Abstract
Association between dietary intake of vegetables and fruits and risk of hip fracture has been reported for many years. However, the findings remain inconclusive. We conducted a meta-analysis to evaluate the relationship between intake of vegetables and fruits and risk of hip fracture. Literature search for relevant studies was performed on PubMed and Embase databases. Five observational studies were included in the meta-analysis. Summary hazard ratio (HR) with corresponding 95% confidence interval (CI) was calculated from pooled data using the random-effects model irrespective of heterogeneity. Sensitivity and subgroup analysis were performed to explore possible reasons for heterogeneity. The summary HR for hip fracture in relation to high intake vs. low intake of only vegetables, only fruits and combined intake of fruits and vegetables, was 0.75 (95% CI, 0.61–0.92), 0.87 (95% CI, 0.74–1.04) and 0.79 (95% CI, 0.61–1.03), respectively. Subgroup analyses based on study design, geographical location, number of cases and gender showed similar results. Increased intake of vegetables, but not fruits, was found to be associated with a lower risk of hip fracture. Large prospective clinical trials with robust methodology are required to confirm our findings.
Similar content being viewed by others
Introduction
Osteoporosis and osteoporotic fractures account for a considerable proportion of disability, morbidity and mortality worldwide, especially in the elderly population, which imposes a significant social and economic burden1,2. Of all fractures, the hip fracture is a major and growing public health problem, especially among the elderly. An estimated 1.6 million hip fractures occurred worldwide in the year 20003. The number of people sustaining a hip fracture is expected to rise to 6.3 million by the year 2050 because of an increasing aging population4. Understanding the risk factors for and the underlying mechanisms of hip fracture would help to develop preventive strategies against osteoporotic fracture.
The etiopathogenesis of hip fracture is complex5. Osteoporosis, one of the major risk factors for hip fracture, is characterized by low bone mass and deterioration of bone tissue. A growing body of evidence implicates lifestyle factors as being among the key determinants of the development of osteoporosis6. Among the various lifestyle factors, diet is considered a critical modifiable factor that affects bone health7. Available evidence from cross sectional studies suggests a correlation of high dietary intake of vegetables and fruits with increased bone mineral density (BMD)8,9 and with lower longitudinal BMD loss in men10 and premenopausal women11. Results from observational studies that examined the association between dietary intake of vegetables and fruits and risk of hip fracture, have often been contradictory. While some studies have suggested an inverse association between vegetables and fruits intake and incidence of hip fractures12,13,14 and reduced risk of hip fracture only among elderly Chinese men but not women15, others found no evidence of such an association16,17 and, or even a positive association18. We conducted a meta-analysis to confirm the hypothesis that higher intake of vegetables and fruits is associated with decreased risk of hip fracture.
Results
Literature search and study characteristics and quality
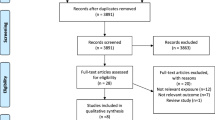
Figure 1 shows the flow diagram of the literature search. On initial search, 271 records were retrieved. After excluding the duplicate publications (N = 44), titles and abstracts of the remaining 227 articles were screened and 213 articles excluded. The remaining 14 articles were full-text reviewed for further assessment. We further excluded three articles19,20,21 due to duplicate publications from the same study population. Three studies were excluded because they evaluated the association between dietary patterns and risk of hip fracture17,22,23. One study was excluded because it reported on the association between diet quality and risk of hip fracture24. Another study was excluded as it assessed the association between combined intake of animal and vegetable diet and hip fracture risk25. One study was excluded because it reported the association of dietary intake of deep-colored vegetables with the prevalence of osteoporosis fracture in postmenopausal Taiwanese women16. Finally, five articles qualified the criteria for inclusion in the meta-analysis (Fig. 1).
The descriptive data for all included studies are summarized in Tables 1, 2. The five studies included one case-control study13 and four cohort studies12,14,15,18, with a combined subject population of 330,417 participants and a total of 6,779 hip fractures came within the purview of our meta-analysis. Of the five studies, 3 were from Europe12,14,18 and 2 from China13,15. All studies separately reported data by intake of fruits or vegetables12,13,14,15,18, while in two studies the combined intake of fruit and vegetable intake was examined12,13. The mean duration of follow-up ranged from 4 to 14.2 years. In all the studies, sub-group analyses adjusted for conventional risk factors for hip fracture, such as age, gender, alcohol intake, total energy intake, physical activity and smoking, were reported.
As shown in the Table 2, the quality scores ranged from 6 to 8 (mean: 7.2).
Combined intake of fruits and vegetables and the risk of hip fracture
Eight studies from five articles were included in the analysis of combined intake of fruits and vegetables and the risk hip fracture. Pooled results indicated no association between combined intake of fruits and vegetables and the risk of hip fracture (OR: 0.83, 95% CI, 0.70–0.98; P = 0.028). However, significant heterogeneity was observed between the studies (I2 = 84.7%, heterogeneity P = 0.000) (Fig. 2). Sensitivity analysis showed unstable results, which ranged from 0.76 (95% CI, 0.65–0.90) with significant heterogeneity (I2 = 85.9%, heterogeneity P = 0.000) (excluding the study by Feart et al.18) to 0.88 (95%CI, 0.78–1.01) with significant heterogeneity (I2 = 73.5%, heterogeneity P = 0.001) (excluding the study by Xie et al.13). On subgroup analyses stratified by geographic location, study design, gender and number of cases, similar results were revealed (Table 3). The power of 63.23% was determined to detect an HR of 0.83 for the highest combined intake of fruits and vegetables intake compared with the lowest combined intake of fruits and vegetables intake.
Intake of fruits and the risk of hip fracture
Six studies from five articles investigated the association between intake of fruits and risk hip fracture. The summary HR for highest versus lowest levels was 0.87 (95% CI: 0.74–1.04; P = 0.119) using the random-effects model, with a high heterogeneity (I2 = 73.0%, P = 0.002, Fig. 3). In sensitivity analysis, the unstable results was observed, which ranged from 0.84 (95%CI: 0.72–0.97) with notable heterogeneity (I2 = 66.8%, heterogeneity P = 0.017) (excluding the study by Feart et al.18) to 0.91 (0.77–1.07) with significant heterogeneity (I2 = 73.0%, heterogeneity P = 0.005) (excluding the study by Xie et al.13). Further, the subgroup analysis was also performed (Table 3). The power of 83.48% was determined to detect an HR of 0.87 for highest versus lowest category of total fruits intake.
Intake of vegetables and the risk of hip fracture
Six studies from five articles examined the association between intake of vegetables and the risk of hip fracture. The summary HR for highest versus lowest levels was 0.75 (95% CI: 0.61–0.92; P = 0.005) using a random-effects model, with a high heterogeneity (I2 = 79.6; P = 0.000, Fig. 4). Sensitivity analysis showed that the overall pooled estimate did not alter substantially with the exclusion of any one study. The overall combined OR after sequential exclusion of one study at a time ranged from 0.70 (95% CI, 0.57–0.86) with significant heterogeneity (I2 = 80.1, heterogeneity P = 0.000) (excluding the study by Feart et al.18) to 0.80 (95% CI, 0.68–0.96) with significant heterogeneity (I2 = 71.1, heterogeneity P = 0.008) (excluding the study by Xie et al.13). Further, the subgroup analysis was also performed (Table 3). The power of 98.34% was determined to detect an HR of 0.75 for highest versus lowest category of total vegetables intake.
Discussion
Clinical practice recommends a daily intake of at least 5 servings of fruits and vegetables26. A higher intake of fruits and vegetables has been shown to reduce the risk of type 2 diabetes27, prolong life28, increase BMD8,9, decrease cardiovascular risk29 and risk of cancer30,31,32. Recently, evidence from multiple observational studies has shown the association between intake of fruits and vegetables and risk of hip fracture12,13,14,15,16,17,18. However, these studies have had a modest sample size and the strength of the association was variable among these studies, with HR varying from 0.06 (95% CI: 0.01–0.38) to 1.95 (95% CI, 1.04–3.66), with results across the studies being inconsistent. In case-control studies, higher consumption of fruits and vegetables was shown to be associated with a reduced risk of hip fracture among Chinese men and women13 and lower forearm fracture among postmenopausal women33. Adherence to a Mediterranean diet, rich in fruits and vegetables was found to be associated with lower risk of hip fracture in a cohort study18; while another cohort study suggested a higher risk of hip fracture14. At present, it is still unclear whether higher intake of fruits and vegetables is associated with lower risk of hip fracture. Therefore, we conducted a comprehensive meta-analysis to assess the association between the intake of fruits and vegetables and the risk of hip fracture. The present meta-analysis found that increased intake of vegetables, but not fruits, was inversely associated with the risk of hip fracture. Inferences drawn from pooled analysis tend to be more reliable than that from a single study as the overall HR is based on a large sample size and has an adequate statistical power. The power of the estimate of combined intake of vegetables and fruits, fruits and vegetables with risk of hip fracture was 63.23%, 83.48% and 98.43%, respectively. Subgroup and sensitivity analyses revealed similar results, which serves to further strengthen the inferences drawn.
Several biological mechanisms may underlie the inverse association found in the meta-analysis. The fruits and vegetables are abundant in alkaline ions (potassium, magnesium and calcium). Calcium is a key element required to maintain bone health. The association of potassium and magnesium with bone health is well-documented34,35. The high vitamin K content in fruits and vegetables may help explain their role in maintaining bone health36. Further, fruits and vegetables are rich source of antioxidants (e.g., vitamin C, carotene and carotenoids), which by countering age-related oxidative stress and inflammation, may increase osteoclastogenesis and osteoclastic differentiation or suppress osteoblastic differentiation37. Furthermore, diets high in fruits and vegetables intake have lower dietary acid load38, which is known to inhibit osteoblast function and increase osteoclast activity resulting in reduced bone formation and increased bone resorption39. Finally, other nutrients such as polyphenols, tocopherols, tocotrienols and glutathione, may potentially contribute in reducing the risk of hip fracture40. However, evidence from animal and experimental studies suggests that reactive oxygen species (ROS), primarily derived from fruits and vegetables, may increase osteoclastogenesis41 and osteoclastic differentiation42, or inhibit osteoblastic differentiation43. Therefore, increased oxidative stress may play an important role in age-related bone loss that leads to osteoporotic fractures44. The preventive effect derived from the fruits and vegetables intake may counteract the adverse effect of ROS in turnover.
To the best of our knowledge this meta-analysis is the first to investigate the association between intake of fruits and vegetables and the risk of hip fracture. The large sample size and a longer time span serve to enhance the statistical power to detect possible associations. The power of HR value of intake of only fruits and only vegetables with risk of hip fracture was 83.48% and 98.43%. Moreover, the use of multivariable-adjusted risk estimates minimized the confounding factors.
However, the potential limitations of this meta-analysis ought to be taken into account while interpreting the results. First, we cannot exclude the possibility that the observed inverse association between intake of vegetables and hip fracture risk could be owe to unmeasured or residual confounding. Further, though the meta-analysis involved a large number of participants, none of the included studies were interventional studies. Third, although we chose the highest multivariable adjusted effect estimates in our meta-analysis, we cannot rule out the effect of uncontrolled confounding by imprecise quantification of the dietary intake of fruits and vegetables. Fourth, a significant heterogeneity was detected among the studies. We further performed sensitivity and subgroup analyses to determine the sources of heterogeneity. The observed heterogeneity could partly be explained by study design (case-control studies and cohort studies) and the article18 reported the positive association. The statistical power of this French study (only included 57 incident hip fracture) was considerable lower, the positive association in the small number of cohort study could be observed by chance, which could be explained the high heterogeneity. In addition, the high heterogeneity observed in the case-control studies may be due in part to the high likelihood of recall and selection or memory bias and to the differential misclassification of exposure. Furthermore, unstable results were observed in subgroup and sensitivity analyses, which indicated that more relevant articles are needed to further explore this association. Fifth, the diet assessment methods and exposure ranges were different across the included studies, which may have contributed to the heterogeneity. Sixth, because the number of included studies were less than 10, we could not examine the publication bias, the influence of the results should not be ignored.
In summary, our results showed that intake of vegetables, but not fruits, may be associated with a lower risk of hip fracture. However, prospective studies need to be conducted to confirm the findings of this meta-analysis.
Materials and Methods
Literature search
A comprehensive literature search for relevant studies published up to May 2015 was performed in PubMed and EMBASE databases. The following search terms were used without imposing any limitation: “fruit(s)” or “vegetable(s)” or “brassicaceae” or “cruciferae” or “citrous” or “citrus”, combined with “hip fracture(s)”. The reference lists in the retrieved publications were manually screened to increase the yield of relevant studies.
Study selection
Studies were considered eligible for inclusion if they met the following criteria: 1) study design: either cohort, case control or cross-sectional; 2) the exposure variable was fruit and/or vegetable consumption; 3) study outcomes included hip fracture risk; 4) Hazard ratio (HR)/Relative risk (RR) and Odds ratio (OR) (95% Confidence interval (CI) reported (or data to calculate these were available). The exclusion criteria were editorial letters, historical reviews and descriptive studies, such as case reports and case series, or laboratory studies. When multiple publications covered the same study population, only the study with the larger sample size was included. Two authors (JKS and HXY) independently performed the literature search and reviewed all studies for their eligibility for inclusion in the meta-analysis. Any disagreements were resolved by consensus or after consultation with the third author (GLH).
Data extraction and assessment of methodological quality
Data pertaining to the following variables were independently extracted for each study by two authors (JKS and HXY) using a standardized data extraction form: first author’s surname, publication year, study design, country, number of subjects (cases/participants), gender, exposure type, methodology for dietary assessment and covariates included in the multivariable model. Disagreements were resolved by discussion and a consensus reached by involving the third author (GLH), if necessary.
The methodological quality of the included studies was evaluated using the Newcastle-Ottawa scale (NOS)45, which contained 9 items for case-control and cohort studies, with every item having a score of 1 point. Studies with a total score of >6 were deemed to be of high quality.
Statistical analysis
Hazard ratio with 95% CI was the common measure across all eligible studies. Since hip fracture is a relatively rare event, the differences among risk estimates (HR, RR and OR) were ignored and the OR and RR were directly converted into HR. A random-effects model of DerSimonian and Laird was used to calculate summary HR, comparing the highest across all included studies regardless of heterogeneity46, which incorporates both intra- and inter-study variability. If a study did not report the total HR for combined intake of vegetables and fruits, but instead reported the HR for only vegetables and only fruits separately in a study, they were considered separately as if obtained from different studies and used the effect estimate for that study in the meta-analysis of combined vegetables and fruits intake and hip fracture risk. If gender-specific estimates were available, they were also regarded as two different studies. Power analysis was performed using the method described by Cafri et al.47.
Sensitivity analysis was performed to evaluate robustness and stability of the results by sequentially omitting one study on each turn. Moreover, subgroup analysis was performed to assess heterogeneity and assess the influence of different inclusion criteria on the overall estimate.
Additional Information
How to cite this article: Luo, S. et al. Increased intake of vegetables, but not fruits, may be associated with reduced risk of hip fracture: A meta-analysis. Sci. Rep. 6, 19783; doi: 10.1038/srep19783 (2016).
References
Burge, R. et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res 22, 465–475 (2007).
Cooper, C., Atkinson, E. J., Jacobsen, S. J., O’Fallon, W. M. & Melton, L. J. 3rd Population-based study of survival after osteoporotic fractures. Am J Epidemiol 137, 1001–1005 (1993).
Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Organ Tech Rep Ser843, 1–129 (1994).
Cooper, C., Campion, G. & Melton, L. J. 3rd Hip fractures in the elderly: a world-wide projection. Osteoporos Int 2, 285–289 (1992).
Cummings, S. R. & Melton, L. J. Epidemiology and outcomes of osteoporotic fractures. Lancet 359, 1761–1767 (2002).
D’Amelio, P., Tamone, C., Pluviano, F., Di Stefano, M. & Isaia, G. Effects of lifestyle and risk factors on bone mineral density in a cohort of Italian women: suggestion for a new decision rule. Calcif Tissue Int 77, 72–78 (2005).
Cashman, K. D. Diet, nutrition and bone health. J Nutr 137, 2507S–2512S (2007).
Zalloua, P. A. et al. Impact of seafood and fruit consumption on bone mineral density. Maturitas 56, 1–11 (2007).
Prynne, C. J. et al. Fruit and vegetable intakes and bone mineral status: a cross sectional study in 5 age and sex cohorts. Am J Clin Nutr 83, 1420–1428 (2006).
Tucker, K. L. et al. Potassium, magnesium and fruit and vegetable intakes are associated with greater bone mineral density in elderly men and women. Am J Clin Nutr 69, 727–736 (1999).
Xu, L. et al. Food groups and risk of forearm fractures in postmenopausal women in Chengdu, China. Climacteric 12, 222–229 (2009).
Byberg, L., Bellavia, A., Orsini, N., Wolk, A. & Michaelsson, K. Fruit and vegetable intake and risk of hip fracture: a cohort study of Swedish men and women. J Bone Miner Res 30, 976–984 (2015).
Xie, H. L. et al. Greater intake of fruit and vegetables is associated with a lower risk of osteoporotic hip fractures in elderly Chinese: a 1:1 matched case-control study. Osteoporos Int 24, 2827–2836 (2013).
Benetou, V. et al. Mediterranean diet and incidence of hip fractures in a European cohort. Osteoporos Int 24, 1587–1598 (2013).
Dai, Z. et al. Protective effects of dietary carotenoids on risk of hip fracture in men: the Singapore Chinese Health Study. J Bone Miner Res 29, 408–417 (2014).
Lin, C. H. et al. Insufficient deep-colored vegetable intake is associated with higher fragility fracture rate in postmenopausal Taiwanese women. International Journal of Gerontology 7, 75–79 (2013).
McTiernan, A. et al. Low-fat, increased fruit, vegetable and grain dietary pattern, fractures and bone mineral density: the Women’s Health Initiative Dietary Modification Trial. Am J Clin Nutr 89, 1864–1876 (2009).
Feart, C. et al. Adherence to a Mediterranean diet and risk of fractures in French older persons. Osteoporos Int 24, 3031–3041 (2013).
Benetou, V. et al. Diet and hip fractures among elderly Europeans in the EPIC cohort. Eur J Clin Nutr 65, 132–139 (2011).
Dai, Z. et al. Adherence to a vegetable-fruit-soy dietary pattern or the Alternative Healthy Eating Index is associated with lower hip fracture risk among Singapore Chinese. J Nutr 144, 511–518 (2014).
Zeng, F. F. et al. Dietary patterns and the risk of hip fractures in elderly Chinese: a matched case-control study. J Clin Endocrinol Metab 98, 2347–2355 (2013).
Fung, T. T. & Feskanich, D. Dietary patterns and risk of hip fractures in postmenopausal women and men over 50 years. Osteoporos Int 26, 1825–1830 (2015).
Samieri, C. et al. Nutrient patterns and risk of fracture in older subjects: results from the Three-City Study. Osteoporos Int 24, 1295–1305 (2013).
Zeng, F. F. et al. Diet-quality scores and risk of hip fractures in elderly urban Chinese in Guangdong, China: a case-control study. Osteoporos Int 25, 2131–2141 (2014).
Frassetto, L. A., Todd, K. M., Morris, R. C. Jr. & Sebastian, A. Worldwide incidence of hip fracture in elderly women: relation to consumption of animal and vegetable foods. J Gerontol A Biol Sci Med Sci 55, M585–592 (2000).
Kushi, L. H. et al. American Cancer Society Guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin 62, 30–67 (2012).
Wu, Y., Zhang, D., Jiang, X. & Jiang, W. Fruit and vegetable consumption and risk of type 2 diabetes mellitus: a dose-response meta-analysis of prospective cohort studies. Nutr Metab Cardiovasc Dis 25, 140–147 (2015).
Bellavia, A., Larsson, S. C., Bottai, M., Wolk, A. & Orsini, N. Fruit and vegetable consumption and all-cause mortality: a dose-response analysis. Am J Clin Nutr 98, 454–459 (2013).
Wang, X. et al. Fruit and vegetable consumption and mortality from all causes, cardiovascular disease and cancer: systematic review and dose-response meta-analysis of prospective cohort studies. BMJ 349, g4490 (2014).
Aune, D. et al. Nonlinear reduction in risk for colorectal cancer by fruit and vegetable intake based on meta-analysis of prospective studies. Gastroenterology 141, 106–118 (2011).
Bamia, C. et al. Fruit and vegetable consumption in relation to hepatocellular carcinoma in a multi-centre, European cohort study. Br J Cancer 112, 1273–1282 (2015).
Xu, C. et al. Fruits and vegetables intake and risk of bladder cancer: a PRISMA-compliant systematic review and dose-response meta-analysis of prospective cohort studies. Medicine (Baltimore) 94, e759 (2015).
Xu, L. et al. Diet, activity and other lifestyle risk factors for forearm fracture in postmenopausal women in China: a case-control study. Menopause 13, 102–110 (2006).
Jehle, S., Hulter, H. N. & Krapf, R. Effect of potassium citrate on bone density, microarchitecture and fracture risk in healthy older adults without osteoporosis: a randomized controlled trial. J Clin Endocrinol Metab 98, 207–217 (2013).
Carpenter, T. O. et al. A randomized controlled study of effects of dietary magnesium oxide supplementation on bone mineral content in healthy girls. J Clin Endocrinol Metab 91, 4866–4872 (2006).
Iwamoto, J., Sato, Y., Takeda, T. & Matsumoto, H. High-dose vitamin K supplementation reduces fracture incidence in postmenopausal women: a review of the literature. Nutr Res 29, 221–228 (2009).
Aruoma, O. I., Grootveld, M. & Bahorun, T. Free radicals in biology and medicine: from inflammation to biotechnology. Biofactors 27, 1–3 (2006).
New, S. A. Intake of fruit and vegetables: implications for bone health. Proc Nutr Soc 62, 889–899 (2003).
Brandao-Burch, A., Utting, J. C., Orriss, I. R. & Arnett, T. R. Acidosis inhibits bone formation by osteoblasts in vitro by preventing mineralization. Calcif Tissue Int 77, 167–174 (2005).
Bu, S. Y., Hunt, T. S. & Smith, B. J. Dried plum polyphenols attenuate the detrimental effects of TNF-alpha on osteoblast function coincident with up-regulation of Runx2, Osterix and IGF-I. J Nutr Biochem 20, 35–44 (2009).
Lee, N. K. et al. A crucial role for reactive oxygen species in RANKL-induced osteoclast differentiation. Blood 106, 852–859 (2005).
Bai, X. C. et al. Reactive oxygen species stimulates receptor activator of NF-kappaB ligand expression in osteoblast. J Biol Chem 280, 17497–17506 (2005).
Li, X. et al. Aluminum induces osteoblast apoptosis through the oxidative stress-mediated JNK signaling pathway. Biol Trace Elem Res 150, 502–508 (2012).
Manolagas, S. C. From estrogen-centric to aging and oxidative stress: a revised perspective of the pathogenesis of osteoporosis. Endocr Rev 31, 266–300 (2010).
Hartling, L. et al. Testing the Newcastle Ottawa Scale showed low reliability between individual reviewers. J Clin Epidemiol 66, 982–993 (2013).
DerSimonian, R. & Laird, N. Meta-analysis in clinical trials. Control Clin Trials 7, 177–188 (1986).
Cafri, G., Kromrey, J. D. & Brannick, M. T. A SAS macro for statistical power calculations in meta-analysis. Behav Res Methods 41, 35–46 (2009).
Author information
Authors and Affiliations
Contributions
J.K.S., G.L.H., X.H.Y. and S.Y.L. wrote the main manuscript text; J.K.S., G.L.H., X.H.Y., D.R.L., K.Z. and H.L. prepared Figures 1–4; J.K.S., G.L.H. and Y.L contributed reagents/materials/analysis tools; All authors reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Luo, S., Li, Y., Luo, H. et al. Increased intake of vegetables, but not fruits, may be associated with reduced risk of hip fracture: A meta-analysis. Sci Rep 6, 19783 (2016). https://doi.org/10.1038/srep19783
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep19783
This article is cited by
-
Risk of hip fracture in meat-eaters, pescatarians, and vegetarians: results from the UK Women’s Cohort Study
BMC Medicine (2022)
-
Association between dietary inflammatory index and bone density in lactating women at 6 months postpartum: a longitudinal study
BMC Public Health (2019)
-
Fruit and vegetable consumption and its contribution to inequalities in life expectancy and disability-free life expectancy in ten European countries
International Journal of Public Health (2019)
-
Benefits and safety of dietary protein for bone health—an expert consensus paper endorsed by the European Society for Clinical and Economical Aspects of Osteopororosis, Osteoarthritis, and Musculoskeletal Diseases and by the International Osteoporosis Foundation
Osteoporosis International (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.