Abstract
The awareness, perceptions and experiences of Nigerian Primary Open Angle Glaucoma (POAG) patients were assessed using a hospital based cross-sectional study design. One hundred and twenty POAG patients attending a glaucoma clinic in Lagos Nigeria were recruited consecutively. They underwent face-to-face interviews with trained interviewers using a semi-structured questionnaire and an interview guide consisting of open-ended questions. A comprehensive ocular examination which included static automated perimetry, gonioscopy, stereoscopic optic nerve head assessment and contrast sensitivity was carried out for all participants. Twenty per cent (n = 24) of the respondents did not know they were being managed for a disease called Glaucoma. Age, gender, religion, ethnicity, marital status and occupation did not significantly affect the awareness of glaucoma diagnosis (p > 0.05). Positive family history of glaucoma, educational status and duration of disease were the most significant factors associated with awareness of glaucoma diagnosis (p < 0.05). POAG patients in Nigeria lack the depth of perception that can equip them to educate and motivate their family members to screen for glaucoma. There is an urgent need to develop continuous eye health education programmes to improve their perception and outlook; thereby increasing the uptake of glaucoma screening by first degree relatives of glaucoma patients.
Similar content being viewed by others
Introduction
Glaucoma is the leading cause of irreversible blindness in the world1 and the second leading cause of blindness in Nigeria being responsible for 16.7% of blindness in the Nigerian National Blindness and Visual Impairment Survey (NNBVIS)2. The most common form of glaucoma in Nigeria is POAG3 which is characteristically symptomless in the early stages of the disease. Prompt diagnosis before significant visual loss has occurred, requires the presence of a high level of public awareness about glaucoma and the culture of periodic routine eye checks to increase case detection. These are both absent in Nigeria. Several studies in Nigeria have reported a low level of awareness and knowledge of glaucoma in patients4,5,6 as well as workers in health institutions7,8. Patients with a positive family history of glaucoma have been reported to have a higher level of awareness of the disease than others9,10,11. Onyekwe et al.6 reported that the most frequent source of information to patients about glaucoma was from relatives and friends and not health workers.
Improved awareness and better perception can positively influence the accuracy of the eye health education messages glaucoma patients share and are key to the development of a positive outlook. A positive outlook can motivate patients to ensure that family members undergo glaucoma screening regularly thereby enhancing prompt diagnosis and reducing the risk of blindness from glaucoma. It can also improve adherence and persistence to treatment and follow up in patients.
We therefore sought to assess from patients being managed for POAG their familiarity with the term ‘Glaucoma’ as the name of the eye disease they had, whether they knew it was heritable, if they had informed their families about their diagnosis and whether their first degree relatives had undergone screening for glaucoma. We hoped to elucidate patient characteristics associated with a low level of awareness and poor perception and suggest more effective ways of targeting eye health education messages to reach them.
Results
A total of 120 patients were interviewed. There were 44 (36.7%) males and 76 (63.3%) females with ages ranging from 40 to 79 years. Majority of the respondents were Christians [n = 99 (82.5%)] and married [n = 91 (75.8%)]. Among the respondents, 3 (2.5%) had no formal education, 21(17.5%) had only primary education, 31 (25.8%) had completed secondary education, 42 (35%) had completed tertiary education and 23 (19.2%) had undergone postgraduate studies.
Ninety-six (80%) of the respondents knew they were being managed for an eye disease called ‘Glaucoma’ while 24 (20%) did not. There was no significant difference (p = 0.71) between the mean age of those who were aware of their diagnosis (58.33years, SD 10.59) and those who were not (59.54years, SD 10.29). Table 1 below shows the socio-demographic factors associated with awareness of glaucoma diagnosis. Respondents with at least a primary school education were six times more likely to be aware of their diagnosis than patients with no formal education (OR: 6.2; 95% CI: 1.29 to 29.89; p = 0.023). There was a twofold higher likelihood of awareness of diagnosis when patients with at least a primary education were compared to those with at least a secondary education but this difference was not statistically significant (OR: 2.4; 95% CI: 0.93 to 6.16; p = 0.068).
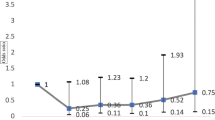
Table 2 compares the clinical features of the group aware of their diagnosis to those that were not aware. Patients aware of their diagnosis had been managed on average for '52.2 months (SD 51.61) while those unaware of their diagnosis had been managed for glaucoma for 29.17 months (SD 30.53) on the average (p = 0.039). The group that was aware of their diagnosis had a larger cup to disc ratio in both eyes compared to those unaware of their diagnosis though their mean and pattern standard deviations did not vary significantly.
59 respondents (49.2%) had a positive family history of glaucoma and were nearly four times more likely to be aware of their diagnosis (unadjusted OR = 3.7, 95% CI: 1.35 to 10.13) than those without a family history of glaucoma. Despite the presence of a positive family history, only 19 (32.2%) of them had family members who had undergone glaucoma screening and 33.9% (n = 20) did not know glaucoma could be heritable.
Of the 96 patients who knew they were being managed for glaucoma, only 21 (21.88%) had good perception; 35 (36.48%) had fair perception and nearly half (n = 40, 41.67%) had poor perception about the disease with over one-third (n = 36, 37.5%) unaware that glaucoma is heritable.
After multiple logistic regression analysis adjusting for confounding variables, a positive family history (p = 0.01), duration of disease (p = 0.03) and educational status (p = 0.03) remained important factors associated with awareness of glaucoma diagnosis. Table 3 shows the multiple regression analysis results.
A hundred and fourteen respondents (95%) were on medical therapy while 6 had had trabeculectomy and were not on any topical medications. 13 respondents had been offered surgical therapy in the course of their management but had declined. Table 4 below lists their reasons for declining. One of them proffered no reason for refusing surgery.
Only 10 (8.77%) of those on medical therapy complained of side effects from their drugs. Table 5 below lists the side effects complained of by the respondents. One of the patients had been switched to a different drug group because of a low pulse rate while on beta blockers and the patient mentioned this as a side effect experienced.
Of the 108 respondents who needed to obtain permission from work to attend clinic visits, 24 (23.7%) had difficulty getting time off work to attend. Nearly half of the 90 respondents (n = 40, 44.4%) who were required to report at work after clinic visits, were not able to do so after an average waiting period of 4 hours in the clinic.
74 respondents (61.67%) were potentially able to drive while 46 (38.33%) did not drive for non-visual reasons. Of these 74, 12 (16.22%) had stopped driving for visual reasons and 62 (83.78%) were still driving. However, nearly a third of those still driving (n = 20, 32.26%) had stopped driving at night for visual reasons.
Discussion
The unacceptably high proportion of patients (17.7%3–24%12) presenting bilaterally blind from glaucoma to hospitals in Nigeria suggests a very low level of awareness about glaucoma in the community. If glaucoma patients are to serve as reliable sources of information to their relatives, there is a need to assess what they perceive glaucoma to be so that the eye health messages they disseminate are accurate and effective. Odberg et al13 reported that there was a lack of knowledge of glaucoma in a large number of their patients in Norway while Gasch et al9 reported that being aware of the fact that one had glaucoma was not a significant determinant of level of awareness about the disease.
Majority of respondents in this study knew they were being managed for a disease called glaucoma but lacked information about the fact that it could be heritable (n = 36, 37.5%); had not informed their families that they had been diagnosed to have glaucoma (n = 29, 30.2%) and had first degree relatives who had not been screened for glaucoma (n = 45, 46.9%). There is a high likelihood that patients unaware of their diagnosis (n = 24) were also unaware of the potential heritability of the disease. If included, it would mean that half of the participants in this study (n = 60, 50%) were not aware of the heritability of glaucoma and the increased risk to their first degree relatives.
These findings suggest that unless urgent action is taken to improve the knowledge of glaucoma patients about the disease and ensure this knowledge is imparted to their relatives, early detection of the disease by targeted screening of at risk population is unlikely to become the norm in Nigeria soon. The proportion of patients who were not aware that glaucoma could be heritable in other studies varies from 21%14 to 68.2%6. Deokule et al15 reported that only 41% of their patients knew that their family members were at increased risk of chronic open angle glaucoma and 45.5% of patients' family members had not been screened for glaucoma.
The key factors related to awareness of glaucoma diagnosis in this study were positive family history of glaucoma, educational status and duration of disease. The proportion of patients in this study with a positive family history of glaucoma was high (49.2%) compared to 15.1%4 and 26.4%16 reported in other Nigerian studies. The reason for this is unclear but may be due to the fact that the average duration of disease in this study was long (47.6 months SD 48.9) with duration ranging from 6 months to 20 years and so over time the respondents would have found out more relatives with glaucoma and more relatives may have developed glaucoma during that period.
Patients with a positive family history of glaucoma (n = 59, 49.2%) were nearly four times more likely to be aware of their diagnosis than those without a positive family history but lacked depth of perception about the disease. This may explain why Adekoya et al16 and Gogate et al17 noted an association between positive family history and late presentation in their studies. POAG patients should be encouraged to inform their families about their diagnosis and the fact that they have a higher risk than the general population of developing the disease over time. They could be asked periodically in the clinic if their relatives are aware of their diagnosis and if they have been screened for glaucoma. Glaucoma clinics could also employ trained counsellors to schedule family counselling sessions to educate first degree relatives who accompany glaucoma patients to the clinic or who want to attend counselling sessions to discuss the disease privately with the counsellor at their convenience.
More educated respondents were more likely to be aware of their diagnosis (Table 1). An earlier study in South-East Nigeria5 had also reported a six fold likelihood of better awareness in those with at least a primary education compared to those with no formal education a was the finding in this study. Other studies have also reported that more educated subjects were more aware than less educated subjects7,9,11,18,19,20.
Age, gender, religion, occupation, marital status, ethnicity did not influence awareness of glaucoma diagnosis in this study (see Table 1). A Nigerian hospital–based study5 had earlier reported that age and gender were not associated with disease knowledge. However a population based study in India11 reported that elderly people and women had better awareness than younger subjects and men. Gasch et al.9 also reported better awareness in subjects aged 50–79 years old. These differences may be accounted for by the fact that the latter two studies were population based studies and the first two were hospital based. Lewallen & Courtright21 suggested that women were more likely to have less access to eye care, to be less educated and to be less aware about eye health. It is possible that because the first two studies were hospital based, the women studied were the more aware, more educated ones who had no problem accessing eye health services. An Ethiopian hospital based study19 and an Indian population based study20 also reported that age, gender and religion did not influence glaucoma awareness in their studies. The reason for the female preponderance in this study is unclear but could suggest a disproportionately higher prevalence of POAG in women in this population. Further epidemiological studies would be needed to confirm this. Also, the cosmopolitan nature of the study location as evidenced by the high level of literacy in the participants may have reduced previously reported gender-related barriers to eye care21 in this study.
The mean duration of disease for the subgroup of respondents that were unaware of their diagnosis in this study was unacceptably long (29.17 months) and suggests that it is possible for medical personnel to take it for granted that over time patients would have acquired some knowledge about the disease they are being managed for. Kim et al22 advocate that repeated patient education is often needed to maintain a useful effect.
The only statistically significant variation in the clinical characteristics of the respondents aware or unaware of their diagnosis was the cup to disc ratio (CDR). The aware group had a larger CDR (Table 2) which may be a sign of more advanced disease and could be accounted for by the much longer mean duration of disease in this subgroup. There was however, no statistically significant variation in relation to the mode of treatment, the number of topical medications, the level of the intra-ocular pressure (IOP), mean contrast sensitivity score, mean deviation or pattern standard deviation. The significant factors affecting awareness after multiple regression analysis (Table 3) were a positive family history (p = 0.01), duration of disease (p = 0.03) and educational status (p = 0.03).
Some respondents had difficulty getting time off work and spent virtually the whole day in clinic with nearly half of them needing to take the whole day off work to attend follow up visits. Staggered appointment times may help to minimize clinic waiting time. If patients are able to work for half of the day either before or after attending clinics, employers may be more willing to give them time off work to attend clinics. Driving cessation and limitation for visual reasons as experienced by patients in this study has also been reported by Ramulu et al23. This factor impacts the quality of life of patients as it limits the freedom of movement.
The strengths of this study include the fact that it examined crucial aspects of glaucoma patients' knowledge about the disease which could influence early detection of the disease and explored their experience using face to face interviews which allowed for clarification of misunderstood questions and reduced the frequency of missing items in the questionnaire. Being a hospital based study, the demographic characteristics and results are not generalizable to the population. Patients may have exhibited reporter bias by not giving answers that make them appear very ignorant about the disease but this was reduced by the use of trained interviewers who were taught to assure them of the confidentiality of their responses and to avoid facial expressions and utterances which could bias subsequent responses. Even though sampling was consecutive and not randomized, the study population was robust enough to have provided some heterogeneity to the study population. However, the wide confidence intervals of some odd ratios suggest that a larger sample size may have evaluated associations better. The focus on patients' knowledge about glaucoma heritability without evaluating their knowledge about glaucoma as a blinding disease is a limitation to this study.
Assessing the knowledge of glaucoma patients periodically will help identify gaps in their knowledge which should be filled. Patient education should be a continuous process using information, education and communication tools. Family members of glaucoma patients should be encouraged to attend eye health education programs with the patients. Formation of glaucoma patient clubs and organisation of period focus group discussions with knowledgeable glaucoma patients acting as facilitators may help motivate other members to learn more about the disease.
Baker et al.24 reported that while social marketing media strategies raise awareness about glaucoma, they do not influence health seeking behaviour. They advocate the addition of interpersonal interaction and community development to produce a change in behaviour. Glaucoma patients can act as resource persons in their immediate social circle to provide the necessary interpersonal interaction that can make family members undergo screening for glaucoma periodically, if they are equipped with accurate information about the disease. The real tragedy in glaucoma is not that the index irreversibly blind patient presented too late for vision to be preserved but that other family members over time go down the same road of avoidable blindness due to a lack of awareness and poor perception exhibited by most of the respondents in this study.
Methods
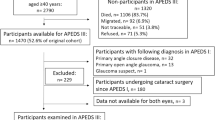
Consecutive patients aged 40 years and above at the time of diagnosis of POAG in either one or both eyes attending the glaucoma clinic of the Lagos University Teaching Hospital in Nigeria were recruited for the study. The study was carried out in accordance with guidelines regulating studies involving human subjects. Written informed consent was obtained from all participants after a detailed explanation of the nature and purpose of the study. Ethical permission was sought and obtained from the ethical committee of Lagos University Teaching Hospital Idi-Araba before the commencement of the study. The study protocol was approved by the Research & Ethical Committee of the Lagos University Teaching Hospital Idi-Araba.
POAG was defined as the presence of features of glaucomatous optic neuropathy: pale and pathologically cupped discs, retinal nerve fibre layer defects, corresponding visual field defects, goniscopically open angles, with or without a raised intra-ocular pressure. Patients with angle closure or secondary glaucoma, optic neuropathies, retinopathies and uncontrolled medical conditions such as hypertension and diabetes were excluded from this study.
Socio-demographic data were obtained from all participants and individual face to face interviews were conducted by trained research assistants using a semi-structured questionnaire and an interview guide to assess the patients' awareness, perceptions and experiences about glaucoma. Only patients who were aware of their diagnosis of glaucoma were questioned further about whether their family was aware of the diagnosis, the heritability of the disease and whether their first degree relatives had undergone screening for glaucoma. All respondents had a comprehensive ocular examination done at the same visit which included optic nerve head assessment, tonometry and gonioscopy. Standard achromatic perimetry (Optifield Sinemed Inc. Benicia, CA. USA) and contrast sensitivity assessment (using the Pelli-Robson chart) were done.
Visual field perimetric indices - mean deviation (MD) were used to stage the disease. Patients with mean deviation less than or equal to −6 dB were defined as having early or mild glaucoma, greater than −6 decibels (dB) but less than −12 dB as moderate glaucoma and greater than −12 dB as severe glaucoma. Cases were classified based on the more severely affected eye.
Participants were asked what eye condition they were being managed for and for how long they had been diagnosed with the disease. Those who knew they were being managed for ‘glaucoma’ were classified as aware of the diagnosis. Those unfamiliar with the term were asked if they knew they were being managed for a pressure related eye disease. Answers in the affirmative were classified as aware even if they could not pronounce the word ‘glaucoma’. Patients, who claimed they did not know why they were being seen periodically in the eye clinic, were classified as unaware. Those that were aware of their diagnosis were then asked if glaucoma could be inherited, if they had informed their relatives that they had glaucoma and if their first degree relatives had been screened for glaucoma. Patients with good depth of perception were expected:
-
to know that glaucoma could be inherited,
-
to have informed their family members that they had been diagnosed to have glaucoma,
-
to have first degree relatives that had undergone screening for glaucoma/or who had been scheduled to be screened for glaucoma.
Perception was defined as fair if two of the three criteria were met. If only one or none of the three criteria was met, perception was defined as poor.
Patients were also asked about the difficulty they experience getting permission from work to attend scheduled clinics, the duration of time spent at each clinic visit and whether they were able to go to their place of work after attending clinics for follow-up. The form of therapy they were on was noted (medical or postsurgical). Those on medical treatment were asked if they experienced side effects from their medications and what the side effects were. Other problems experienced were also noted. They were also asked if glaucoma had forced them to give up an activity they previously indulged in.
Data was initially entered into EXCEL and then exported and analysed using MedCalc Statistical Software Version 12.7.5 (MedCalc Software buba, Ostend, Belgium). Evaluation of group differences was performed using t-tests for continuous variables and Chi-square and Fishers exact tests for categorical variables. Multiple logistic regression analysis was carried out adjusting for confounding variables. A two-tailed p-value < 0.05 was considered statistically significant. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research.
References
Quigley, H. A. & Broman, A. T. The number of people with glaucoma worldwide in 2010 and 2020. Br. J. Ophthal. 90, 262–267 (2006).
Rabiu, M. M. et al. Review of the publications of the Nigeria national blindness survey: Methodology, prevalence, causes of blindness and visual impairment and outcome of cataract surgery. Ann. Afr. Med. 11, 125–130 (2012).
Enock, M. E., Omoti, A. E. & Momoh, R. O. Glaucoma in a suburban tertiary care hospital in Nigeria. J. Ophthal. Vis.Res. 5, 87–91 (2010).
Bodunde, O. T. et al. Knowledge, Attitude and health Believes of Glaucoma patients in a Nigerian Hospital. Niger. Med. Pract. 50, 62–64 (2006).
Nwosu, S. N. Patients' knowledge of glaucoma and treatment options. Niger. J. Clin. Pract. 13, 74–77 (2010).
Onyekwe, L. O., Okosa, M. C. & Apakama, A. I. Knowledge and attitude of eye hospital patients towards Chronic Open Angle Glaucoma in Onitsha. Niger. Med. J. 50, 1–3 (2009).
Adegbehingbe, B. O. & Bisiriyu, L. A. Knowledge, attitudes and self-care practices associated with glaucoma among hospital workers in Ile Ife, Osun State, Nigeria. Tanzan. J. Health Res. 10, 240–245 (2008).
Komolafe, O. O. et al. Awareness and knowledge of glaucoma among workers in a Nigerian tertiary health care institution. Mid. East Afr. J. Ophthalmol. 20, 163–167 (2013).
Gasch, A. T., Wang, P. & Pesquale, L. R. Determinants of glaucoma awareness in a general eye clinic. Ophthal. 107, 303–308 (2000).
Saw, S. M. et al. Awareness of glaucoma and health beliefs of patients suffering primary acute angle closure. Br. J. Ophthal. 87, 446–449 (2003).
Sathyamangalam, R. V. et al. Determinants of glaucoma awareness and knowledge in Urban Chennai. Ind. J. Ophthalmol. 57, 355–360 (2009).
Omoti, A. E., Osahon, A. I. & Waziri-Erameh, M. J. Pattern of presentation of primary open angle glaucoma in Benin City, Nigeria. Trop. Doct. 36, 97–100 (2006).
Odberg, T., Jakobsen, J. E., Haltgren, S. J. & Halseide, R. The impact of glaucoma on the quality of life of patients in Norway. I. Results from a self-administered questionnaire. Acta. Ophthalmol. Scand. 79, 116–120 (2001).
Okeke, C. N. et al. Targeting relatives of patients with primary open angle glaucoma: the help the family glaucoma project. J. Glauc. 16, 549–555 (2007).
Deokule, S., Sadiq, S. & Shah, S. Chronic Open angle Glaucoma: patient awareness of the nature of the disease, topical medication, compliance and the prevalence of systemic symptoms. Ophth. & Phys. Optics. 24, 9–15 (2004).
Adekoya, B. J., Shah, S. P., Onakoya, A. O. & Ayanniyi, A. A. Glaucoma in Southwest Nigeria: clinical presentation, family history and perceptions. Int. Ophthalmol. 34, 1027–1036 10:1007/s10792-014-9903-2 (2014).
Gogate, P., Deshpande, R., Chelerkar, V., Deshpande, S. & Deshpande, M. Is glaucoma blindness a disease of deprivation and ignorance? A case control study for late presentation of glaucoma in India. Ind. J. Ophthalmol. 59, 29–35 (2011).
Hennis, A. et al. Awareness of incident open angle glaucoma in a population study. The Barbados Eye Studies. Ophthal. 114, 1816–1821 (2007).
Tenkir, A., Solomon, B. & Deribew, A. Glaucoma awareness among people attending ophthalmic services in south-western Ethiopia. BMC. Ophthalmol. 10, 17; 10.1186/1471-2415-10-17 (2010).
Prabhu, M., Patil, S. H. & Kangokar, P. C. R. Glaucoma awareness and knowledge in a tertiary care hospital in a tier-2 city in south India. J. of the Sci. Soc. 40, 3–8 (2013).
Lewallen, S. & Courtright, P. Gender differences in cataract: Increasing uptake of eye services by women. J. of Comm. Eye Health. 19, 59–61 (2006).
Kim, S. et al. The effect of a brief education program on glaucoma patients. J. Glauc. 6, 146–151 (1997).
Ramulu, P. Y., West, S. K., Munoz, B., Jampel, H. D. & Friedman, D. S. Driving cessation and driving limitation in glaucoma: the Salisbury Eye Evaluation Project. Ophthal. 116, 1846–1853 (2009).
Baker, H. & Murdoch, I. E. Can a public health package on glaucoma reach its target population? Eye. 18, 478–482 (2008).
Author information
Authors and Affiliations
Contributions
C.A.M. and A.O.O. wrote the manuscript and reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Mbadugha, C., Onakoya, A. The awareness, perceptions and experiences of primary open angle glaucoma patients in Lagos Nigeria. Sci Rep 4, 7585 (2014). https://doi.org/10.1038/srep07585
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep07585
This article is cited by
-
Knowledge of glaucoma and associated factors among primary glaucoma patients in Kunming, China
BMC Ophthalmology (2022)
-
Glaucoma Awareness and Knowledge Among Ethiopians in a Tertiary Eye Care Center
Ophthalmology and Therapy (2021)
-
Awareness and knowledge of glaucoma and associated factors among adults: a cross sectional study in Gondar Town, Northwest Ethiopia
BMC Ophthalmology (2017)
-
Microvascular endothelial function and severity of primary open angle glaucoma
Eye (2016)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.