Abstract
Periodontitis is characterized by inflammation associated with the colonization of different oral pathogens. We here aimed to investigate how bacteria and host cells shape their environment in order to limit inflammation and tissue damage in the presence of the pathogen. Human dental follicle stem cells (hDFSCs) were co-cultured with gram-negative P. intermedia and T. forsythia and were quantified for adherence and internalization as well as migration and interleukin secretion. To delineate hDFSC-specific effects, gingival epithelial cells (Ca9-22) were used as controls. Direct effects of hDFSCs on neutrophils (PMN) after interaction with bacteria were analyzed via chemotactic attraction, phagocytic activity and NET formation. We show that P. intermedia and T. forsythia adhere to and internalize into hDFSCs. This infection decreased the migratory capacity of the hDFSCs by 50%, did not disturb hDFSC differentiation potential and provoked an increase in IL-6 and IL-8 secretion while leaving IL-10 levels unaltered. These environmental modulations correlated with reduced PMN chemotaxis, phagocytic activity and NET formation. Our results suggest that P. intermedia and T. forsythia infected hDFSCs maintain their stem cell functionality, reduce PMN-induced tissue and bone degradation via suppression of PMN-activity, and at the same time allow for the survival of the oral pathogens.
Similar content being viewed by others
Introduction
The oral microbiome contains hundreds of different species forming complex multi-species biofilms1,2. The existence of some species and composition of such biofilms are potential indicators to distinguish between health and disease2,3,4,5. Especially a shift of species to gram-negative anaerobic bacteria, e.g. Aggregatibacter actinomycetemcommitans, Fusobacterium nucleatum, Porphyromonas gingivalis, Prevotella intermedia and Tannerella forsythia, is associated with progressive periodontitis6,7,8,9. Periodontitis is an inflammatory disease of the periodontium induced by bacteria and is characterized by progressive irreversible loss of supportive tissue and finally tooth loss. The oxygen level is decreased in periodontal pockets allowing those anaerobic species to colonize10,11 and disrupt host cell homeostasis12. With increasing access to deeper tissues, periodontal pathogenic bacteria get in contact with various local cell types beside epithelial cells, including different progenitor cells. In vitro studies documented increasing migration of mesenchymal stem cells under hypoxic conditions13. Furthermore, bacterial LPS ambivalently affects human dental pulp stem cell migration, enhancing at 1μg/ml, inhibiting at 10μg/ml14. P. gingivalis LPS inhibits periodontal ligament stem cell osteoblastic differentiation15. Nonetheless, bacterial infection with viable microorganisms presumably has diverse effects on host cells.
As part of tissue repair mechanisms, investigation on stem cell-bacteria interaction is important for better understanding of periodontal disease progression. The direct interaction between bacteria and host cells stimulates immune response in terms of secretion of a wide range of cytokines16,17,18,19. A major recruiting factor for phagocytic polymorphonuclear leukocytes (PMNs) is interleukin-8 which provokes PMN accumulation20,21, further tissue damage and progression of periodontitis22. Human mesenchymal stem cells and gingival epithelial cells were shown to secrete IL-8 after infection with F. nucleatum and P. gingivalis in vitro23. Additionally, Prevotella intermedia LPS provokes IL-8 secretion in human dental pulp fibroblasts24 and interacts with KB cells25, a HeLa derived cell line. Interaction of T. forsythia with Ca9-22 or KB cells was also previously investigated26.
Taken together it can be hypothesized that host cells, including progenitor stem cells, pathogenic bacteria and primary defense cells like PMNs, engage in interactions in the periodontal pocket. The nature of this interplay could determine periodontitis disease outcome. Therefore, the aim of this study was to analyze how oral pathogenic bacteria influence oral stem cells and oral epithelial cells in vitro with a focus on effects they might execute towards PMNs. Our experimental setup was designed to achieve a deeper insight in immunological mechanisms in this complex infection model. In this study, the interaction between periodontal pathogens and human dental follicle stem cells (hDFSCs) was investigated. To understand the specific role of these stem cells, results were compared to the gingival epithelial cell line (Ca9-22). As stem cells have immunomodulatory and tissue regenerating function27, we aimed to demonstrate the effects hDFSCs primed by initial bacterial pathogen contact have on PMNs, which represent a major factor in periodontal inflammation and tissue destruction.
P. intermedia and T. forsythia were chosen for infection as only little is known about those species compared to the well-studied species P. gingivalis, A. actinomycetemcommitans and F. nucleatum. Both species are tightly associated with periodontal disease28,29, although underrepresented in the current literature.
Results
Anaerobic cultivation of hDFSCs
Survival of hDFSCs under anaerobic conditions was observed over 72 h via trypan blue staining, metabolic activity using MTS and expression of stem cell marker.
Under anoxic conditions cell count is reduced to 75% after 24 h, 60% after 48 h and 30% after 72 h compared to aerobic cultivated cells. Thereby, the metabolic activity is reduced. After standardization to the diminished cell count metabolic activity is comparable to aerobic cultivated hDFSCs (see Supplementary Fig. S1). Expression of CD73, CD29, CD90, CD105 and CD44 (CD45-negative) was stable over 72 h of anaerobic incubation (Fig. 1, see Supplementary Tab. S1 for median fluorescence intensity data).
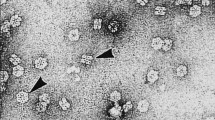
Oral bacteria invade hDFSCs
Adherence and internalization are major steps in host invasion and pathogenesis. The direct interaction between undifferentiated hDFSCs and oral species was examined in terms of adherence and internalization after 2 h of anaerobic co-culture. The differentiated gingival epithelial cell line Ca9-22 was used as control (MOI = 100).
As shown in Fig. 2, P. intermedia adheres equally well to hDFSCs and Ca9-22 cells (about 1% of the inoculum). However, the percentage of P. intermedia internalized into hDFSCs is higher compared to values of the P. intermedia-Ca9-22 interaction. T. forsythia has a distinct phenotype in this assay. Adherence to hDFSCs is more pronounced compared to Ca9-22 cells, whereas internalization into Ca9-22 was significantly higher for T. forsythia. Together, these data show that both species are able to adhere and internalize into hDFSCs as well as Ca9-22 with distinct phenotypes (Fig. 2).
Direct interaction of P. intermedia and T. forsythia with human cells.
HDFSCs and Ca9-22 were infected with P. intermedia or T. forsythia under anaerobic conditions for 2 h. Adherent and internalized bacteria were quantified. Adherent bacteria were related to reference bacteria present in the inoculum, and internalized bacteria were related to adherent bacteria. Results are displayed as median ± interquartile range, *p < 0.05, **p < 0.01 (Mann-Whitney U test), n ≥ 4.
Bacterial infection had neither impact on stem cell marker surface expression nor the differentiation potential
Among others, characteristics of stem cells are the expression of typical stem cell surface markers and the potential to differentiate into various cell lineages depending on stimulus. Thus, it was mandatory to investigate alterations in surface marker display and differentiation under the infection situation described in the previous result section.
In summary, after infection of hDFSCs with P. intermedia or T. forsythia (MOI = 100) no alternation in stem cell surface marker expression (positive for CD73, CD29, CD90, CD105 and CD44; negative for CD45) under anaerobic atmosphere and differentiation potential to adipogenic, chondrogenic and osteogenic fate was detected compared to uninfected cells (Fig. 3, see Supplementary Tab. S2 for median fluorescence intensity data of infected hDFSCs).
Bacterial infection and anaerobic condition reduce hDFSC migration
The migration ability of adherent cells is important in the context of tissue repair and cell repopulation during wound healing30,31. It was shown, that LPS and hypoxia alter migration of stem cells in vitro13,14,32. Consequently, migration activity of hDFSCs was quantified under aerobic and anaerobic conditions with or without bacterial infection (MOI = 100). This phenotype was monitored every 4 h post-infection up to 24 h post infection of co-culture in 24 well plates.
Under aerobic conditions hDFSCs efficiently migrate to completely heal the scratch. An anaerobic atmosphere reduces this capacity by 50%. Under aerobic conditions infection of hDFSCs with both P. intermedia and T. forsythia leads to similarly reduced migration capacities. Infection with T. forsythia under oxygen limitation further impaired cellular migration capacity, however, not reaching significance levels (Fig. 4). Of note, an expected additive effect of infection and anaerobic stress concerning migration of hDFSCs was not observed. The migration of hDFSCs is reduced after anoxic stress and infection. P. intermedia and T. forsythia infection of hDFSCs suppress migration and thus scratch healing. This effect is more significant compared to anaerobic conditions.
Migration of hDFSCs after 24 h.
HDFSCs were incubated under aerobic or anaerobic conditions and in parallel infected with P. intermedia or T. forsythia. Uninfected hDFSCs were used as control. Migration was analyzed in a scratch assay, while the scratch diameter was measured each 4 h up to 24 h. The initial scratch diameter was defined as 100%. The migration dynamic of infected and uninfected hDFSCs is observed over 24 h, results are displayed as median ± standard deviation (A) and final results are presented after 24 h of incubation. Results are displayed as median ± interquartile range, *p < 0.05 (Mann-Whitney U test), n = 4 (B). Representative microscopic photograph of the migrating HDFSCs after 24 h of aerobic (C) and anaerobic (D) incubation.
Bacterial infection induces interleukin secretion by hDFSCs
As response to bacterial infection human cells are able to secrete a wide range of cytokines with pro- and/or anti-inflammatory effects to influence their environment. Thus, after infection of hDFSCs or Ca9-22 with P. intermedia or T. forsythia accumulation of interleukins IL-6, IL-8 and IL-10 in the supernatant was quantified after 2 h, 4 h and 24 h of anaerobic co-culture (MOI = 100).
Infection of hDFSCs with P. intermedia or T. forsythia results in increasing IL-6 concentration in the supernatant after 24 h. In contrast, the gingival epithelial cell line Ca9-22 does not respond to P. intermedia or T. forsythia infection with increased IL-6 secretion emphasizing the unexpected and obviously specific phenotype of the infection-responsive undifferentiated hDFSCs. (Fig. 5A).
Secretion of IL-6, IL-8 and IL-10 after infection of human cells.
HDFSCs and Ca9-22 were infected with P. intermedia or T. forsythia under anaerobic conditions. IL-6 (A), IL-8 (B) and IL-10 (C) levels were quantified via ELISA after 2 h, 4 h and 24 h from the supernatant of infected cells with P. intermedia (left) and T. forsythia (right). Values from uninfected hDFSC controls matching the experimental time points were subtracted beforehand. Results are displayed as median ± interquartile range, *p < 0.05 (Mann-Whitney U test), n = 4.
A significant accumulation of IL-8 by infected hDFSCs after P. intermedia and T. forsythia infection was exclusively detected after 24 h. P. intermedia infected hDFSCs show a highly significant increase compared to infected Ca9-22 cells, which are rather unresponsive in terms of IL-8 secretion. The Ca9-22 cell response to T. forsythia infection is comparable to hDFSCs with only a marginally significant difference 2 h post-infection (Fig. 5B).
No time-dependent accumulation of anti-inflammatory IL-10 was detected for either cell type infected with P. intermedia or T. forsythia. Of note, the general levels of accumulated IL-10 in infected hDFSCs are higher, reaching significance for almost all measurement time points. In general, hDFSCs are more responsive towards infection with P. intermedia or T. forsythia (Fig. 5C).
Together, P. intermedia and T. forsythia are capable of provoking hDFSCs to secrete inflammatory cytokines like IL-6 and IL-8 in similar or higher concentrations compared to gingival epithelial cells. However, this pro-inflammatory response appears to be counterbalanced by constant IL-10 level.
Infected hDFSCs can reduce chemotaxis of PMN
Cytokines, e.g. interleukins, are secreted by cells to influence their direct environment. PMNs are recruited to infection sites following a chemical gradient of especially IL-8, which can be produced by hDFSCs, as shown in the previous section. The attraction potential of P. intermedia and T. forsythia after infection of hDFSCs was addressed in a transwell migration assay. To this end, migration of PMN towards sterile filtered supernatants of hDFSCs and/or bacteria was quantified after 2 h of aerobic incubation in cell culture medium.
To evaluate the different culture influences, PMN migration towards untreated hDFSCs is determined and set to 100%. The bacterial culture supernatant of P. intermedia leads to high level attraction and migration of PMNs (209.1%). Presence of hDFSCs in the initial interaction with P. intermedia leads to an almost abolished PMN chemotaxis (6.8%), which implies a suppressive effect of hDFSCs in co-culture with the microorganism. T. forsythia supernatants alone and after hDFSC infection lead to 50% reduction of PMN movement towards the infection stimulus. Thus, hDFSCs are able to influence the chemotactic attraction potential of bacteria towards PMNs in a species specific manner (Fig. 6).
Chemotactic behavior of PMNs towards infected hDFSCs.
Migration of PMNs was assessed via transwell assay. After 24 h sterile filtered supernatants of P. intermedia and T. forsythia in cell culture medium with/without hDFSCs were used as chemo attractants in the lower wells. PMNs in fresh cell culture medium without serum were added to the insert. After 2 h of aerobic incubation the count of PMNs migrated into the lower compartment was determined. Migration of PMNs in the presence of non-infected hDFSCs was set to 100% (dashed line). Results are displayed with median ± interquartile range. *p < 0.05, **p < 0.01 (Mann-Whitney U test), n ≥ 4.
Infected hDFSCs reduce phagocytic activity of PMNs
As hDFSCs secrete several cytokines and influence PMN chemotaxis, the influence on phagocytosis, an important component of the innate immune response of PMNs, was next characterized.
The phagocytic activity of PMNs was determined by quantification of bacteria in the supernatant after 2 h of incubation in presence and absence of hDFSCs. To prevent bacteria from internalization into hDFSCs, the cytoskeleton inhibitor of actin polymerization Latrunculin was added to hDFSCs. The inhibitor was removed prior to bacterial infection in order to allow undisturbed PMN activity at later stages of the experiment. This treatment completely abolished bacterial internalization (data not shown). After 2 h of anaerobic incubation with PMNs bacterial counts were assessed.
First, the number of bacteria used for infection was considered the maximum number that could be cleared and was therefore considered a 100% clearance. Accordingly, within two hours, PMNs eliminated 75.5% of inoculated P. intermedia and 71.3% of T. forsythia. Presence of hDFSCs led to a significantly reduced bacterial clearance efficiency of the PMNs (15.5% clearance of P. intermedia, 22.5% clearance of T. forsythia). Inhibition of bacterial internalization into hDFSCs results in moderate but still significant reduction of clearance (47.2% clearance of P. intermedia, 51.4% clearance of T. forsythia). Thereby, the protective effect of hDFSCs against PMN induced bacterial clearance has two distinguishable levels. First, a direct influence of hDFSCs on PMN activity, and second, internalization of bacteria into hDFSCs further reduce the number of available bacterial for PMN mediated clearance (Fig. 7).
Phagocytic activity of PMNs against oral bacteria.
Phagocytic activity is shown as bacterial clearance from the supernatant of P. intermedia or T. forsythia with hDFSCs relative to the control of bacteria only. Results are displayed with median ± interquartile range. **p < 0.01, ***p < 0.001 (Mann-Whitney U test), n ≥ 4.
Infected hDFSCs reduce NET formation of PMN
Another important feature of PMN defense is the formation of neutrophil extracellular traps in response to harmful signals. PMNs were stimulated with supernatants of infected hDFSCs, bacteria or cells for 180 min, and NET formation was quantified with respect to extracellular DNA content. As positive control PMNs were stimulated with glucose oxidase.
Extracellular DNA content of PMNs challenged with hDFSCs in cell culture medium is set to 100%. Bacterial presence increases DNA release further. Nevertheless, the stimulus is higher using bacteria without stem cells (143.0% for P. intermedia, 186.1% for T. forsythia). Under glucose oxidase stimulation of PMN maximum NET formation was observed in the supernatant. In consequence, hDFSCs apparently reduce NET formation of PMNs after bacterial infection (Fig. 8).
NET formation of PMNs against oral bacteria.
NETs were quantified via quantification of extracellular DNA. HDFSCs and P. intermedia or T. forsythia were used as stimuli for PMNs. After 180 min, extracellular DNA was quantified and uninfected hDFSCs were set to 100%. Results are displayed with median ± interquartile range. *p < 0.05 (Mann-Whitney U test) significance to hDFSC control, n = 4.
Discussion
The major focus of this study was to investigate the trilateral interaction of periodontopathogenic bacteria, dental stem cells and PMN activity. This constellation occurs during active periodontitis in patients, and thus we aimed to elucidate if in vitro results could at least partially explain clinical phenotypes in periodontitis. This inflammatory disease is characterized by bacterial biofilms in periodontal pockets, a sustained inflammatory reaction as innate immune response to bacterial presence, hyper-immune activation, osteoclast activation, tissue and bone resorption and finally tooth loss.
In this study, we demonstrated different effects of infection of human dental follicle stem cells with either P. intermedia or T. forsythia. With respect to the anaerobic bacterial species, P. intermedia and T. forsythia, and low partial pressure of oxygen in periodontal pockets10,11,30,31, an anaerobic in vitro model described by Kriebel et al.23 was applied. The consequences of anoxic stress towards the dental stem cells (hDFSCs) were analyzed. As previously shown by Kanafi and colleagues migration and proliferation of human dental pulp stem cells (SHEDs and DPSCs) were increased under hypoxic conditions of 2.3% O2 und 5% CO2 compared to normoxic conditions33. Even 3% of oxygen stimulated migration of mesenchymal bone marrow stem cells13,34,35. In the experimental system studied here we show that anoxia lead to significantly lower migration, and no proliferation was observed. The infection of hDFSCs also reduced migration, but had no additive effect on migration. Interestingly, LPS from P. gingivalis was described as a positive stimulus for dental stem cell migration, although no increase in interleukin levels was shown32. Nonetheless, stimulation of cells with bacterial components may differ from an infection with vital bacteria, a note that favors our experimental setup. In co-culture of primary human keratinocytes with P. gingivalis or F. nucleatum a species specific delay in scratch closure was demonstrated in aerobic condition36. Thus, migration activity is influenced by various factors, among them cell type, microbial stimulation modus and culture conditions.
Adherence and internalization are key steps in host infection. For this purpose, various taxa specific adhesion molecules are expressed by oral species37. It was already shown that different oral pathogens, e.g. P. gingivalis, F. nucleatum and A. actinomycetemcommitans, are able to enter different host cell types18,38,39. In our current study, we proved the direct interaction of P. intermedia and T. forsythia with hDFSCs in vitro. Although the adherence of P. intermedia to hDFSCs and gingival epithelial cells was indistinguishable, more bacteria entered the dental stem cells, implying a more efficient cell invasion. In fact, little is known about the specific mechanism, but type A fimbriae are suspected to be of general relevance for P. intermedia internalization40,41. A higher number of T. forsythia was able to adhere to hDFSCs compared to differentiated Ca9-22 cells, although the internalized bacteria related to the adherent beforehand was significantly higher for Ca9-22 cells. A possible explanation could be the specific expression of surface molecule BspA, which mediates cell adhesion and invasion40,41,42,43. Sabet and colleagues described for T. forsythia 2% of adherence to and 0.5% of internalization into KB cells44, which is comparable to our presented results with regard to a differential experimental set up and MOI. Of note, P. gingivalis and F. nucleatum show higher affinity towards epithelial cells compared to hDFSCs underlining a possible divergent survival strategy in host tissue compared to T. forsythia and P. intermedia18. The co-infection with a mixture of different oral species may further influence the affinity towards host cells and should be studied in the future.
When challenged with bacterial infection, host cells secrete immunomodulatory cytokines. We have shown here that both, P. intermedia and T. forsythia, trigger hDFSC IL-6 and IL-8 response, while IL-10 level remain at constant levels throughout the experiment. However, it should be taken into consideration that protease activity can not be excluded and thus influences IL quantification. Guan and colleagues already demonstrated secretion of IL-6 und IL-8 by human periodontal ligament cells after infection with P. intermedia, but no stimulation of IL-1ß and TNF-α19. T. forsythia provoked KB cells to secrete comparable levels of IL-8, but only basal IL-6 levels compared to infected hDFSCs in this study45. The IL-8 concentration in the supernatant was lower for T. forsythia. Proteolytic enzymes, e.g. putative serine proteases, Karipsin and Karilysinn are identified46,47 and might influence chemotactic attraction of immune cells. Remarkably, compared to IL-8 secretion levels by hMSCs infected with Fusobacterium nucleatum23, P. intermedia induced a similar phenotype upon hDFSC infection in our study. HDFSCs infected with P. gingivalis and F. nucleatum are almost unresponsive in terms of IL-8 secretion18, a phenotype diverging from hDFSCs infected with P. intermedia and T. forsythia in this study. This again highlights divergent survival strategies of various oral periodontal pathogens.
Our further results revealed chemotaxis of PMNs towards T. forsythia infected hDFSCs is reduced compared to uninfected cells. Of note, the infection did not promote PMN migration. Low IL-8 levels in the supernatant could be a reason for this reduced attraction. In contrast, P. intermedia showed increased attraction of PMNs in this experiment. Remarkably, P. intermedia infected hDFSCs did not attract immune cells within 2 h post-infection, although IL-8 accumulation was high implying another chemotactic mechanism upon IL-8 response. The constant IL-10 concentration might support this behavior, since it is known to suppress pro-inflammatory cytokine release of PMNs48. Another mechanism or so far unidentified secretory factor can be responsible, too.
The immunomodulation of periodontal stem cells was demonstrated by Cianci et al.49. A specific protective effect of hDFSCs against tissue damage is conceivable and moreover, these effects vary depending on the bacterial species in contact with hDFSCs. Especially remarkable is the reduction of bacterial clearance via PMN killing from the supernatant in the presence of dental stem cells. The bacterial killing by PMNs is more effective in the absence of hDFSCs. Inhibition of direct bacteria-stem cell interaction leads to intermediate clearance. A possible mechanism is the observed bacterial invasion into hDFSCs to evade PMN activity, since the invasion in co-culture without immune cells is negligible compared to the inoculated bacteria. It is known that host defense and PMN activity mediate tissue degradation in periodontitis50, thus our results rather suggest a phenotypical environment with strongly reduced tissue and bone destruction.
Main mediators for bacterial recognition are LPS receptor CD14 and toll like receptors (TLRs), e.g. TLR-2 and TLR-4, which play a critical role in periodontal inflammation51,52,53. An induced reduction of host cell CD14 expression by P. gingivalis is related to reduced phagocytic activity of macrophages against living bacteria54.
The formation of neutrophil extracellular traps was increased upon bacterial challenge compared to infected stem cells, and compared to uninfected hDFSCs. Again, dental stem cells cause a decrease in defense efficiency of PMNs against bacteria.
Generally, PMN activity against oral microorganisms is a complex orchestration of defense strategies, e.g. chemotactic movement to the site of infection, capturing of bacteria in NETs and phagocytic elimination from the environment. HDFSCs apparently protect the oral bacteria against PMN mediated removal, most likely via anti-inflammatory cytokine secretion and internalization of bacteria. Since bacterial survival is increased in the co-culture with local host stem cells, a higher burden of such species is reasonable in periodontal pockets. Otherwise, anti-inflammatory cytokine release prevents against hyperstimulation of PMN and thus aggravated host mediated tissue degradation. This observation with P. intermedia and T. forsythia is contrary to oral species as P. gingivalis, which are known to rapidly increase inflammation55. In summary, decreased PMN activity induced by exploitation of hDFSCs by P. intermedia and T. forsythia could lead to decreases in reactive oxygen species activity and subsequent reduced osteoclast activation, thereby protecting against bone resorption and tooth loss.
Of course, this mono-specific infection is restricted to the in vitro model, as complex oral biofilms consists of hundreds of species. On the other hand, mono-causal effects cannot be drawn back in multi-variant experimental setups, and thus undermine better understanding of species-specific interactions.
Conclusion
Our results pinpoint towards a bacterial species-dependent exploitation of dental stem cells, leading in final consequence to immunomodulatory functions of dental stem cells in bacterially induced periodontal disease. Oral bacteria trigger interleukin response by hDFSCs in in vitro co-culture. In the case of P. intermedia and T. forsythia infected hDFSCs this leads to decreased chemotaxis, phagocytic activity and NET formation of PMNs, implying anti-inflammatory effects of infected dental stem cells. Especially with respect to host tissue damage by activated neutrophils, the role of hDFSCs is a two edged sword, as undermining PMN activity leads to better survival of periodontal pathogenic bacteria, maintaining a constant source of inflammation and immune response. Of note, P. intermedia and T. forsythia infected hDFSCs maintain their stem cell functionality and archetypical differentiation potential, at the same time signaling towards a reduced PMN mediated innate immune response.
Methods
Ethics statements
Ethics approval for all experiments using human materials in this study was granted by the University of Rostock Ethics Committee (https://ethik.med.uni-rostock.de/). All methods using the human stem cells and human blood PMNs were carried out in accordance with all relevant guidelines and regulations and all experimental protocols were approved by the above mentioned Ethics Board.
In detail, human stem cells from the dental follicle (hDFSCs) were isolated from wisdom teeth provided by the Department of Oral and Maxillofacial Plastic Surgery, University of Rostock. Informed consent was obtained from all subjects. Moreover, donors gave their written approval to participate in this study. This procedure was authorized by the ethics committee of the University of Rostock, Germany (Permission No. A 2011 91). Approval for the use and isolation of human polymorphonuclear leukocytes (PMNs) from the blood of healthy volunteers was given by the ethics committee of the University of Rostock, Germany (Permissions No. A 2013 0127 and No. A 2014 0131) and again informed consent was obtained from all subjects.
Anaerobic cultivation of cells and oral microorganisms
Anaerobic cultivation was realized using the miniMACS anaerobic workstation (Don Whitley Scientific, Shipley, UK) with integrated palladium catalyst, temperature and humidity control. Before entering the workstation two nitrogen flushes were performed to eliminate environmental oxygen. Additionally, absence of oxygen was controlled using anaerobic atmosphere indicator strips (Biomérieux, Marcy-l′Étoile, F).
Cell isolation and culture
Isolation of human stem cells from the dental follicle (hDFSCs) was performed as described by Haddouti et al.56 from three young donors with healthy periodontal status. The wisdom teeth were not erupted before extraction to prevent bacterial priming. Cells were cultivated in Dulbecco modified Eagle medium (DMEM F-12, Thermo Fisher Scientific, Waltham, USA) supplemented with 10% fetal calf serum (FCS) and 1% PenStrep (Thermo Fisher Scientific, Waltham, USA) at 37 °C, 5% CO2. For experimental setup cells of passages 8 to 12 were used. Living cell count, metabolic activity and expression of stem cell markers were validated before and after co-cultivation of bacteria under aerobic (37 °C, 5% CO2) and anaerobic conditions (37 °C, 80% N2/10% H2/10% CO2) at time points 24 h, 48 h and 72 h. The living cell count was determined via trypan blue staining in a Neubauer counting chamber. The metabolic activity was quantified following the MTS based assay protocol (CellTiter96 AQueouse One Solution Reagent, Promega, Madison, USA). Positive expression of CD73, CD29, CD90, CD105 and CD44, and negative expression of CD45 was confirmed. For this, incubated cells were trypsinized, centrifuged (300 g, 10 min, 21 °C), washed with PBS and resuspended in FACS buffer (PBS, pH 7.2, 0.2% BSA). Cells were incubated with antibody and isotype control (Biolegend, San Diego, USA) for 30 min at 4 °C, centrifuged (300 g, 10 min, 4 °C), washed with FACS buffer and analyzed in a flow cytometer (Accuri C6, BD Biosciences, Franklin Lakes, USA).
The human gingival epithelial cell line Ca9-22 was provided by the German Cancer Research Center (DKFZ, Heidelberg, G). Cells were cultivated in Dulbecco modified Eagle medium (DMEM + GlutaMax-I, Thermo Fisher Scientific, Waltham, USA) supplemented with 10% FCS and 1% PenStrep at 37 °C and 5% CO2. Cell count and metabolic activity were proved for co-culture conditions as described above.
Human polymorphonuclear leukocytes (PMNs) were isolated from the blood of 8 healthy young volunteers at room temperature. Erythrocytes from heparinized venous blood were lysed by Buffer EL (Qiagen, Venlo, Netherlands), followed by centrifugation (300 g, 10 min, 21 °C) and washing with PBS. Density gradient separation of remaining cells (400 g, 40 min, 21 °C) was performed using Ficoll-Paque PLUS (GE Healthcare Bio-Sciences, Chalfont St Giles, Great Britain). The quality of blood cell separation was assessed via flow cytometry using CD15 antibody (ImmunoTools, Friesoythe, Germany).
Bacterial species
The strains Tannerella forsythia ATCC 43037 and Prevotella intermedia ATCC 25611 were acquired from commercial providers (American Type Culture Collection, Manassas, USA), and cultivated on COL agar plates (BD, Franklin Lakes, USA) and in PYG modified with 5 μg/ml hemin and 1% vitamin K1 under anaerobic atmosphere (37 °C, 80% N2/10% H2/10% CO2). Growth behavior in cell culture medium DMEM with 10% FCS was validated via optical density at 600 nm in parallel with PYG and BHI and parallel CFU determination of BHI probes on BHI agar plates over 24 h under anaerobic conditions.
Co-culture
The co-culture of bacteria and human stem cells was established by Kriebel et al.23. Cells were seeded into well plates without antibiotics and incubated to allow attachment and forming of a 70–80% confluent monolayer at 37 °C, 5% CO2. For each co-culture 105 hDFSCs or Ca9-22 cells/ml were used.
Bacterial species T. forsythia and P. intermedia were grown to stationary phase in PYG modified with 5 μg/ml hemin and 1% vitamin K1 at 37 °C, 80% N2/10% H2/10% CO2. Bacterial count was adjusted to 107 microorganisms/ml in DMEM. Adherent human cells were washed with PBS and infected with oral bacteria at a multiplicity of infection (MOI) of 100 in DMEM.
Freshly isolated PMNs were counted using a Neubauer chamber, adjusted to 106 PMNs/ml in DMEM and added to the previous co-cultures. According to the experimental setup, co-culture is realized under different conditions as described below.
Adherence and internalization
To measure direct interactions of oral bacteria and gingival epithelial cells or hDFSCs, cells were prepared as described in the section co-culture in 24 well plates. Co-culture with the anaerobic bacteria was realized anaerobically (37 °C, 80% N2/10% H2/10% CO2) in DMEM without FCS (MOI = 100). Wells with bacteria mono-culture were used as growth reference.
After 2 h supernatants were removed and cells were washed with PBS. For adherence, human cells were trypsinized, centrifuged (300 g, 10 min, 21 °C), washed with PBS and lysed. Adherent bacteria were counted after plating on COL agar plates. For internalization, fresh medium with 1% PenStrep was added after washing with PBS to kill extracellular adherent bacteria. After a further 2 h incubation period hDFSCs were washed with PBS, trypsinized, centrifuged (300 g, 10 min, 21 °C) and washed with PBS. After cell lysis, internalized bacteria were plated on COL agar.
Stem cell marker and differentiation
HDFSCs were infected with microorganisms. After 24 h of anaerobic co-culture stem cell surface factors (CD29, CD44, CD73, CD90, CD105 and CD45) and corresponding isotype controls were quantified via flow cytometer as described in section Cell isolation and culture (MOI = 100). Uninfected hDFSCs were used as control under aerobic and anaerobic conditions.
To analyze the influence of infection on differentiation potential of the dental stem cells, hDFSCs were seeded into 24 well plates with cover slips and initially infected with P. intermedia or T. forsythia for 2 h. Afterwards cells were washed and treated with 1% PenStrep. Uninfected hDFSCs were used as control. After 24 h of aerobic incubation cells were covered with differentiation medium (adipogenic: 1 μM dexamethasone, 0.2 mM indomethacin, 0.5 mM 3-isobutyl-1-methylxanthine, 2 μM Insulin; osteogenic: 1 μM dexamethasone, 10 mM β-glycerophosphate, 50 μM ascorbic acid 2-phosphate; chondogenic: 50 μM ascorbic acid 2-phosphate, 40 μg/ml proline, 100 μg/ml, sodium pyruvate, ITS) with medium exchange after three to four days. Cells with normal cell culture medium DMEM with 10% FCS were used as negative control, uninfected cells in differentiation medium were used as positive control. After 7, 14 and 21 days, cells were stained and analyzed via microscopy. Adipogenic differentiation experimental probes were stained with Oil Red O solution, chondogenic differentiation was visualized with safranin, and osteogenic fate was examined using von Kossa stain.
Cytokine secretion
HDFSCs and Ca9-22 cells were seeded into 24 well plates and co-cultivated with the anaerobic bacteria in DMEM with 10% FCS (MOI = 100). Uninfected cells served as control. After 2 h, 4 h and 24 h (37 °C, 80% N2/10% H2/10% CO2) supernatants were collected and stored at −20 °C for analysis of IL-6, IL-8 and IL-10 concentrations via OptEIA Human IL ELISA Kits (BD, Franklin Lakes, USA). Performance and calibration were done according to manufacture description. Controls were subtracted from the values determined for infected cells.
Migration
The ability of hDFSCs to migrate was assessed under aerobic and anaerobic conditions (37 °C). Therefore, a wound closure assay described by Laheij et al.57 was modified. Cells were seeded into 24 well plates with cover slips. The adherent cell layer was continuously scratched, medium was exchanged and cells were infected with 107 cfu/ml of each bacteria species (MOI = 100). Each scratch diameter was determined in five representative image sections for three technical replicates per experiment each 4 h up to 24 h from the beginning using the Biozero BZ 8000 (Keyence, Osaka, J) and corresponding Biozero software. Uninfected hDFSCs were used as control.
Chemotaxis
To analyze the chemotactic attraction potential of infected stem cells towards PMNs, the transwell migration assay was modified as described by Nuzzi et al.58. Transwell permeable support plates (3 μm polyester membrane, Corning, Corning, USA) were coated with 2.5 μg/ml fibrinogen for 1 h and dried overnight. Sterile filtered supernatants of HDFSCs infected with oral bacteria for 24 h in DMEM without FCS (37 °C, 80% N2/10% H2/10% CO2) were used as attractants and added to the lower compartment (MOI = 100). Sterile filtered supernatants of hDFSCs or bacterial mono-cultures were used as controls.
106 freshly isolated PMNs were added into the insert. After 2 h of aerobic incubation the number of PMNs in the lower segments was assessed using trypan blue and a Neubauer counting chamber.
Phagocytosis
The phagocytosis assay was adapted from Leijh et al.59. 105 hDFSCs were infected with 107 bacteria in DMEM without FCS (MOI = 100) and 106 freshly isolated PMNs were added. Mono-cultures of bacteria or PMNs were used for control. After 2 h of cultivation (37 °C, 5% CO2) PMNs were counted via trypan blue staining and a Neubauer counting chamber, centrifuged (300 g, 10 min, 21 °C) and lysed to determine extracellular and intracellular bacteria and bacterial clearance by PMNs. For control, stem cells were pre-treated for 1 h with Latrunculin B (10 μM) and washed with fresh medium to prevent direct bacteria-stem cell interaction and thus evasion from PMNs.
NETosis
The formation of NETs was quantified in black 96 well plates after challenging 106 PMNs/ml with 107 microorganisms/ml cultivated with or without 105 hDFSCs/ml (MOI = 100). Control stimulation of PMNs was realized using glucose oxidase (20 mU, from Aspergillus niger, Sigma Aldrich). After 165 min of aerobic incubation extracellular DNA was quantified via adding 30 μl Sytox green (50 μM, Life Technologies, Carlsbad, California) to the samples. After 15 min of incubation (37 °C, 5% CO2) fluorescence was measured at 485/520 nm.
Statistics
All experiments were carried out in at least 4 biological replicates. The results are presented as median ± interquartile range. Statistical analysis for significance was realized with Mann-Whitney U test, and significance was defined as *p < 0.05, **p < 0.01 and ***p < 0.001 using the implemented analysis function of GraphPad Prism 6 software (La Jolla, USA).
Additional Information
How to cite this article: Hieke, C. et al. Human dental stem cells suppress PMN activity after infection with the periodontopathogens Prevotella intermedia and Tannerella forsythia. Sci. Rep. 6, 39096; doi: 10.1038/srep39096 (2016).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Aas, J. A., Paster, B. J., Stokes, L. N., Olsen, I. & Dewhirst, F. E. Defining the normal bacterial flora of the oral cavity. J. Clin Microbiol. 43, 5721–5732, doi: 10.1128/JCM.43.11.5721-5732.2005 (2005).
Dewhirst, F. E. et al. The human oral microbiome. J. Bacteriol. 192, 5002–5017, doi: 10.1128/JB.00542-10 (2010).
Zarco. M. F., Vess, T. J. & Ginsburg, G. S. The oral microbiome in health and disease and the potential impact on personalized dental medicine. Oral Dis. 18, 109–120, doi: 10.1111/j.1601-0825.2011.01851.x (2012).
Wade, W. G. The oral microbiome in health and disease. Pharmacol. Res. 69, 137–143, doi: 10.1016/j.phrs.2012.11.006 (2013).
Duran-Pinedo, A. E. & Frias-Lopez, J. Beyond microbial community composition: functional activities of the oral microbiome in health and disease. Microbes Infect. 17, 505–516, doi: 10.1016/j.micinf.2015.03.014 (2015).
Berezow, A. B. & Darveau, R. P. Microbial shift and periodontitis. Periodontol 2000. 55, 36–47, doi: 10.1111/j.1600-0757.2010.00350.x (2011).
Klein, M. I. & Gonçalves, R. B. Detection of Tannerella forsythensis (Bacteroides forsythus) and porphyromonas gingivalis by polymerase chain reaction in subjects with different periodontal status. J. periodontol. 74, 798–802, doi: 10.1902/jop.2003.74.6.798 (2003).
Yano-Higuchi, K., Takamatsu, N., He, T., Umeda, M. & Ishikawa, I. Prevalence of Bacteroides forsythus, Porphyromonas gingivalis and Actinobacillus actinomycetemcomitans in subgingival microflora of Japanese patients with adult and rapidly progressive periodontitis. J. Clin Periodontol. 27, 597–602, doi: 10.1034/j.1600-051x.2000.027008597.x (2000).
Yang, H., Huang, Y. & Chou, M. Occurrence of Porphyromonas gingivalis and Tannerella forsythensis in periodontally diseased and healthy subjects. J. Periodontol. 75, 1077–1083, doi: 10.1902/jop.2004.75.8.1077 (2004).
Mettraux, G. R., Gusberti, F. A. & Graf, H. Oxygen tension (pO2) in untreated human periodontal pockets. J. Periodontol. 55, 516–521, doi: 10.1902/jop.1984.55.9.516 (1984).
Loesche, W. J., Gusberti, F., Mettraux, G., Higgins, T. & Syed, S. Relationship between oxygen tension and subgingival bacterial flora in untreated human periodontal pockets. Infect Immun. 42, 659–667 (1983).
Darveau, R. P. Periodontitis: a polymicrobial disruption of host homeostasis. Nat Rev Microbiol. 8, 481–490, doi: 10.1038/nrmicro2337 (2010).
Rosová, I., Dao, M., Capoccia, B., Link, D. & Nolta, J. A. Hypoxic preconditioning results in increased motility and improved therapeutic potential of human mesenchymal stem cells. Stem Cells. 26, 2173–2182, doi: 10.1634/stemcells.2007-1104 (2008).
Li, D. et al. The effects of LPS on adhesion and migration of human dental pulp stem cells in vitro. J. Dent. 42, 1327–1334, doi: 10.1016/j.jdent.2014.07.007 (2014).
Kato, H., Taguchi, Y., Tominaga, K., Umeda, M. & Tanaka, A. Porphyromonas gingivalis LPS inhibits osteoblastic differentiation and promotes pro-inflammatory cytokine production in human periodontal ligament stem cells. Arch. Oral Biol 59, 167–17,. doi: 10.1016/j.archoralbio.2013.11.008 (2014).
Han, Y. W. et al. Interactions between Periodontal Bacteria and Human Oral Epithelial Cells: Fusobacterium nucleatum Adheres to and Invades Epithelial Cells. Infect Immun. 68, 3140–3146, doi: 10.1128/IAI.68.6.3140-3146.2000 (2000).
Okada, H. & Murakami, S. Cytokine Expression in Periodontal Health and Disease. Crit Rev Oral Biol Med. 9, 248–266, doi: 10.1177/10454411980090030101 (1998).
Biedermann, A., Kriebel, K., Kreikemeyer, B. & Lang, H. Interactions of anaerobic bacteria with dental stem cells: an in vitro study. PLoS One. 9, e110616, doi: 10.1371/journal.pone.0110616 (2014).
Guan, S., Zhang, M., He, J. & Wu, J. Mitogen-activated protein kinases and phosphatidylinositol 3-kinase are involved in Prevotella intermedia-induced proinflammatory cytokines expression in human periodontal ligament cells. Biochem Biophys Res Commun. 386, 471–476, doi: 10.1016/j.bbrc.2009.06.058 (2009).
Djeu, J. Y., Matsushima, K., Oppenheim, J. J., Shiotsuki, K. & Blanchard, D. K. Functional activation of human neutrophils by recombinant monocyte-derived neutrophil chemotactic factor/IL-8. J. Immun. 144 (6), 2205–2210 (1990).
Huber, A. R., Kunkel, S. L., Todd, R. F. & Weiss, S. J. Regulation of transendothelial neutrophil migration by endogenous interleukin-8. Science. 254, 99–102 (1991).
Graves, D. Cytokines that promote periodontal tissue destruction. J. Periodontol. 79, 1585–1591, doi: 10.1902/jop.2008.080183 (2008).
Kriebel, K., Biedermann, A., Kreikemeyer, B. & Lang, H. Anaerobic co-culture of mesenchymal stem cells and anaerobic pathogens - a new in vitro model system. PLoS One. 8, e78226, doi: 10.1371/journal.pone.0078226 (2013).
Nagaoka, S. et al. Interleukin-8 gene expression by human dental pulp fibroblast in cultures stimulated with Prevotella intermedia lipopolysaccharide. J. Endod. 22, 9–12, doi: 10.1016/S0099-2399(96)80228-7 (1996).
Dorn, B. R., Leung, K. L. & Progulske-Fox, A. Invasion of human oral epithelial cells by Prevotella intermedia. Infect Immun. 66, 6054–6057 (1998).
Sakakibara, J. et al. Loss of adherence ability to human gingival epithelial cells in S-layer protein-deficient mutants of Tannerella forsythensis. Microbiology. 153, 866–876, doi: 10.1099/mic.0.29275-0 (2007).
Wada, N., Menicanin, D., Shi, S., Bartold, P. M. & Gronthos, S. Immunomodulatory properties of human periodontal ligament stem cells. J. Cell Physiol. 219, 667–676, doi: 10.1002/jcp.21710 (2009).
Socransky, S. S., Haffajee, A. D., Cugini, M. A., Smith, C. & Kent, R. L. Microbial complexes in subgingival plaque. J. Clin Periodontol. 25, 134–144, doi: 10.1111/j.1600-051X.1998.tb02419.x (1998).
Kumar, P. S. et al. New Bacterial Species Associated with Chronic Periodontitis. J. Dent Res. 82, 338–344, doi: 10.1177/154405910308200503 (2003).
De Becker, A. & Riet, I. V. Homing and migration of mesenchymal stromal cells: How to improve the efficacy of cell therapy? World J. Stem Cells. 8, 73–87, doi: 10.4252/wjsc.v8.i3.73 (2016).
Shaw, T. J. & Martin, P. Wound repair: a showcase for cell plasticity and migration. Curr Opin Cell Biol. 42, 29–37, doi: 10.1016/j.ceb.2016.04.001 (2016).
Chatzivasileiou, K., Lux,.C. A., Steinhoff, G. & Lang, H. Dental follicle progenitor cells responses to Porphyromonas gingivalis LPS. J. Cell and Mol Med. 17, 766–773, doi: 10.1111/jcmm.12058 (2013).
Kanafi, M. M., Ramesh, A., Gupta, P. K. & Bhonde, R. R. Influence of hypoxia, high glucose, and low serum on the growth kinetics of mesenchymal stem cells from deciduous and permanent teeth. Cells Tissues Organs. 198, 198–208, doi: 10.1159/000354901 (2013).
Rochefort, G. Y. et al. Multipotential mesenchymal stem cells are mobilized into peripheral blood by hypoxia. Stem Cells. 24, 2202–2208, doi: 10.1634/stemcells.2006-0164 (2006).
Hu, X. et al. Hypoxic preconditioning enhances bone marrow mesenchymal stem cell migration via Kv2.1 channel and FAK activation. Am J. Physiol Cell Physiol. 301, C362–72, doi: 10.1152/ajpcell.00013.2010 (2011).
Bhattacharya, R. et al. Effect of bacteria on the wound healing behavior of oral epithelial cells. PLoS One. 9, e89475, doi: 10.1371/journal.pone.0089475 (2014).
Amano, A. Bacterial adhesins to host components in periodontitis. Periodontol 2000. 52, 12–37, doi: 10.1111/j.1600-0757.2009.00307.x (2010).
Sandros, J., Papapanou, P. & Dahlén, G. Porphyromonas gingivalis invades oral epithelial cells in vitro. J. Periodont Res. 28, 219–226 (1993).
Li, Y. et al. Coinfection with Fusobacterium nucleatum can enhance the attachment and invasion of Porphyromonas gingivalis or Aggregatibacter actinomycetemcomitans to human gingival epithelial cells. Arch. Oral Biol. 60, 1387–1393, doi: 10.1016/j.archoralbio.2015.06.017 (2015).
Matsushita, K. et al. Immunobiological activities of a 55-kilodalton cell surface protein of Prevotella intermedia ATCC 25611. Infect Immun. 62, 2459–2469 (1994).
Hamada, S. et al. The importance of fimbriae in the virulence and ecology of some oral bacteria. Oral Microbiol Immunol. 13, 129–138 (1998).
Inagaki, S., Onishi, S., Kuramitsu, H. K. & Sharma, A. Porphyromonas gingivalis vesicles enhance attachment, and the leucine-rich repeat BspA protein is required for invasion of epithelial cells by “Tannerella forsythia”. Infect Immun. 74, 5023–5028, doi: 10.1128/IAI.00062-06 (2006).
Sharma, A. et al. Tannerella forsythia-induced alveolar bone loss in mice involves leucine-rich-repeat BspA protein. J. Dent Res. 84, 462–467 (2005).
Sabet, M., Lee, S., Nauman, R. K., Sims, T. & Um, H. The surface (S-) layer is a virulence factor of Bacteroides forsythus. Microbiol. 149, 3617–3627, doi: 10.1099/mic.0.26535-0 (2003).
Kirschbaum, M., Schultze-Mosgau, S., Pfister, W. & Eick, S. Mixture of periodontopathogenic bacteria influences interaction with KB cells. Anaerobe. 16, 461–468, doi: 10.1016/j.anaerobe.2010.03.009 (2010).
Bodet, C., Piché, M., Chandad, F. & Grenier, D. Inhibition of periodontopathogen-derived proteolytic enzymes by a high-molecular-weight fraction isolated from cranberry. J. Antimicrob Chemother. 57, 685–690, doi: 10.1093/jac/dkl031 (2006).
Saito, T., Ishihara, K., Kato, T. & Okuda, K. Cloning, expression, and sequencing of a protease gene from Bacteroides forsythus ATCC 43037 in Escherichia coli. Infect Immun. 65, 4888–4891 (1997).
Cassatella, M. A. Interleukin 10 (IL-10) inhibits the release of proinflammatory cytokines from human polymorphonuclear leukocytes. Evidence for an autocrine role of tumor necrosis factor and IL-1 beta in mediating the production of IL-8 triggered by lipopolysaccharide. J. Exp Med. 178, 2207–2211, doi: 10.1084/jem.178.6.2207 (1993).
Cianci, E. et al. Human Periodontal Stem Cells Release Specialized Proresolving Mediators and Carry Immunomodulatory and Prohealing Properties Regulated by Lipoxins. Stem Cells Transl Med. 5, 20–32, doi: 10.5966/sctm.2015-0163 (2016).
Kantarci, A., Oyaizu, K. & Van Dyke, T. E. Neutrophil-mediated tissue injury in periodontal disease pathogenesis: findings from localized aggressive periodontitis. J. Periodontol. 74, 66–75, doi: 10.1902/jop.2003.74.1.66 (2003).
Assinger, A. et al. Efficient phagocytosis of periodontopathogens by neutrophils requires plasma factors, platelets and TLR2. J. Thromb Haemost. 9, 799–809, doi: 10.1111/j.1538-7836.2011.04193.x (2011).
Beklen, A., Hukkanen, M., Richardson, R. & Konttinen, Y. T. Immunohistochemical localization of Toll-like receptors 1-10 in periodontitis. Oral Microbiol Immunol. 23, 425–431, doi: 10.1111/j.1399-302X.2008.00448.x (2008).
Folwaczny, M., Glas, J., Torok, H., Limbersky, O. & Folwaczny, C. Toll-like receptor (TLR) 2 and 4 mutations in periodontal disease. Clin Exp Immunol. 135 (2), S. 330–335, doi: 10.1111/j.1365-2249.2004.02383.x (2004).
Wilensky, A., Tzach-Nahman, R., Potempa, J., Shapira, L. & Nussbaum, G. Porphyromonas gingivalis gingipains selectively reduce CD14 expression, leading to macrophage hyporesponsiveness to bacterial infection. J. Innate Immun. 7, 127–135, doi: 10.1159/000365970 (2015).
Birkedal-Hansen, H. Role of cytokines and inflammatory mediators in tissue destruction. J. Periodont Res. 28, 500–510 (1993).
Haddouti, E. et al. Human dental follicle precursor cells of wisdom teeth: isolation and differentiation towards osteoblasts for implants with and without scaffolds. Mat.-wiss Werkstofftech. 40, 732–737, doi: 10.1002/mawe.200900505 (2009).
Laheij, A. M. G. A., de Soet, J. J., Veermann, E. C. I., Bolscher, J. G. M. & van Loveren, C. The influence of oral bacteria on epithelial cell migration in vitro. Mediators Inflamm. 2013, doi: 10.1155/2013/154532 (2013).
Nuzzi, P. A., Lokuta, M. A. & Huttenlocher, A. Analysis of neutrophil chemotaxis. Methods Mol Biol. 370, 23–36, doi: 10.1007/978-1-59745-353-0_3 (2007).
Leijh, P. C., Van den Barselaar, M. T., Van Zwet, T. L., Dubbeldeman-Rempt, I. & Van Furth, R. Kinetics of phagocytosis of Staphylococcus aureus and Escherichia coli by human granulocytes. Immunol. 37, 453–465 (1979).
Acknowledgements
CH kindly acknowledges funding by the University of Rostock Landesgraduiertenförderung of Mecklenburg Vorpommern, Germany, scholarship program. Purchase of the BD Accuri C6 Flow Cytometer was kindly supported by the EU-EFRE (European Funds for Regional Development) program and funds provided by the University Medicine Rostock.
Author information
Authors and Affiliations
Contributions
C.H., K.K., H.L. and B.K. designed the study. CH performed the experiments. C.H., K.K. and B.K. analyzed and interpreted the experimental data. C.H. prepared all figures and wrote a manuscript draft. B.K. and C.H. wrote the final manuscript version. R.E., M.H. and H.L. contributed to the reagents and helped with data interpretation.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Hieke, C., Kriebel, K., Engelmann, R. et al. Human dental stem cells suppress PMN activity after infection with the periodontopathogens Prevotella intermedia and Tannerella forsythia. Sci Rep 6, 39096 (2016). https://doi.org/10.1038/srep39096
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep39096
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.