harboring NF-κB-secretory alkaline phosphatase (SEAP) construct, a reporter of NF-κB transcriptional activity, were pre-incubated with CGA-JK3 for 2–4 h, allowed to recover in complete media after washing, and then stimulated with LPS. CGA-JK3 did not affect LPS-induced NF-κB transcriptional activity when it was washed out before LPS stimulation (Fig. 6D), suggesting a reversible mechanism of action. To determine whether IKKβ was a primary target of CGA-JK3 in the suppression of NF-κB activating pathway, we transfected RAW 264.7 cells harboring NF-κB-SEAP reporter construct with expression vector encoding IKKβ or NF-κB p65. The ectopic expression of IKKβ or NF-κB p65, which bypasses TLRs or cytokine receptors, increased SEAP activity as a reporter of NF-κB transcriptional activity (Fig. 6E,F). CGA-JK3 decreased IKKβ vector-elicited NF-κB transcriptional activity (Fig. 6E), but not SEAP activity under the control of NF-κB p65 vector (Fig. 6F). This result excluded the possibility of direct effect of CGA-JK3 on the NF-κB activating pathway that is located downstream from IKKβ.
RAW 264.7 cells were pretreated with CGA-JK3 for 2 h, and stimulated with Pam3CSK4 or LPS for 30–40 min (A) or with LPS (100 ng/ml) for 1 h (B) in the presence of CGA-JK3. (A) Cell extracts were subjected to Western blot analysis (WB) with anti-IκBα or anti-GAPDH antibody. (B) The cells were subjected to confocal fluorescence microscopy, displaying the NF-κB p65-stained with Alexa Fluor 568-labeled antibody as a red color and the nuclei-stained with DAPI as a blue color. (C) RAW 264.7 cells harboring NF-κB-SEAP reporter construct were stimulated with Pam3CSK4 (1 μg/ml) or LPS (100 ng/ml) for 20 h in the presence of CGA-JK3. (D) RAW 264.7 cells harboring NF-κB-SEAP reporter construct were treated with CGA-JK3 for 2–4 h, washed with PBS and recovered in complete media. The cells were then stimulated with LPS for 20 h. RAW 264.7 cells harboring NF-κB-SEAP reporter construct were transfected with expression vector encoding IKKβ (E) or NF-κB p65 (F) in combination with β-galactosidase control vector. The transfected cells were treated with CGA-JK3 for 20 h. SEAP activity, a reporter of NF-κB transcriptional activity, is represented as relative fluorescence units (RFU) (C,D) or RFU after normalizing to the β-galactosidase activity as a reference of transfection efficiency (E,F). Data are mean ± SEM from three independent experiments using the average values of triplicate in each experiment. #P < 0.05 vs. media alone-added group. *P < 0.05 vs. Pam3CSK4- or LPS alone-stimulated group (C) or IKKβ vector alone-transfected group (E).
However, CGA-JK3 showed no inhibition of the c-Jun phosphorylation at the Ser-63 residue in LPS- or CpG ODN-activated RAW 264.7 cells, and the AP-1 transcriptional activity in LPS-activated cells containing AP-1-Luc reporter construct (Supplementary Fig. 4A,B). In addition, CGA-JK3 did not affect the IRF3 phosphorylation at the Ser-396 residue in poly I:C- or LPS-activated RAW 264.7 cells, and the IRF3 transcriptional activity in LPS-activated cells containing IRF3-Luc reporter construct (Supplementary Fig. 4C,D). The results suggested that CGA-JK3 interrupted IKKβ-inducible NF-κκB activation in macrophages, whereas it had no effects on TLR/MyD88-associated AP-1 activation and TLR/TRIF-dependent IRF3 activation.
CGA-JK3 suppressed mRNA and protein levels of TNF-α or IL-1α in LPS-activated macrophages (Fig. 7A and Table 1), which was consistent with the in vivo effects in endotoxemia- or ALF-induced mice (Figs 1E,F and 2E). RAW 264.7 cells were then transfected with TNF-α-Luc reporter construct containing TNF-α promoter region (−1260/+60). CGA-JK3 inhibited LPS-induced promoter activity of TNF-α gene (Fig. 7B). Moreover, CGA-JK3 inhibited NO production and decreased protein levels of iNOS in Pam3CSK4- or LPS-activated RAW 264.7 cells (Fig. 7C,D). CGA-JK3 consistently attenuated mRNA levels of iNOS in LPS-activated RAW 264.7 cells (Fig. 7A), and inhibited promoter activity of iNOS gene in LPS-activated cells containing iNOS (−1592/+183)-Luc reporter construct (Fig. 7E). The results suggested that CGA-JK3 suppressed NF-κB-regulated expression of TNF-α, IL-1α or iNOS gene at the transcription level. However, CGA-JK3 affected neither the mRNA and protein levels of IRF3-target genes encoding IFN-β or IP-10 in LPS-activated macrophages (Fig. 7A and Table 1), nor the promoter activity of IFN-β gene in LPS-activated cells containing IFN-β (−1814/+11)-Luc reporter construct (Fig. 7F).
(A) RAW 264.7 cells were pretreated with CGA-JK3 for 2 h and stimulated with LPS for 4–6 h in the presence of CGA-JK3. Total RNAs were subjected to RT-PCR analysis to determine mRNA levels of TNF-α, IL-1α, iNOS, IFN-β or IP-10 with β-actin as an internal control. Relative intensity of each cytokine normalized to β-actin is also represented as %. RAW 264.7 cells were transfected with each reporter construct of TNF-α (−1260/+60)-Luc (B), iNOS (−1592/+183)-Luc (E) or IFN-β (−1814/+11)-Luc (F) in the combination with Renilla control vector. The transfected cells were stimulated with LPS for 20 h in the presence of CGA-JK3. Cell extracts were subjected to dual-luciferase assay. Firefly luciferase activity, a reporter of the promoter activity of TNF-α, iNOS or IFN-β gene, is represented as relative fold after normalizing to the Renilla activity as a reference of transfection efficiency. RAW 264.7 cells were stimulated with Pam3CSK4 (1 μg/ml) or LPS (100 ng/ml) for 24 h in the presence of CGA-JK3. (C) Aliquots of the culture supernatants were reacted with Griess reagents to determine NO levels with NaNO2 as a standard. (D) Cell extracts were subjected to Western blot analysis (WB) with anti-iNOS or anti-GAPDH antibody. Data are mean ± SEM from three independent experiments using the average values of triplicate in each experiment. #P < 0.05 vs. media alone-added group. *P < 0.05 vs. LPS- or Pam3CSK4 alone-stimulated group.
Discussion
In the current study, CGA-JK3 ameliorated TLRs-associated endotoxemia, polymicrobial sepsis or ALF in vivo. As a molecular mechanism, CGA-JK3 targeted the ATP-binding active site of IKKβ on the basis of evidences showing that it inhibited IKKβ-catalyzed kinase activity in a competitive manner with respect to ATP, and displaced fluorescent ATP probe from the complex with IKKβ.
The pathophysiological importance of IKKβ has been revealed in gene knockout (KO) mice. Classical KO mice lacking IKKβ die at an embryonic stage due to severe liver degeneration, but can be rescued after TNFR inactivation26,27. On the other hand, conditional KO mice with parenchymal hepatocyte-specific deletion of IKKβ, which bypass the embryonic lethality, are attenuated from soluble TNF-α-induced apoptotic injury and ischemia/reperfusion-induced necrotic damage in the liver28,29. Therefore, it is likely that IKKβ has differential roles in the liver during the embryonic development and adult stages.
Caffeic acid derivatives from medicinal plants have numerous anti-inflammatory benefits. In particular, caffeic acid quinate (chlorogenic acid) rescues endotoxemia-induced mice via directly inhibiting IRAK-4-catalyzed kinase activity, and CLP-induced septic mice via decreasing TNF-α or HMGB-1 levels13,14,15. Caffeic acid phenethyl ester (CAPE) ameliorates LPS-induced endotoxemia in rats by correcting the imbalance between pro- and anti-inflammatory cytokines in the blood, and reduces mortality rates of CLP-challenged septic mice12,30. CAPE also protects from LPS/GalN-induced ALF in rats with restored antioxidant defense in the liver31. CAPE has a negative regulatory role in the NF-κB activating pathway, but its molecular target is controversially assigned as either DNA-binding ability of NF-κB or unidentified signal transducer(s) upstream from IκB phosphorylation/degradation32,33,34. In the current study, chlorogenic acid inhibited the kinase activity of rhIRAK-4 but not rhIKKβ in cell-free reactions, whereas CAPE did not affect the kinase activities of both rhIRAK-4 and rhIKKβ (Supplementary Fig. 5A,B), suggesting different molecular targets from CGA-JK3.
In conclusion, CGA-JK3 interrupted IKKβ-inducible NF-κB activation and NF-κB-regulated gene expression in macrophages stimulated with TLR (1/2, 2/6, 4, 5, 7, 9) agonists from Gram-positive/negative bacteria and viruses or with endogenous cytokines (TNF-α, IL-1α, HMGB-1). Thus, IKKβ was a potential molecular target of CGA-JK3 in the amelioration of TLRs-associated redundant inflammatory responses in endotoxemia-, sepsis- or ALF-induced mice. Finally, CGA-JK3 may be more attractable in the treatment of polymicrobes-infected septic disorders than the drug candidates Eritoran and TAK-242 that are limiting to inflammatory responses in Gram-negative bacteria-infected sepsis. CGA-JK3, a small molecule inhibitor of IKKβ in TLRs-associated immune responses, may be beneficial and reduce mortality of sepsis patients in whom inflammation is excessive and itself causes injury but may harm to the patients in immune suppressive stages, since sepsis leads to high morbidity and mortality through a complex pathophysiology including SIRS, compensatory anti-inflammatory response syndrome, and abnormal blood coagulation35,36,37,38. Further study relating to safety and efficacy profiles of CGA-JK3 or other IKKβ inhibitors would be necessary to translate these concepts into clinical application.
Methods
Chemicals and antibodies
CGA-JK3 (>97% purity) was synthesized from caffeic acid by reacting with cyclohexylamine under an amidation condition. rhIKKβ or other protein kinases were purchased from SignalChem (Richimond, Canada), TLR agonists from Invitrogen (Carlsbad, CA, USA), ATP-TNP from Life Technology (Bangalore, India), and IKKtide or myeloid basic protein (MBP) from Millipore (Temecula, CA, USA). Antibodies were purchased from Santa Cruz Biotechnology (Santa Cruz, CA, USA) and Cell Signaling Technology (Danvers, MA, USA). All other materials, including LPS-FITC, were purchased from Sigma-Aldrich (St. Louis, MO, USA).
Sepsis or ALF model in mice
C57BL/6J male mice, aged 6–7 weeks, were purchased from Korea Research Institute of Bioscience and Biotechnology (Cheongju, Korea), and kept under well-controlled conditions of temperature (22 ± 2 °C), humidity (55 ± 5%) and a 12 h/12 h light-dark cycle with access to food and water ad libitum. The protocol was approved by the Animal Experimentation Ethics Committee in Chungbuk National University (permit number CBNUA-809–15–01), and conducted in accordance with the Korean Ministry of Food and Drug Safety Guide for the Care and Use of Laboratory Animals. C57BL/6J mice were challenged with LPS (40 mg/kg, i.p.) for endotoxemia, CLP for polymicrobial sepsis, or LPS (10 μg/kg, i.p.)/GalN (500 mg/kg, i.p.) for ALF, and treated with CGA-JK3 (i.v.) at 1 h after each challenge. Survival rates were examined as primary outcome. Blood samples were collected to analyze systemic levels of AST, bilirubin or cytokines. Hepatic lobules were fixed in 10% formalin and embedded in paraffin. Serial sections (3 μm thick) of the specimens were stained with hematoxylin and eosin for histological examination, and hepatic injury index was scored as normal = 1, mild = 2, moderate = 3, and severe = 4.
Western blot analysis
Cell extracts were resolved on SDS-acrylamide gels by electrophoresis and transferred to polyvinylidene difluoride membranes. Blocking was with either 5% non-fat milk in PBS containing Tween 20 or 5% BSA in TBS containing Tween 20. The blots were incubated with primary antibody at 4 °C overnight followed by the appropriate horseradish peroxidase-labeled secondary antibody at room temperature for 3–5 h. The immune complex was visualized after reacting with an enhanced chemiluminescence kit (GE Healthcare, Chalfont St. Giles, UK).
RT-PCR analysis
Total RNAs were subjected to RT-PCR with an RNA PCR kit (Bioneer, Daejeon, Korea) in the determination of mRNA levels of TNF-α, IL-1α, IFN-β, iNOS or IP-10. Nucleotide sequences of the PCR primers were previously described15. In brief, total RNAs were reversely transcribed at 42 °C for 1 h and then subjected to 25–30 cycles of PCR. Cycling conditions were 30-s denaturation at 94 °C, 60-s annealing at 50–60 °C and 90-s extension at 72 °C. The RT-PCR products were resolved on agarose gels by electrophoresis and stained with ethidium bromide.
Cell culture
RAW 264.7 cells were purchased from ATCC (Manassas, VA, USA), and peritoneal macrophages were isolated from C57BL/6J mice. In brief, mice were anesthetized with diethyl ether inhalation and the abdominal area was disinfected with 70% ethyl alcohol. Peritoneal cavities of the mice were flushed with ice-cold PBS to harvest macrophages. RAW 264.7 cells or peritoneal macrophages were cultured in Dulbecco’s modified Eagle’s medium supplemented with 10% fetal bovine serum, benzylpenicillin (143 U/ml) and streptomycin (100 μg/ml) under an atmosphere of 37 °C and 5% CO2.
Flow cytometry
Cells were incubated with LPS-FITC (500 ng/ml) for 30 min. Flow cytometric analysis was then conducted using FACSCalibur (BD Bioscience, San Jose, CA, USA).
Cell viability assay
Cells were reacted with 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT, 50 μg/ml) for 2–4 h. Formazan crystals were dissolved in 50% dimethyl sulfoxide and absorbance was measured at 540 nm.
Protein kinase assay
Catalytically active rhIKKβ or other protein kinases were reacted with IKKtide (1 mg/ml) or MBP (0.33 mg/ml) as exogenous substrate in the presence of [γ-32P]ATP (5 μCi) probe at 30 °C for 30 min. Aliquots of the reaction mixtures were spotted onto P81 phosphocellulose, and washed three times with 0.75% H3PO4 followed by once with 100% acetone. Radioactivity was measured as count per min (cpm). Lineweaver-Burk plots were used to estimate kinetic parameters, including Km and Vmax, of rhIKKβ-catalyzed kinase activity.
Fluorescence analysis
ATP-TNP (3 μM) was incubated with rhIKKβ or other protein kinases for 2 h. Fluorescence values were measured as relative fluorescence units (RFU) under excitation at 400 nm and emission at 500–610 nm.
Molecular docking
Crystallographic structure of human IKKβ was obtained from the Protein Data Bank (PDB code 3RZF). Chemical structure of CGA-JK3 was drawn with the Sybyl package and minimized with Tripos force field and Gasteiger-Huckel charge. Docking arrangement of CGA-JK3 onto the crystal structure of IKKβ was carried out with the Surflex-Dock program in Sybyl version 8.1.1 (Tripos Associates, St. Louis, MO, USA).
Confocal microscopy
Cells were fixed in 4% p-formaldehyde, permeabilized in 0.5% Triton X-100 and then blocked in 1% BSA. The cells were reacted with anti-NF-κB p65 antibody followed by Alexa Fluor 568-labeled secondary antibody for immunostaining, incubated with 4,6-diamidino-2-phenylindole (DAPI, 3 μM) for nuclei staining, and then examined under confocal fluorescence microscopy.
SEAP reporter assay
RAW 264.7 cells harboring NF-κB-SEAP reporter construct were used in the determination of NF-κB transcriptional activity15,39. Aliquots of the culture supernatants were heated at 65 °C for 5 min and then reacted with 4-methylumbelliferyl phosphate (500 μM) in the dark. SEAP activity was measured as RFU under excitation at 360 nm and emission at 450 nm.
Luciferase reporter assay
Luciferase reporter constructs of AP-1-Luc or GAS/ISRE-Luc were used in the determination of transcriptional activity of AP-1 or IRF3 (Promega, Madison, WI, USA), and those of TNF-α (−1260/+60)-Luc, iNOS (−1592/+183)-Luc or IFN-β (−1814/+11)-Luc for the promoter activity of TNF-α, iNOS or IFN-β gene40,41. Cells were transfected with each reporter construct in combination with Renilla control vector using a lipofectamine kit (Invitrogen, Carlsbad, CA, USA). Cell extracts were subjected to dual-luciferase assay (Promega, Madison, WI, USA). Firefly luciferase activity as the reporter was normalized to Renilla activity as a reference for transfection efficiency.
NO quantification
Supernatants from macrophage cultures were reacted with Griess reagents (0.1% sulfanilamide and 0.1% N-(1-naphthyl)ethylenediamine in 5% H3PO4), and absorbance was measured at 540 nm with NaNO2 as a standard.
Statistical analysis
Results were expressed as mean ± SEM from at least three independent experiments. Data were statistically analyzed using Dunnett’s test in the ANOVA. Values of P < 0.05 were considered significant.
Additional Information
How to cite this article: Choi, J. H. et al. Caffeic Acid Cyclohexylamide Rescues Lethal Inflammation in Septic Mice through Inhibition of IκB Kinase in Innate Immune Process. Sci. Rep. 7, 41180; doi: 10.1038/srep41180 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Singer, M. et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA 315, 801–810, doi: 10.1001/jama.2016.0287 (2016).
Opal, S. M. et al. Effect of eritoran, an antagonist of MD2-TLR4, on mortality in patients with severe sepsis: the ACCESS randomized trial. JAMA 309, 1154–1162, doi: 10.1001/jama.2013.2194 (2013).
Rice, T. W. et al. A randomized, double-blind, placebo-controlled trial of TAK-242 for the treatment of severe sepsis. Crit Care Med 38, 1685–1694, doi: 10.1097/CCM.0b013e3181e7c5c9 (2010).
Tse, M. T. Trial watch: sepsis study failure highlights need for trial design rethink. Nat Rev Drug Discov 12, 334, doi: 10.1038/nrd4016 (2013).
Mullarkey, M. et al. Inhibition of endotoxin response by e5564, a novel Toll-like receptor 4-directed endotoxin antagonist. J Pharmacol Exp Ther 304, 1093–1102, doi: 10.1124/jpet.102.044487 (2003).
Takashima, K. et al. Analysis of binding site for the novel small-molecule TLR4 signal transduction inhibitor TAK-242 and its therapeutic effect on mouse sepsis model. Br J Pharmacol 157, 1250–1262, doi: 10.1111/j.1476-5381.2009.00297.x (2009).
Kenny, E. F. & O’Neill, L. A. Signalling adaptors used by Toll-like receptors: an update. Cytokine 43, 342–349, doi: 10.1016/j.cyto.2008.07.010 (2008).
Flannery, S. & Bowie, A. G. The interleukin-1 receptor-associated kinases: critical regulators of innate immune signalling. Biochem Pharmacol 80, 1981–1991, doi: 10.1016/j.bcp.2010.06.020 (2010).
Landstrom, M. The TAK1-TRAF6 signalling pathway. Int J Biochem Cell Biol 42, 585–589, doi: 10.1016/j.biocel.2009.12.023 (2010).
Napetschnig, J. & Wu, H. Molecular basis of NF-kB signaling. Annu Rev Biophys 42, 443–468, doi: 10.1146/annurev-biophys-083012-130338 (2013).
Hyun, J., Kanagavelu, S. & Fukata, M. A unique host defense pathway: TRIF mediates both antiviral and antibacterial immune responses. Microbes Infect 15, 1–10, doi: 10.1016/j.micinf.2012.10.011 (2013).
Tekin, A. et al. Effects of caffeic acid phenethyl ester (CAPE) on sepsis in rats. Inflammation 31, 273–280, doi: 10.1007/s10753-008-9075-1 (2008).
Lee, C. H., Yoon, S. J. & Lee, S. M. Chlorogenic acid attenuates high mobility group box 1 (HMGB1) and enhances host defense mechanisms in murine sepsis. Mol Med 18, 1437–1448, doi: 10.2119/molmed.2012.00279 (2012).
Park, S. H. et al. Inhibition of IRAK-4 activity for rescuing endotoxin LPS-induced septic mortality in mice by lonicerae flos extract. Biochem Biophys Res Commun 442, 183–188, doi: 10.1016/j.bbrc.2013.11.045 (2013).
Park, S. H. et al. IRAK4 as a molecular target in the amelioration of innate immunity-related endotoxic shock and acute liver injury by chlorogenic acid. J Immunol 194, 1122–1130, doi: 10.4049/jimmunol.1402101 (2015).
Mignon, A. et al. LPS challenge in D-galactosamine-sensitized mice accounts for caspase-dependent fulminant hepatitis, not for septic shock. Am J Respir Crit Care Med 159, 1308–1315, doi: 10.1164/ajrccm.159.4.9712012 (1999).
Wu, Z., Han, M., Chen, T., Yan, W. & Ning, Q. Acute liver failure: mechanisms of immune-mediated liver injury. Liver Int 30, 782–794, doi: 10.1111/j.1478-3231.2010.02262.x (2010).
Loguercio, C. & Festi, D. Silybin and the liver: from basic research to clinical practice. World J Gastroenterol 17, 2288–2301, doi: 10.3748/wjg.v17.i18.2288 (2011).
Buss, H. et al. Constitutive and interleukin-1-inducible phosphorylation of p65 NF-kB at serine 536 is mediated by multiple protein kinases including IkB kinase (IKK)-a, IKKb, IKKe, TRAF family member-associated (TANK)-binding kinase 1 (TBK1), and an unknown kinase and couples p65 to TATA-binding protein-associated factor II31-mediated interleukin-8 transcription. J Biol Chem 279, 55633–55643, doi: 10.1074/jbc.M409825200 (2004).
Chen, W. et al. Contribution of Ser386 and Ser396 to activation of interferon regulatory factor 3. J Mol Biol 379, 251–260, doi: 10.1016/j.jmb.2008.03.050 (2008).
Weber, C. K., Liptay, S., Wirth, T., Adler, G. & Schmid, R. M. Suppression of NF-kB activity by sulfasalazine is mediated by direct inhibition of IkB kinases a and b. Gastroenterology 119, 1209–1218 (2000).
Burke, J. R. et al. BMS-345541 is a highly selective inhibitor of IkB kinase that binds at an allosteric site of the enzyme and blocks NF-kB-dependent transcription in mice. J Biol Chem 278, 1450–1456, doi: 10.1074/jbc.M209677200 (2003).
Bennett, B. L. et al. SP600125, an anthrapyrazolone inhibitor of Jun N-terminal kinase. Proc Natl Acad Sci USA 98, 13681–13686, doi: 10.1073/pnas.251194298 (2001).
Reilly, S. M. et al. An inhibitor of the protein kinases TBK1 and IKK-e improves obesity-related metabolic dysfunctions in mice. Nat Med 19, 313–321, doi: 10.1038/nm.3082 (2013).
Xu, G. et al. Crystal structure of inhibitor of kB kinase b. Nature 472, 325–330, doi: 10.1038/nature09853 (2011).
Li, Q., Van Antwerp, D., Mercurio, F., Lee, K. F. & Verma, I. M. Severe liver degeneration in mice lacking the IkB kinase 2 gene. Science 284, 321–325 (1999).
Tanaka, M. et al. Embryonic lethality, liver degeneration, and impaired NF-kB activation in IKK-b-deficient mice. Immunity 10, 421–429 (1999).
Maeda, S. et al. IKKb is required for prevention of apoptosis mediated by cell-bound but not by circulating TNFa. Immunity 19, 725–737 (2003).
Luedde, T. et al. Deletion of IKK2 in hepatocytes does not sensitize these cells to TNF-induced apoptosis but protects from ischemia/reperfusion injury. J Clin Invest 115, 849–859, doi: 10.1172/jci23493 (2005).
Korish, A. A. & Arafa, M. M. Propolis derivatives inhibit the systemic inflammatory response and protect hepatic and neuronal cells in acute septic shock. Braz J Infect Dis 15, 332–338 (2011).
Korish, A. A. Effect of caffeic acid phenethyl ester on the hemostatic alterations associated with toxic-induced acute liver failure. Blood Coagul Fibrinolysis 21, 158–163, doi: 10.1097/MBC.0b013e32833678be (2010).
Natarajan, K., Singh, S., Burke, T. R. Jr., Grunberger, D. & Aggarwal, B. B. Caffeic acid phenethyl ester is a potent and specific inhibitor of activation of nuclear transcription factor NF-kB. Proc Natl Acad Sci USA 93, 9090–9095 (1996).
Mapesa, J. O. et al. Catechols in caffeic acid phenethyl ester are essential for inhibition of TNF-mediated IP-10 expression through NF-kB-dependent but HO-1- and p38-independent mechanisms in mouse intestinal epithelial cells. Mol Nutr Food Res 55, 1850–1861, doi: 10.1002/mnfr.201100105 (2011).
Zhao, W. X. et al. Caffeic acid phenethyl ester attenuates pro-inflammatory and fibrogenic phenotypes of LPS-stimulated hepatic stellate cells through the inhibition of NF-kB signaling. Int J Mol Med 33, 687–694, doi: 10.3892/ijmm.2013.1613 (2014).
Delano, M. J. & Ward, P. A. The immune system’s role in sepsis progression, resolution, and long-term outcome. Immunol Rev 274, 330–353, doi: 10.1111/imr.12499 (2016).
Lehmann, C. et al. Novel approaches to the development of anti-sepsis drugs. Expert Opin Drug Discov 9, 523–531, doi: 10.1517/17460441.2014.905538 (2014).
Mansur, A. et al. The regulatory toll-like receptor 4 genetic polymorphism rs11536889 is associated with renal, coagulation and hepatic organ failure in sepsis patients. J Transl Med 12, 177, doi: 10.1186/1479-5876-12-177 (2014).
Mansur, A. et al. The CD14 rs2569190 TT genotype is associated with an improved 30-day survival in patients with sepsis: a prospective observational cohort study. PLoS One 10, e0127761, doi: 10.1371/journal.pone.0127761 (2015).
Moon, K. Y., Hahn, B. S., Lee, J. & Kim, Y. S. A cell-based assay system for monitoring NF-kB activity in human HaCat transfectant cells. Anal Biochem 292, 17–21, doi: 10.1006/abio.2001.5059 (2001).
Yao, J., Mackman, N., Edgington, T. S. & Fan, S. T. Lipopolysaccharide induction of the tumor necrosis factor-a promoter in human monocytic cells: regulation by Egr-1, c-Jun, and NF-kB transcription factors. J Biol Chem 272, 17795–17801 (1997).
Lowenstein, C. J. et al. Macrophage nitric oxide synthase gene: two upstream regions mediate induction by interferon g and lipopolysaccharide. Proc Natl Acad Sci USA 90, 9730–9734 (1993).
Acknowledgements
This study was financially supported by the grant 2015R1D1A1A01057043 or the MRC program 2008–0062275 from the National Research Foundation of Korea, and the foresting project of Osong academy-industry convergence from the Korea Ministry of Trade, Industry & Energy. We thank Dr. Peter F. Johnson (National Cancer Institute, USA) for kind supply of TNF-α-Luc construct, Dr. Kwang Youl Lee (Chonnam National University, Korea) for IFN-β-Luc construct, Dr. William J. Murphy (The Johns Hopkins University School of Medicine, USA) for iNOS-Luc construct, and Dr. Nam Song Choi (Huons Pharmaceutical Co., Korea) for TAK-242.
Author information
Authors and Affiliations
Contributions
J.H.C., J.-K.J., S.-B.H. and Y.K. contributed to the design of this study; J.H.C., S.H.P., W.-J.C., C.-Y.Y., Y.P.C., J.H.Y. and J.T.H. to the acquisition of data; J.H.C., S.H.P., B.A., H.L. and Y.K. to the analysis and interpretation of data; J.H.C., J.-K.J. and Y.K. to the manuscript drafting. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Choi, J., Park, S., Jung, JK. et al. Caffeic Acid Cyclohexylamide Rescues Lethal Inflammation in Septic Mice through Inhibition of IκB Kinase in Innate Immune Process. Sci Rep 7, 41180 (2017). https://doi.org/10.1038/srep41180
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep41180