Abstract
Extracellular vesicles (EVs) released by eukaryotes, archaea, and bacteria contain proteins, lipids, polysaccharides, and other molecules. The cargo analysis of EVs shows that they contain virulence factors suggesting a role in the pathogenesis of infection. The proteome, lipidome, RNA content, and carbohydrate composition of EVs from Paracoccidioides brasiliensis and Paracoccidioides lutzii were characterized. However, the effects of P. brasiliensis EVs on the host immune system have not yet been investigated. Herein, we verified that EVs from P. brasiliensis induce the production of proinflammatory mediators by murine macrophages in a dose-dependent manner. Addition of EV to macrophages also promoted transcription of the M1-polarization marker iNOs and diminish that of the M2 markers Arginase-1, Ym-1, and FIZZ-1. Furthermore, the augmented expression of M2-polarization markers, stimulated by IL-4 plus IL-10, was reverted toward an M1 phenotype in response to secondary stimulation with EVs from P. brasiliensis. The ability of EVs from P. brasiliensis to promote M1 polarization macrophages favoring an enhanced fungicidal activity, demonstrated by the decreased CFU recovery of internalized yeasts, with comparable phagocytic efficacy. Our results suggest that EVs from P. brasiliensis can modulate the innate immune response and affect the relationship between P. brasiliensis and host immune cells.
Similar content being viewed by others
Introduction
Paracoccidioides brasiliensis and Paracoccidioides lutzii are thermodimorphic pathogenic fungi that are the etiologic agents of paracoccidioidomycosis (PCM), a disease endemic to Latin America associated with severe public health problems. PCM starts by the inhalation of airborne propagules from fungal mycelia, which convert into yeasts in the lungs, causing granuloma formation and adversely affecting the functions of other infected organs1,2,3. Active PCM mostly affects the lungs, but it may develop into an acute form or, more frequently, reactivate later as a chronic and insidious disease that can disseminate to many different organs and tissues4,5,6. Although the mechanisms by which the host controls PCM remain unclear, modulation of the immune system is crucial to determine the progress of the infection, and cellular immunity is the principal defense mechanism involved in PCM.
The secretion of fungal components is critical for the establishment of a successful infection, as is reported for Candida albicans7, Histoplasma capsulatum8, Cryptococcus neoformans9. Some fungal components are secreted through conventional mechanisms, involving vesicles of the post-Golgi network that move to and fuse with the plasma membrane to release their cargo through exocytosis10. Eukaryotes evolved unconventional secretion mechanisms to release proteins into the extracellular milieu11,12,13,14,15, including secretion through exosomes. Exosomes are formed by internal vesicles present in the lumen of endosomes, which generate multivesicular bodies that fuse with the plasma membrane, resulting in the release of internal vesicles into the extracellular milieu. These fungal extracellular vesicles (EVs), also termed fungal exosomes, contain a wide assortment of proteins, lipids, polysaccharides, and nucleic acid. In the case of P. brasiliensis, EVs were first purified from the supernatant of yeast cultures16 and identified by the presence of terminal Gal-α –(1,3)-Gal (α –Gal) epitopes. Subsequently, EVs from P. brasiliensis and P. lutzii were characterized with regards to their proteome17, lipidome18, RNA content19, and carbohydrate composition20.
Several virulence factors that enhance pathogen survival in the host by allowing evasion of immune surveillance possible have been associated with fungal EVs21,22. In addition, several cellular factors released by fungi have been associated with immunomodulation14,15,23,24,25,26,27. Studies on the immunomodulatory activity of EVs allow a better understanding of how the host immune response may be influenced by fungal components. Immunomodulation by EVs may be directed toward macrophages, which are essential in guiding the ensuing development of adaptive immunity28. It is known that macrophages can be engaged in different types of activation: “classic” M1 macrophages are inflammatory cells that phagocytize and kill microbes, while “alternative” M2 cells work in favor of angiogenesis, and tissue remodeling and repair29. However, capacity for EVs from P. brasiliensis to mediate immunomodulatory effects has not been investigated. A recent study showed that in chronic PCM the majority of macrophages are M230, which contribute to the development of a Th2 immune response that is associated with susceptibility to the infection30,31. Therefore, we hypothesized that EVs from P. brasiliensis could play a determinant role in the interaction of the pathogen with macrophages and could modulate host immunity, as was reported for EVs from C. neoformans15.
In this study, we investigated whether EVs from P. brasiliensis affected the polarization of macrophages and their effects on macrophage phagocytosis and fungicidal activity against P. brasiliensis. EVs from P. brasiliensis were found to induce M1 polarization of macrophages and enhance the fungicidal activity of murine macrophages. Our results suggest that EVs of P. brasiliensis can influence the interaction of the fungus with host cells.
Results
P. brasiliensis EVs induce proinflammatory mediators in murine peritoneal macrophages
Extracellular vesicles have recently been isolated from culture supernatants of P. brasiliensis yeasts and characterized regarding their proteome, lipidome, and carbohydrate content18,20. Since the influence of the vesicles on the host innate immunity cells has not been evaluated, we examined whether EVs produced by P. brasiliensis yeasts could stimulate macrophages. To do so we added various quantities of EVs to murine peritoneal macrophages and assessed the culture supernatant for the production of nitric oxide and cytokines after 48 h of incubation. EVs induced the release of NO, IL-12p40, IL-12p70, IL-6, TNF-α, IL-1α, and IL-1β in a dose-dependent manner (Fig. 1). In contrast, the detected levels of IL-10 were as low as those released by unstimulated macrophages (data not show). These findings show that EVs induce murine macrophages to produce proinflammatory mediators.
EVs from P. brasiliensis induce the production of proinflammatory mediators by peritoneal macrophages.
Peritoneal macrophages (1.5 × 106/mL) of C57BL/6 mice were incubated at 37 °C for 48 h with the indicated amounts of extracellular vesicles from P. brasiliensis (x axis). The medium and LPS (1 μg/mL) plus IFN-γ (2 ng/mL) were used as negative and positive controls, respectively. The culture supernatants were assessed for nitrite (a), TNF-α (b), IL-6 (c), IL-12p40 (d), IL-12p70 (e), IL-1α (f), and IL-1β (g) concentrations. The results, expressed as mean ± SEM, were compared to the levels in unstimulated cells (with the medium only). Differences were considered significant when p < 0.05 (*).
P. brasiliensis EVs stimulate J774A.1 cells to produce proinflammatory cytokines
We also evaluated the effects of the EVs on murine macrophages of the cell line J774A.1. The cells were incubated for 48 h with several quantities of EVs, and the culture supernatants were assessed for cytokines production. TNF-α, IL-6, and IL-12 levels significantly increased in response to the EV stimulus in a dose-dependent manner (Fig. 2). These observations corroborate with the capacity of EVs to promote a proinflammatory profile in murine macrophages.
EVs from P. brasiliensis induce the production of proinflammatory mediators by the macrophage cell line J774A.1.
J774A.1 cells (1.5 × 106/mL) were incubated at 37 °C for 48 h with the indicated amounts of extracellular vesicles from P. brasiliensis (x axis). The medium and LPS (1 μg/mL) plus IFN-γ (2 ng/mL) were used as negative and positive controls, respectively. The culture supernatants were assessed for TNF-α (a), IL-6 (b), and IL-12p40 (c) levels. The results, expressed as mean ± SEM, were compared to the levels in unstimulated cells (with the medium only). Differences were considered significant when p < 0.05 (*).
P. brasiliensis EVs induce macrophage M1 phenotype
The high production of proinflammatory mediators suggests that EVs could favor the development of macrophages toward the “classical” M1 activation phenotype. To investigate this hypothesis, we extracted total RNA of macrophages that had been incubated with EVs for 6 h and carried out the relative quantification of transcripts of M1 (iNOs) and M2 (Arginase-1, Ym-1, and FIZZ-1) polarization markers. The iNOs mRNA increased 5800-fold in EV-stimulated murine peritoneal macrophages, a response that overcame that induced by the IFN-γ plus IL-12 stimulus (Fig. 3a). In contrast, the relative expression of FIZZ-1 mRNA was reduced significantly under the EV stimulus. Consistently, the expression of Arginase-1 and Ym-1 mRNA in the presence of vesicles remained close to that found in unstimulated cells (Fig. 3b–d). These results indicate that P. brasiliensis EVs promote the polarization of macrophages towards the “classical” M1 phenotype.
EVs from P. brasiliensis promote macrophage classical activation.
Macrophages (2 × 106/mL) of C57BL/6 mice were incubated at 37 °C for 6 h with EVs (10 μg/mL) and IFN-γ (2 ng/mL) plus IL-12p40 (50 ng/mL) as M1 inducers (classical activation) or IL-10 plus IL-4 (50 ng/mL both) as M2 inducers (alternative activation). The medium was used as a negative control. Following RNA extraction and conversion into cDNA, the relative expressions of iNOS (a), FIZZ1 (b), Arginase-1 (c), and Ym-1 (d) were determined by real-time PCR. The results, expressed as mean ± SEM, were compared to those obtained from the negative control. Differences were considered significant when p < 0.05 (*).
EVs from P. brasiliensis induce switching from M2 to M1 macrophages
In fungal infections, macrophage polarization is plastic, the cells being able to change from the M2 (‘non-protective’) to the M1 (‘protective’) phenotype32. We investigated whether EVs from P. brasiliensis could promote the switching of macrophages from an M2 to an M1 phenotype. We stimulated murine peritoneal macrophages with EVs (10 μg/mL) or IL-4 (50 ng/mL) plus IL-10 (50 ng/mL) to develop M1 or M2 macrophages, respectively. The medium alone was used as a negative control. After 24 h, the cells were washed and subjected to a secondary stimulation for 48 h: cells that had previously been stimulated with IL-4 plus IL-10 were now re-stimulated with EVs, and vice-versa. Cell supernatants were assessed for NO concentration. We found that the NO production by cells stimulated with IL-4 plus IL-10 was low and was reverted by EVs re-stimulation (Fig. 4b), whereas the NO production by macrophages stimulated with EVs was high and was significantly decreased when re-stimulated with IL-4 plus IL-10 (Fig. 4b). The relative expression of M1 and M2 polarization markers was also examined. The relative expression of iNOs mRNA increased under the EV stimulus and significantly decreased after secondary stimulation with IL-4 plus IL-10. As expected, stimulation with IL-4 plus IL-10 did not induce relative expression of iNOs, a scenario that was modified under re-stimulation with EVs, which promoted a significant relative expression of iNOs mRNA (Fig. 4c). Further, the relative expression of M2 polarization markers (Arginase and YM1) was induced by IL-4 plus IL-10 and not by EVs. The expression induced by IL-4 plus IL-10 decreased significantly under restimulation with EVs (Fig. 4c,d), whereas restimulation with IL-4 plus IL-10 reverted the negative response to EV-stimulation.
EVs from P. brasiliensis induce switching from M2 to M1 macrophages.
(a) Peritoneal macrophages (2 × 106/mL) were incubated at 37 °C with EVs (10 μg/mL; red), IL-4 plus IL-10 (50 ng/mL both; blue), and the medium as a negative control (green). After 24 h, the cells were washed and subjected to re-stimulation for 48 h as follows: the macrophages that were stimulated with IL-4 plus IL-10 (blue) during the first 24 hours were then re-stimulated with EVs (red); those stimulated for 24 h with EVs (red) were then re-stimulated with IL-4 plus IL-10 (blue). The culture supernatants were assessed for nitrite concentration (b), and cells were analyzed by real-time PCR for the relative expression of iNOS (c), Arginase-1 (d), and Ym-1 (e). The results, expressed as mean ± SEM, were compared to those obtained from the negative control. Differences were considered significant when p < 0.05 (*). An additional comparison was made between the results obtained at 24 and 48 h, represented as blue or red bars (#). Differences were considered significant when p < 0.05.
In addition, we stimulated murine peritoneal macrophages with EVs (10 μg/mL), IL-4 (50 ng/mL) plus IL-10 (50 ng/mL), or IL-12 (50 ng/mL) plus IFN-γ (50 ng/mL). After 24 h of maintained stimulation to develop M2 macrophages, cells were re-stimulated, for 48 h, with EVs or IL-12 plus IFN-γ (Fig. 5a). The relative expression of iNOs (M1) and Arginase (M2) was determined, showing that iNOs mRNA increased after re-stimulation with EV or IL-12 plus IFN-γ (Fig. 5b). In contrast, re-stimulation with EVs did not change the Arginase expression by macrophages, i.e., it was similar to the verified in the absence of re-stimulus (medium) (Fig. 5c), indicating that the M2 phenotype of macrophages was maintained. The major conclusion of these results is that P. brasiliensis EVs can stimulate macrophage switching from an M2 toward an M1 phenotype.
EVs from P. brasiliensis induce M1 macrophages under conditions that favor the development of M2 phenotype.
(a) Peritoneal macrophages (2 × 106/mL) were incubated at 37 °C with EVs (10 μg/mL; red), IL-4 plus IL-10 (50 ng/mL both; blue), IL-12 plus IFN-γ (50 ng/mL both; black) and the medium as a negative control (green). After 24 h, the cells previously stimulated with IL-4 plus IL-10 (blue) were re-stimulated for 48 h with IL-12 plus IFN-γ (50 ng/mL both; black) or EVs (40 μg/mL; red). The cells were analyzed by real-time PCR for the relative expression of iNOS (b) and Arginase (c). The results, expressed as mean ± SEM, were compared to those obtained from the negative control (medium, green). Differences were considered significant when p < 0.05 (*).
EVs from P. brasiliensis stimulate the fungicidal activity of macrophages
Because EV-stimulation of macrophages induces the production of proinflammatory mediators and M1 polarization, we examined whether EVs could promote phagocytosis and killing of P. brasiliensis. Macrophages previously treated for 24 h with IFN-γ (50 ng/mL), EVs (10 μg/mL), or the medium were incubated with propidium iodide (PI)-stained P. brasiliensis. After 2 h, the percentage of macrophages containing adhering or internalized PI-stained yeasts was determined by flow cytometry. A similar proportion of macrophages containing PI-stained yeasts was found in unstimulated cells and cells stimulated with IFN-γ or EVs (Fig. 6a). In addition, the CFU recovery from the supernatant of murine peritoneal macrophages was similar between unstimulated, IFN-γ-stimulated, and EVs-stimulated cells (Fig. 6b). Remarkably, after 48 h of incubation, the CFU recovery from the macrophage lysate showed that the stimulation with either IFN-γ or EVs was associated with a CFU count lower than that obtained from unstimulated macrophages (Fig. 6d). We conclude that EV-stimulated macrophages exhibit a high fungicidal activity, comparable to those induced by IFN γ.
EVs from P. brasiliensis enhanced the fungicidal activity of macrophages.
Peritoneal macrophages (1.5 × 106/mL), treated for 24 h with EVs (10 μg/mL), IFN-γ (50 ng/mL), or the medium were washed and infected with P. brasiliensis (yeast-to-macrophage ratio of 1:1) and labeled with propidium iodide (PI), for 2 h. The macrophages were analyzed by flow cytometry. The percentage of PI-stained cells is shown in (a) (histogram) and (b) (bars). Alternatively, macrophages were infected with P. brasiliensis (yeast-to-macrophage ratio of 1:10), for 4 h. The cell supernatants were harvested and assessed for CFU, as a measurement of the presence of extracellular P. brasiliensis (c). After washing gently, the medium was added to the cells, and they were cultured for an additional 48 h. The cells were washed and lysed for the detection of viable intracellular yeasts by CFU (d). The results, expressed as mean ± SEM, were compared to those obtained from the negative control. Differences were considered significant when p < 0.05 (*).
Discussion
Herein we reported that EVs from P. brasiliensis induce the activation of peritoneal macrophages and that they can modulate the host innate immunity. We verified that murine peritoneal macrophages and the murine macrophage cell line J774A.1 released pro-inflammatory mediators in response to EVs stimulation, which in turn accounted for the development of M1 macrophages. Moreover, we showed that EVs could repolarize M2 macrophages toward an M1 profile, which was accompanied by an enhanced fungicidal capacity of the macrophages.
EVs released from infected cells have been studied more often than those released by the pathogens themselves. The studies found that EVs of host origin may contain inflammatory mediators that recruit and activate leukocytes and promote elimination of the invading organism. Nonetheless, the EVs released from infected cells contain pathogen components, many of which are known to act as major drivers of host immunity [reviewed by ref. 33]. The presence of EVs released from infected cells was demonstrated during viral, bacterial, parasitical, and fungal infections, and their primary function was shown to be immunomodulation. In the present study, we focused on vesicles released directly by the fungi, an approach we adopted from prior studies showing that extracellular vesicles from Cryptococcus neoformans activate macrophages, promoting cytokine production and restricting the fungal infection15. Furthermore, another study showed that C. neoformans EVs favor the C. neoformans infection, since interference with the export of exosomes decreased the virulence of C. neoformans11. A recent study demonstrated that EVs from Malassezia sympodialis enhance TNF-α and IL-4 production in peripheral blood mononuclear cells34, whereas EVs from Candida albicans stimulate macrophages and dendritic cells to produce proinflammatory mediators and up-regulate the expression of CD86 and MHC-II9. In addition, EVs isolated from supernatants of Saccharomyces cerevisae and Histoplasma capsulatum have been well characterized13,15; however, the studies provided limited insight into the influence of their EVs on immunomodulation. Regarding the studies on EVs from P. brasiliensis, Puccia and colleagues performed a series of studies that provide relevant information regarding the characterization of EVs. They elucidated the molecules of P. brasiliensis that EVs carry into the extracellular environment16 by describing the proteome17, lipidome18, as well as the RNA19 and carbohydrate20 content of the vesicles. However, the influence of P. brasiliensis EVs on the host immunity and PCM pathogenesis were not investigated.
P. brasiliensis EVs stimulated the development of M1 macrophages, which was characterized by the production of inflammatory cytokines and nitric oxide and by the augmented expression of iNOS2, besides reinforced by the fact that P. brasiliensis EVs did not induce macrophages to produce IL-10 (data not show). This profile contrasted with the one of M2 macrophages, induced by IL-4 plus IL-10 in our study, which was discriminated by the expression of Arginase-1, FIZZ1, and YM-135. Immune modulation towards the M1 phenotype is strongly correlated to the outcome of the immune response to fungal infections, contributing to fungal clearance during experimental infections with Cryptococcus neoformans32 and Candida albicans36,37,38. However, there are somewhat conflicting observations on the role played by M1 or M2 macrophages in P. brasiliensis infection. The susceptible B10A mouse strain has an innate tendency to polarize macrophages into M1 phenotype, and the opposite polarization occurs in resistant A/J mice, supporting the idea that susceptibility and resistance to P. brasiliensis infection are strongly associated with M1 and M2 polarization, respectively39,40,41. However, the association of resistance with M1 polarization is supported by the fact that dectin-1 KO mice infected with P. brasiliensis develop M2 polarization, which impairs the fungicidal ability and diminishes survival rates (27). The association of M1 polarization and resistance to P. brasiliensis infection was reinforced recently by the report that the fungal lectin paracoccin, which exerts a therapeutic effect against PCM42, induces M1 polarization of peritoneal macrophages43.
We found that EVs from P. brasiliensis induce macrophages to switch their phenotype from M2 to M1. Interestingly, during the course of C. neoformans infection, the polarization status of pulmonary macrophages changes over time by repolarization of individual macrophages or the replacement of M2-polarized (non-protective) by new, M1-polarized (protective) cells. These mechanisms support the long-term persistence of the pathogen32. In addition, C. albicans blocked switching of the M2 to the M1 phenotype through the suppression of the host inflammatory response44. The plasticity of macrophage polarization during P. brasiliensis infection has not been previously evaluated; our data demonstrate, for the first time, the occurrence of macrophage repolarization from M2 to M1 in response to P. brasiliensis EVs. Furthermore, we showed that such M1 polarization is only partially reverted by the presence of M2-driving cytokines. Although we did not assess the occurrence of macrophage polarization in vivo, we hypothesize that P. brasiliensis EVs modulate immunity of infected mice. Ongoing studies of our laboratory investigate whether the intranasal administration of P. brasiliensis EVs effectively activates alveolar macrophages, as verified in vitro, and induces resistance to the infection. Positive responses may open new perspectives in the immunotherapy of PCM.
We used PI-stained P. brasiliensis to evaluate the interaction of the yeast with macrophages that were previously stimulated with EVs. The M1 polarization of macrophages showed to be induced by EVs and did not influence phagocytizing of the yeasts. The proportion of macrophages that adhered to or ingested PI-stained yeasts was similar between cells incubated with EVs, IFN-γ, or the medium alone. The responses to IFN-γ and the medium were close to those reported by Costa et al.31 when studying the influence of IL-10 on the phagocytic activity of macrophages. The results we obtained in the phagocytosis assay were consistent with the number of CFUs recovered from the extracellular milieu, which did not differ among macrophages incubated with EVs, IFN-γ, or the medium alone either. However, as reported by Oliveira et al.15, EVs from C. neoformans enhanced the phagocytic activity of RAW 264.7.
Notably, macrophages stimulated with EVs showed enhanced intracellular killing of P. brasiliensis, evident by the lower recovery of yeast CFU from lysed macrophages. This finding is consistent with the fact that the production of NO, a fungicidal compound, increased following macrophage stimulation with EVs from P. brasiliensis, as well as with IFN-γ. EVs from C. neoformans and C. albicans were also reported to enhance the fungicidal activity of macrophages9,15.
In summary, we studied the ability of EVs from P. brasiliensis to modulate peritoneal macrophage polarization with an effector mechanism of fungal elimination. In this context, EV components from P. brasiliensis account for macrophage activation, production of pro-inflammatory mediators, M1 polarization, and killing of the fungus. These biological activities triggered by EVs on peritoneal macrophages were summarized in a proposed model shown in Fig. 7. The effects of P. brasiliensis EVs on macrophage functionality raise questions regarding the benefits of the host or the immune response subversion eventually provided by the production of EVs.
A proposed model that demonstrate the effects of EVs from P. brasiliensis on murine peritoneal macrophages.
EVs from P. brasiliensis yeast have the ability to induce proinflammatory mediator’s production by murine peritoneal macrophages. Moreover, M1 polarization induced by EVs is associated with the increase in fungicidal activity. In addition, EVs from P. brasiliensis induce switching from M2 to M1 macrophages, a fact that suggests the EVs activity as a modulator of innate immune response.
Methods
Ethics statement
This study was approved by the Committee of Ethics in Animal Research of the College of Medicine of Ribeirão Preto at the University of São Paulo and was conducted in accordance with the Ethical Principles in Animal Research adopted by the Brazilian College of Animal Experimentation, Protocol number 20/2013-1.
Mice and P. brasiliensis isolates
Male C57BL/6 (wild-type, WT) mice at 6–8 weeks of age were used in this study. They were acquired from the animal house of the Campus of Ribeirão Preto, University of São Paulo, Ribeirão Preto, São Paulo, Brazil. The animals were housed in the animal facility of the Molecular and Cellular Biology Department of the Faculty of Medicine of Ribeirão Preto, University of São Paulo, under optimized hygienic conditions.
The P. brasiliensis isolate Pb18 was maintained by weekly subcultivation in the YPD medium (2% peptone, 1% yeast extract, and 2% glucose) in the yeast phase, at 36 °C. To ensure virulence of the yeast, serial passages in BALB/c mice were performed before the isolate Pb18 was used in experiments.
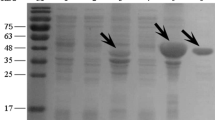
Vesicle isolation
EVs were obtained as previously described by Vallejo et al.16. Yeast cells were transferred into Erlenmeyer flasks containing 200 mL of Ham’s F12 medium (Gibco, Carlsbad, CA, USA) supplemented with 1.5% glucose (Sigma-Aldrich, St. Louis, MO, USA) and cultivated for 4 days at 36 °C with continuous shaking (pre-inocula). The yeast cells from the pre-inocula were harvested and inoculated in 500 mL of fresh medium for another 48 h. A cell-free supernatant was obtained by sequential centrifugation at 5,000 g (15 min) and 15,000 g (30 min) at 4 °C. The pellets were discarded, and the supernatants ultra/diafiltrered using a membrane with a 100-kDa cutoff (Millipore, Billerica, MA, USA). The material was centrifuged at 15,000 g (30 min) to remove aggregates, and the resulting supernatant was centrifuged at 100,000 g for 1 h to precipitate vesicles. Vesicle pellets were washed in phosphate-buffered saline (PBS) and finally suspended in PBS for further analysis. The vesicle quantification was performed based on the analysis of sterol in their membranes, using a quantitative fluorimetric Amplex Red sterol assay kit (Molecular Probes, Thermo Fisher Scientific, Waltham, MA, USA), according to the manufacturer’s instructions.
Preparation of murine peritoneal macrophages and the murine macrophage cell line J774A.1
Peritoneal macrophages were obtained from the peritoneal cavity of C57BL/6 mice that received an intraperitoneal injection of 1.0 mL of 3% sterile sodium thioglycollate medium (Sigma-Aldrich) 4 days earlier. The cells were harvested by peritoneal lavage with 5 mL of cold sterile PBS and centrifuged at 300 g (10 min at 4 °C). The pellet obtained was washed twice at 300 g for 10 min at 4 °C in Roswell Park Memorial Institute (RPMI) 1640 medium (Life Technologies, Grand Island, NY, USA) supplemented with 10% fetal cow serum (FCS; Life Technologies), 1% streptomycin/penicillin, and 2 mM L-glutamine (Sigma-Aldrich). Cells of the macrophage lineage J774A.1 were cultured in T75 flasks in RPMI 1640 containing 10% FCS supplemented with 1% streptomycin/penicillin and 2 mM L-glutamine (Sigma-Aldrich). Flasks were kept at 37 °C in an atmosphere of humidified air containing 5% CO2. The cells were maintained at subconfluent densities, and passages were performed every 2–3 days.
Macrophages and macrophage-like cells were incubated with EVs at different concentrations (1.25–40 μg/mL), LPS (1 μg/mL) plus IFN-γ (2 ng/mL), IL-4 (50 ng/mL) plus IL-10 (50 ng/mL), IFN-γ (50 ng/mL) plus IL-12 (50 ng/mL), or with the medium alone. The macrophages were cultured for 6 h for real-time quantitative PCR analysis, 48 h for determining the TNF-α, IL-12p40, IL-12p70, IL-1β, IL-1α, IL-6, and NO levels, or 24 h for quantifying their phagocytosis and killing of P. brasiliensis.
Measurement of nitric oxide (NO) production
Supernatants from macrophage cell cultures (1.5 × 106/mL; 7.5 × 105 cells/well; 48-well plates) were used to measure the production of NO, which was inferred by measuring the accumulation of nitrite in the monolayer supernatants by a standard Griess reaction45. In short, 50 μL of each supernatant was incubated with an equal volume of Griess reagent (1.0% sulfanilamide, 0.1% naphthalenediaminedihydrochloride, and 2.5% H3PO4) and distributed in a 96-well microplate for 10 min at room temperature. The absorbance at 550 nm was measured using a Power Wave-X microplate reader (BioTek Instruments, Inc., Winooski, VT, USA). The conversion of absorbance values into micromolar (μM) concentrations of NO was done on the basis of a standard curve, concomitantly generated by using known concentrations of NaNO2 diluted in RPMI medium.
Cytokine measurement
Supernatants of stimulated macrophages (1.5 × 106/mL; 7.5 × 105 cells/well; 48-well plates) were assessed for their levels of IL-12p40, IL-12p70, IL-6, TNF-α, IL-1α, and IL-1β. The cytokines were measured by capture enzyme-linked immunosorbent assay (ELISA) with antibody pairs purchased from BD Biosciences (Pharmingen, San Diego, CA, USA). The ELISA was performed according to the manufacturer’s protocol. The cytokine concentrations were determined from standard curves, using murine recombinant cytokines as a standard. The absorbance was read at 450 nm in the Power Wave-X microplate scanning spectrophotometer (BioTek Instruments, Inc.).
Quantitative reverse transcription (qRT)-PCR
After 6 h of stimulation, the murine peritoneal macrophages (2 × 106/mL; 1 × 106 cells/well; 24-well plates) were used to extract the total RNA using the Trizol Reagent (Invitrogen, Life Technologies, Camarillo, CA, USA), according to the manufacturer’s instructions. The total RNA was reverse-transcribed into cDNA by the ImProm-II Reverse Transcription System (Promega, Fitchburg, WI, USA) using oligo(dT). qRT-PCR was performed in 15 μL, the reactions were using carried out by SYBR Green (Applied Biosystems/Life Technologies, Carlsbad, CA, USA) on a 7500 Real-Time PCR System (Applied Biosystems), under the following conditions: 50 °C for 2 min, 95 °C for 10 min, and 40 cycles of 95 °C for 15 sec/60 °C for 1 min. The relative expression of transcripts was quantified using the ΔΔCt method, and β-actin was used as the endogenous control. PCR primers utilized were: β-actin (F-CCTAAGGCCAACCGTGAAAA, R-GAGGCATACAGGGACAGCACA), Ym1 (F-TCACAGGTCTGGCAATTCTTCTG, R-ACTCCCTTCTATTGGCCTGTCC), Arginase-1 (F-GTTCCCAGATGTACCAGGATTC, R-CGATGTCTTTGGCAGATATGC), FIZZ1 (F-CCTGAGATTCTGCCCCAGGAT, R-TTCACTGGGACCATCAGCTGG), and iNOS2 (F-CCGAAGCAAACATCACATTCA, R-GGTCTAAAGGCTCCGGGCT).
Phagocytosis and fungicidal activity assays of macrophages
Thioglycollate-induced peritoneal macrophages (1.5 × 106/mL; 7.5 × 105 cells/well; 48-well plates) were infected with P. brasiliensis cells for phagocytosis and fungicidal activity assays 24 h after stimulation. For the phagocytosis assay, the infection was performed with propidium iodide (PI)-stained P. brasiliensis, at a macrophage-to-yeast ratio of 1:1. The labeling of P. brasiliensis cells was performed according to the method reported by other studies31,40,46. The cells were cocultivated for 2 h at 37 °C. The supernatants were then removed and the cells washed with PBS to remove any yeast cells that were not ingested or that did not adhere. The macrophages were harvested and analyzed by flow cytometry (Guava easyCyte, Guava Technologies, Millipore, Hayward, CA, USA) for PI-staining. For the fungicidal activity assay, macrophages were cocultivated with P. brasiliensis in a macrophage-to-yeast ratio of 10:1 for 4 h at 37 °C. The macrophage monolayer was then washed, and the macrophages were cultivated for an additional 48 hours. Afterwards, the supernatants were removed and distilled water (100 μL) was added to the monolayer to promote macrophage lysis. The material was assayed for the presence of viable yeasts by the colony forming units (CFU) assay, as described previously47.
Statistical Analysis
Statistical analyses were performed using the GraphPad Prism software (GraphPad Software, San Diego, CA). All data are presented as the mean ± SEM (standard error mean) of independent experiments performed (n = 3 for each group). Statistical determinations of the difference between means of groups were performed with the analysis of variance (1-way), followed by Bonferroni’s multiple comparison tests. Differences with p < 0.05 were considered statistically significant.
Additional Information
How to cite this article: da Silva, T. A. et al. Extracellular vesicles from Paracoccidioides brasiliensis induce M1 polarization in vitro. Sci. Rep. 6, 35867; doi: 10.1038/srep35867 (2016).
References
Brummer, E., Castaneda, E. & Restrepo, A. Paracoccidioidomycosis: an update. Clin Microbiol Rev 6, 89–117 (1993).
Restrepo, A., McEwen, J. G. & Castaneda, E. The habitat of Paracoccidioides brasiliensis: how far from solving the riddle? Med Mycol 39, 233–241 (2001).
Teixeira, M. M. et al. Phylogenetic analysis reveals a high level of speciation in the Paracoccidioides genus. Molecular Phylogenetics and Evolution 52, 273–283, 10.1016/J.Ympev.2009.04.005 (2009).
Laniado-Laborin, R. Coccidioidomycosis and other endemic mycoses in Mexico. Rev Iberoam Micol 24, 249–258, 200724249 [pii] (2007).
de Almeida, S. M. Central nervous system paracoccidioidomycosis: an overview. Braz J Infect Dis 9, 126–133, S1413-86702005000200002 (2005).
Restrepo, A. Morphological aspects of Paracoccidioides brasiliensis in lymph nodes: implications for the prolonged latency of paracoccidioidomycosis? Med Mycol 38, 317–322 (2000).
Monod, M. & Borg-von Zepelin, M. Secreted proteinases and other virulence mechanisms of Candida albicans. Chem Immunol 81, 114–128 (2002).
Batanghari, J. W., Deepe, G. S. Jr., Di Cera, E. & Goldman, W. E. Histoplasma acquisition of calcium and expression of CBP1 during intracellular parasitism. Mol Microbiol 27, 531–539 (1998).
Vargas, G. et al. Compositional and immunobiological analyses of extracellular vesicles released by Candida albicans. Cell Microbiol 17, 389–407, 10.1111/cmi.12374 (2015).
Glick, B. S. & Malhotra, V. The curious status of the Golgi apparatus. Cell 95, 883–889 (1998).
Panepinto, J. et al. Sec6-dependent sorting of fungal extracellular exosomes and laccase of Cryptococcus neoformans. Mol Microbiol 71, 1165–1176, 10.1111/j.1365-2958.2008.06588.x (2009).
Manjithaya, R., Anjard, C., Loomis, W. F. & Subramani, S. Unconventional secretion of Pichia pastoris Acb1 is dependent on GRASP protein, peroxisomal functions, and autophagosome formation. J Cell Biol 188, 537–546, 10.1083/jcb.200911149 (2010).
Albuquerque, P. C. et al. Vesicular transport in Histoplasma capsulatum: an effective mechanism for trans-cell wall transfer of proteins and lipids in ascomycetes. Cell Microbiol 10, 1695–1710, 10.1111/j.1462-5822.2008.01160.x (2008).
Rodrigues, M. L. et al. Extracellular vesicles produced by Cryptococcus neoformans contain protein components associated with virulence. Eukaryotic Cell 7, 58–67, 10.1128/Ec.00370-07 (2008).
Oliveira, D. L. et al. Extracellular vesicles from Cryptococcus neoformans modulate macrophage functions. Infect Immun 78, 1601–1609, 10.1128/IAI.01171-09 (2010).
Vallejo, M. C. et al. The pathogenic fungus Paracoccidioides brasiliensis exports extracellular vesicles containing highly immunogenic alpha-Galactosyl epitopes. Eukaryot Cell 10, 343–351, 10.1128/EC.00227-10 (2011).
Vallejo, M. C. et al. Vesicle and vesicle-free extracellular proteome of Paracoccidioides brasiliensis: comparative analysis with other pathogenic fungi. J Proteome Res 11, 1676–1685, 10.1021/pr200872s (2012).
Vallejo, M. C. et al. Lipidomic analysis of extracellular vesicles from the pathogenic phase of Paracoccidioides brasiliensis. PLoS One 7, e39463, 10.1371/journal.pone.0039463 (2012).
da Silva, R. P. et al. Extracellular vesicle-mediated export of fungal RNA. Sci Rep 5, 7763, 10.1038/srep07763 (2015).
Peres da Silva, R. et al. Extracellular vesicles from Paracoccidioides pathogenic species transport polysaccharide and expose ligands for DC-SIGN receptors. Sci Rep 5, 14213, 10.1038/srep14213 (2015).
Bliska, J. B., Wang, X., Viboud, G. I. & Brodsky, I. E. Modulation of innate immune responses by Yersinia type III secretion system translocators and effectors. Cell Microbiol 15, 1622–1631, 10.1111/cmi.12164 (2013).
Rana, R. R. et al. Yersinia pestis TIR-domain protein forms dimers that interact with the human adaptor protein MyD88. Microb Pathog 51, 89–95, 10.1016/j.micpath.2011.05.004 (2011).
Eigenheer, R. A., Jin Lee, Y., Blumwald, E., Phinney, B. S. & Gelli, A. Extracellular glycosylphosphatidylinositol-anchored mannoproteins and proteases of Cryptococcus neoformans. FEMS Yeast Res 7, 499–510, 10.1111/j.1567-1364.2006.00198.x (2007).
Almeida, F., Wolf, J. M. & Casadevall, A. Virulence-associated enzymes of Cryptococcus neoformans. Eukaryot Cell 14, 1173–1185, 10.1128/EC.00103-15 (2015).
Beauvais, A. et al. Dipeptidyl-peptidase IV secreted by Aspergillus fumigatus, a fungus pathogenic to humans. Infect Immun 65, 3042–3047 (1997).
Chaffin, W. L., Lopez-Ribot, J. L., Casanova, M., Gozalbo, D. & Martinez, J. P. Cell wall and secreted proteins of Candida albicans: identification, function, and expression. Microbiol Mol Biol Rev 62, 130–180 (1998).
Djordjevic, J. T., Del Poeta, M., Sorrell, T. C., Turner, K. M. & Wright, L. C. Secretion of cryptococcal phospholipase B1 (PLB1) is regulated by a glycosylphosphatidylinositol (GPI) anchor. Biochemical Journal 389, 803–812, 10.1042/Bj20050063 (2005).
Hussell, T. & Bell, T. J. Alveolar macrophages: plasticity in a tissue-specific context. Nat Rev Immunol 14, 81–93, 10.1038/nri3600 (2014).
Murray, P. J. & Wynn, T. A. Protective and pathogenic functions of macrophage subsets. Nat Rev Immunol 11, 723–737, 10.1038/nri3073 (2011).
de Carli, M. L. et al. M2 macrophages and inflammatory cells in oral lesions of chronic paracoccidioidomycosis. J Oral Pathol Med 45, 141–147, 10.1111/jop.12333 (2016).
Costa, T. A. et al. In Pulmonary Paracoccidioidomycosis IL-10 Deficiency Leads to Increased Immunity and Regressive Infection without Enhancing Tissue Pathology. Plos Neglected Tropical Diseases 7, 10.1371/journal.pntd.0002512 (2013).
Davis, M. J. et al. Macrophage M1/M2 polarization dynamically adapts to changes in cytokine microenvironments in Cryptococcus neoformans infection. MBio 4, e00264–00213, 10.1128/mBio.00264-13 (2013).
Schorey, J. S., Cheng, Y., Singh, P. P. & Smith, V. L. Exosomes and other extracellular vesicles in host-pathogen interactions. EMBO Rep 16, 24–43, 10.15252/embr.201439363 (2015).
Gehrmann, U. et al. Nanovesicles from Malassezia sympodialis and host exosomes induce cytokine responses–novel mechanisms for host-microbe interactions in atopic eczema. PLoS One 6, e21480, 10.1371/journal.pone.0021480 (2011).
Lawrence, T. & Natoli, G. Transcriptional regulation of macrophage polarization: enabling diversity with identity. Nat Rev Immunol 11, 750–761, 10.1038/nri3088 (2011).
Reales-Calderon, J. A., Aguilera-Montilla, N., Corbi, A. L., Molero, G. & Gil, C. Proteomic characterization of human proinflammatory M1 and anti-inflammatory M2 macrophages and their response to Candida albicans. Proteomics 14, 1503–1518, 10.1002/pmic.201300508 (2014).
Hardison, S. E. et al. Pulmonary infection with an interferon-gamma-producing Cryptococcus neoformans strain results in classical macrophage activation and protection. Am J Pathol 176, 774–785, 10.2353/ajpath.2010.090634 (2010).
Hardison, S. E., Wozniak, K. L., Kolls, J. K. & Wormley, F. L. Jr. Interleukin-17 is not required for classical macrophage activation in a pulmonary mouse model of Cryptococcus neoformans infection. Infect Immun 78, 5341–5351, 10.1128/IAI.00845-10 (2010).
de Souza Silva, C. et al. The Effects of Paracoccidioides brasiliensis Infection on GM-CSF- and M-CSF-Induced Mouse Bone Marrow-Derived Macrophage from Resistant and Susceptible Mice Strains. Mediators Inflamm 2015, 605450, 10.1155/2015/605450 (2015).
Feriotti, C., Loures, F. V., Frank de Araujo, E., da Costa, T. A. & Calich, V. L. Mannosyl-recognizing receptors induce an M1-like phenotype in macrophages of susceptible mice but an M2-like phenotype in mice resistant to a fungal infection. PLoS One 8, e54845, 10.1371/journal.pone.0054845 (2013).
Pina, A., Bernardino, S. & Calich, V. L. Alveolar macrophages from susceptible mice are more competent than those of resistant mice to control initial Paracoccidioides brasiliensis infection. J Leukoc Biol 83, 1088–1099, 10.1189/jlb.1107738 (2008).
Alegre-Maller, A. C. et al. Therapeutic administration of recombinant Paracoccin confers protection against paracoccidioides brasiliensis infection: involvement of TLRs. PLoS Negl Trop Dis 8, e3317, 10.1371/journal.pntd.0003317 (2014).
Freitas, M. S. et al. Paracoccin Induces M1 Polarization of Macrophages via Interaction with TLR4. Front Microbiol 7, 1003, 10.3389/fmicb.2016.01003 (2016).
Zheng, X. F. et al. Lipopolysaccharide-induced M2 to M1 macrophage transformation for IL-12p70 production is blocked by Candida albicans mediated up-regulation of EBI3 expression. PLoS One 8, e63967, 10.1371/journal.pone.0063967 (2013).
Green, L. C. et al. Analysis of nitrate, nitrite, and [15N]nitrate in biological fluids. Anal Biochem 126, 131–138 (1982).
Loures, F. V. et al. MyD88 signaling is required for efficient innate and adaptive immune responses to Paracoccidioides brasiliensis infection. Infect Immun 79, 2470–2480, 10.1128/IAI.00375-10 (2011).
Alegre, A. C., Oliveira, A. F., Dos Reis Almeida, F. B., Roque-Barreira, M. C. & Hanna, E. S. Recombinant paracoccin reproduces the biological properties of the native protein and induces protective Th1 immunity against Paracoccidioides brasiliensis infection. PLoS Negl Trop Dis 8, e2788, 10.1371/journal.pntd.0002788 (2014).
Acknowledgements
This study was supported by the Fundação de Amparo à Pesquisa do Estado de São Paulo (Grant numbers 2013/04088-0; 2013/10741-8; 2016/04877-2; 2016/03322-7).
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: T.A.S. and F.A. Performed the experiments: T.A.S. and F.A. Analyzed the data: T.A.S., M.C.R.-B., A.C. and F.A. Wrote the paper: T.A.S., M.C.R.-B., A.C. and F.A. All authors have read and approved the final manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
da Silva, T., Roque-Barreira, M., Casadevall, A. et al. Extracellular vesicles from Paracoccidioides brasiliensis induced M1 polarization in vitro. Sci Rep 6, 35867 (2016). https://doi.org/10.1038/srep35867
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep35867
This article is cited by
-
Yeast strains isolated from fermented beverage produce extracellular vesicles with anti-inflammatory effects
Scientific Reports (2024)
-
Characteristics and potential clinical applications of the extracellular vesicles of human pathogenic Fungi
BMC Microbiology (2023)
-
Extracellular Vesicles From Sporothrix brasiliensis Yeast Cells Increases Fungicidal Activity in Macrophages
Mycopathologia (2021)
-
Extracellular vesicles carry cellulases in the industrial fungus Trichoderma reesei
Biotechnology for Biofuels (2019)
-
Extracellular vesicles secreted by Saccharomyces cerevisiae are involved in cell wall remodelling
Communications Biology (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.