Abstract
Micronutrient deficiency is common in patients with HIV/AIDS, usually caused by mal-absorption and/or drug interactions. 25-hydroxyvitamin D is of fundamental importance for the homeostasis of musculoskeletal health. The current study aimed to evaluate the nutritional status of HIV-infected subjects in order to make their nutritional diagnoses, including their vitamin D blood levels and to estimate their consumption of vitamin D. The study included 98 HIV-1-infected subjects, followed at University of São Paulo Medical School - HC-FMUSP. We performed a nutritional evaluation, along with the determination of patients’ serum 25-hydroxyvitamin D and calcium concentration, biochemical analyses and an anthropometric assessment. In the medical interview a 24-hour food recall was used (R24) to estimate daily calorie intake, macronutrients, calcium and vitamin D. A high level of vitamin D deficiency was observed in our patients: 83.4% of them had levels below 30 ng/ml; they also presented an increased risk of cardiovascular disease, along with a high consumption of dietary fat. Factors related to the virus itself and to the use of antiretroviral drugs may have contributed for the low vitamin D levels seen in our HIV-1-infected patients.
Similar content being viewed by others
Introduction
HIV-infected patients on highly active antiretroviral therapy (HAART) have an increased risk for several complications not directly related to AIDS, many of them more common in aging patients1,2, such as cardiovascular disease, cancer, kidney and bone disease3. There is a decrease in bone mineralization in a large proportion of patients, resulting from various factors from the host itself, the virus and the use of HAART. Appropriate nutritional status is a prerequisite for improving the quality of life of these patients4.
Micronutrient deficiency is common in HIV/AIDS patients, caused by mal-absorption, drug interactions, metabolic changes and loss of fluids from vomiting and diarrhea. Vitamins and minerals are considered essential to maintaining health, as they protect against opportunistic infections and favor the body’s proper functioning, particularly that of the immune system5. Vitamin D is of fundamental importance for the homeostasis of calcium and phosphorus and for musculoskeletal health6,7,8. Furthermore, vitamin D deficiency causes an increase in parathyroid hormone (PTH), which in turn increases insulin resistance, leading to hypertension, inflammation and increased cardiovascular risk9.
The usual daily intake of vitamin D varies between 5–10 mg; it can be found in foods such as fish oil, egg yolk and milk10. An adequate consumption of calcium and vitamin D from food and/or supplements is necessary to achieve a normal bone mineral density (BMD), in order to decrease the rate of bone loss in the elderly10. The current study aimed to evaluate the nutritional status of HIV-infected subjects followed in a Sao Paulo, Brazil university hospital, in order to make their nutritional diagnoses, including their vitamin D blood levels and to estimate their vitamin D consumption.
Material and Methods
We have been following HIV-positive patients in our outpatient service for 29 years. For the purpose of this study, from a total of 500 HIV-1 subjects we currently follow, a subset of 98 were invited and accepted to participate. In this convenience sample, patients were included if they were more than 18 years old and were in active follow-up during the period ranging from August 2011 to December 2013. After signing an informed consent form, patients answered a questionnaire containing information on their socio-behavioral characteristics.
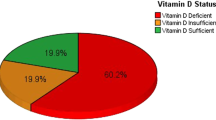
A detailed nutritional evaluation was performed, along with the determination of 25-hydroxyvitamin D, calcium, cholesterol and its fractions, triglycerides and glucose blood levels, in order to make a nutritional diagnosis and to estimate patients consumption of vitamin D. Vitamin D levels were classified according to the American Society of Endocrinology as: <10 ng/ml – deficiency; 10–30 ng/ml – insufficiency; and >30 ng/ml – sufficiency. Sun exposure was considered adequate if legs and/or arms were exposed to sunlight for at least 20 minutes every day.
Anthropometric assessment consisted of measuring the triceps, biceps, sub-scapular, axillary, calf average and mid-thigh skin folds, the arm and waist circumferences and body weight and height11. In the medical interview a 24-hour food recall was used (R24), in order to estimate the daily caloric intake, macronutrients, calcium and vitamin D. Questionnaires also included questions about cardiovascular risk factors, such as smoking.
Descriptive statistics were performed with the statistics program SPSS 20.0 and displayed in tables showing frequencies and percentages. Statistical analysis was conducted using Student’s t-test for parametric data and the chi-square test for proportions. Possible differences in patient characteristics or laboratory values among groups were evaluated with two-way Mann-Whitney’s test and Kruskal-Wallis test. The study was approved by the ethical board of Hospital das Clínicas, FMUSP (CAPPesq no 0532/11) and all procedures were done in accordance with approved guidelines.
Results
Mean age was 39 years for the 66 men (67.4%) and 41.7 years for the 32 (32.6%) women. Mean duration of HIV infection was 6.31 years for men and 7.31 for women; smokers represented 22.6% of the sample and most were on HAART (Table 1). Table 1 also shows the blood levels of 25-hydroxyvitamin D and ionic calcium: 21 (66%) of women and 49 (72%) of men presented deficient levels of vitamin D. Similar results were obtained for the consumption of vitamin D, since 26 (81%) of women and 57 (87%) of men did not consume enough daily amounts of foods rich in vitamin D. Ionic calcium levels were normal for 23 (72%) women and 48 (73%) men, respectively.
Table 2 shows the risk factors associated with vitamin D deficiency, classified by gender. Fourteen (43.7%) and 34 (51.5%) of women and men, respectively, reported a minimum sun exposure of 15 minutes on their arms and legs daily. Twenty-six (81.2%) women and 45 (68.2%) men were former or current smokers. One third of the men did consume alcohol three times a week, although no further detailed intake information was obtained. Nine (9.4%) and 18 (27.3%) women and men, respectively, were not on HAART and 70% of the patients had undetectable viral loads in their blood.
Table 3 presents a nutritional and self-image evaluation of the patients; 20 (63%) women and 33 (50%) men were overweight or obese (p = 0.04). Abdominal circumference, as a measure of cardiovascular risk, was elevated for 23 (72%) women and 29 (53%) men. A self-image evaluation revealed that 16 women and almost 70% of the men did not notice any differences in their appearances. No significant differences were observed for the variables age over 50 years-old, T CD4 cells count, level of HIV viremia, cardiovascular risk, smoking habits, alcohol consumption and BMI; the exception was daily sun exposure (p = 0.009) (Table 4).
Discussion
A high level of 25-hydroxyvitamin D deficiency and insufficiency was observed in our patients since 83.4% of them had levels below 30 ng/ml. A recent report showed a 23% prevalence of vitamin D deficiency in HIV Brazilian patients12. In the United States, a study revealed vitamin D deficiency in 74.4% of HIV-positive adults10. Taken together, these studies are in accordance with recent epidemiological studies, which pointed to a worldwide occurrence of vitamin D deficiency7,13,14.
In addition to the findings described above other factors related to HIV itself and to the use of antiretroviral drugs can be considered as contributing causes for low vitamin D blood levels15,16,17. We found a low intake of vitamin D, maybe because its natural occurrence in food is small and supplementation of food with this vitamin is not done for the general population18,19. Vitamin D supplementation with 600–800 UL/day was not enough to normalize the levels of the vitamin in African American and Latin American HIV-infected patients and to achieve that goal an intake of 1000 to 2000 UL/day would have been required. Studies involving a larger number of subjects are needed to assess the impact of vitamin D supplementation on the co-morbidities of adults with HIV infection20.
The major finding of this study was the high frequency (>80%) of insufficient levels of vitamin D, as well as a high consumption of dietary fat, along with a sizable proportion of overweight and obese patients21. Thus, nutritional intervention is necessary, possibly including supplementation of vitamin D. There are several causes for the high prevalence of vitamin D insufficiency, even in low-latitude regions. The synthesis of vitamin D is proportional to the area exposed to sunlight and is influenced by environmental factors such as latitude, season, time of day, amount of clouds or the ozone layer and factors related to the individuals and their habits22,23. Persons with more melanin in their skin synthesize less pro-vitamin D for the same dose of UV-B. Sunscreen use is another factor impairing the ability to synthesize vitamin D, a correct use of sunscreen with SPF 8 or 15 reducing the synthesis of vitamin D from 95% to 99.9%, respectively7.
More than 98% of our patients did not consume the optimum amount of calcium. A study in the Southern Brazil city of Porto Alegre demonstrated that 95% of children and adolescents did not consume the recommended daily amount of calcium, revealing a significant deficit in their calcium supply24. The data from our study in São Paulo confirm that people living with HIV/AIDS have a low calcium intake. The importance of calcium in bone mineralization is worth emphasizing and therefore the low intake of calcium seen in our patients may put them at high risk for fractures. Corroborating this finding, a 60% prevalence of osteopenia or osteoporosis was seen in the original cohort from where our sample was drawn and also observed elsewhere25.
This study has potential confounders since some differences in the distribution of independent variables we found may not be specific to HIV-infected patients, but merely reflect what happens in the population at large.
For example, women’s lower prevalence of smoking, a finding of our study, could be only mirroring the same gender difference in the prevalence of smoking in the population of Sao Paulo city.
Concluding, a high level of vitamin D deficiency or insufficiency was observed in 83.4% of our patients, along with high consumption of dietary fat; the prevalence of overweight was high. Thus, these patients may be at high risk for cardiovascular diseases and bone fractures in the future. Therefore, a multidisciplinary team should care for these subjects aiming at prevention and early treatment of these risk factors.
Additional Information
How to cite this article: Sales, S. H. et al. High frequency of deficient consumption and low blood levels of 25-hydroxyvitamin D in HIV-1-infected adults from São Paulo city, Brazil. Sci. Rep. 5, 12990; doi: 10.1038/srep12990 (2015).
Change history
20 October 2015
A correction has been published and is appended to both the HTML and PDF versions of this paper. The error has been fixed in the paper.
References
WHO Living well with HIV/aids – Manual on nutritional care and support for people living with HIV/aids. WHO 3, 95 (2002).
Ministério da Saúde Programa Nacional de Controle e Prevenção de DST/AIDS. Boletim epidemiológico - AIDS. MS, Secr Vig Sd, Prog Nac Cont e Prev de DST/AIDS 201, 66 (2013).
Deeks, S. G. & Phillips, A. N. HIV infection, antiretroviral treatment, ageing and non –AIDS related morbidity; clinical review. BMJ 338, 186–190 (2009).
Kruzich L. A. M. G., Wilson, C. M. & Stephensen, C. B. HIV-infected US youth are at high risk of obesity and poor diet quality: A challenge for improving short – and long-term health outcomes. J Am Diet Assoc 104, 1554–1560 (2004).
Gautam, N. et al. Role of Multivitamins, Micronutrients and Probiotics Supplementation in Management of HIV Infected Children. Ind J of Ped 81, 1315–20 (2014).
Premaor M. O. F. T. Hipovitaminose D em adultos: entendendo melhor a apresentação de uma velha doença. Arq Bras Endocrinol Metab 50, 25–37 (2006).
Holick, M. F. High prevalence of vitamin D inadequacy and implications for health. Mayo Clinic Proc 81, 353–373 (2006).
Ponda, M. P., McGee, D. & Breslow, J. L. Vitamin D-binding protein levels do not influence the effect of vitamin D repletion on serum PTH and calcium: data from a randomized, controlled trial. JC Clin Endoc and Metab 99, 2494–2499 (2014).
Deckers, M. M. et al. Prevalence of vitamin D deficiency and consequences for PTH reference values. Clin Chim Acta, Int J Cklin Chem 426, 41–45 (2013).
Rodriguez-Martinez, M. A. & Garcia-Cohen, E. C. Role of Ca(2+) and vitamin D in the prevention and treatment of osteoporosis. Pharm &Therap 93, 37–49 (2002).
Van der Sande, M. A. et al. Body mass index at time of HIV diagnosis: a strong and independent predictor of survival. J of Acqui Immune Def Synd 37, 1288–1294 (2004).
Havers, F. et al. 25-Hydroxyvitamin D insufficiency and deficiency is associated with HIV disease progression and virological failure post-antiretroviral therapy initiation in diverse multinational settings. JID 210, 244–253 (2014).
Holick, M. F. Vitamin D deficiency. NEJM 357, 266–281 (2007).
Bandeira, F., Griz, L., Dreyer, P., Eufrazino, C., Bandeira, C. & Freese, E. Vitamin D deficiency: A global perspective. Arq Bras End e Met 50, 640–646 (2006).
Villamor, E. A potential role for vitamin D on HIV infection? Nutrit Ver 64, 226–233 (2006).
Cozzolino, M. et al. HIV-protease inhibitors impair vitamin D bioactivation to 1,25-dihydroxyvitamin D. Aids 17, 513–520 (2003).
Wang, T. J. et al. Vitamin D deficiency and risk of cardiovascular disease. Circ 117, 503–511 (2008).
Holick, M. F. Vitamin D: its role in cancer prevention and treatment. Prog Biop am Mol Bio 92, 49–59 (2006).
Calvo, M. S., Whiting, S. J. & Barton, C. N. Vitamin D intake: a global perspective of current status. J of Nut 35, 310–316 (2005).
Theodorou, M., Serste, T., Van Gossum, M. & Dewit, S. Factors associated with vitamin D deficiency in a population of 2044 HIV-infected patients. Clin Nut 33, 274–279 (2014).
Soares, F. M. & Costa, I. M. Treatment of HIV-associated facial lipoatrophy: impact on infection progression assessed by viral load and CD4 count. An Bras Derm 88, 570–577 (2013).
Vieth, R. What is the optimal vitamin D status for health? Prog Biop am Mol Bio 92, 26–32 (2006).
Webb, A. R. Who, what, where and when-influences on cutaneous vitamin D synthesis. Prog Biop am Mol Bio 92, 17–25 (2006).
Bueno, A. L. & Czepielewski, M. A. The importance for growth of dietary intake of calcium and vitamin D. J Ped 84, 386–394 (2008).
Tedaldi, E. M. et al. Increased body mass index does not alter response to initial highly active antiretroviral therapy in HIV-1-infected patients. J of Acq Imm Def Synd 43, 35–41 (2006).
Acknowledgements
This study was partially funded by Fapesp n. 2011/04868-0 and 2015/12311-6. SHS was the receptor of a CAPES scholarship.
Author information
Authors and Affiliations
Contributions
S.H.S., S.M. and D.C.S. collected the data and wrote the manuscript. L.A.M.F. and T.A.S. made the statistical analysis and revised the final version of the MS. A.J.S.D. and J.C. designed the study and read the final version of the MS.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Sales, S., Matta, S., Silva, D. et al. High frequency of deficient consumption and low blood levels of 25-hydroxyvitamin D in HIV-1-infected adults from São Paulo city, Brazil. Sci Rep 5, 12990 (2015). https://doi.org/10.1038/srep12990
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep12990
This article is cited by
-
Low bone mass and vitamin D in Brazilian people living with HIV under antiretroviral therapy
Archives of Osteoporosis (2022)
-
Contemporary Lifestyle Modification Interventions to Improve Metabolic Comorbidities in HIV
Current HIV/AIDS Reports (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.