Abstract
Antiestrogens including tamoxifen and fulvestrant have been evaluated as chemotherapeutics for ovarian cancer, particularly in cases of platinum resistant disease. Human epididymis protein 4 (HE4) is highly overexpressed in women with ovarian cancer and overexpression of HE4 has been found to correlate with platinum resistance. However, the role of HE4 in modulating responses to hormones and hormonal therapy has not been characterized in ovarian cancer. Here we demonstrate that 17β-estradiol, tamoxifen and fulvestrant induce nuclear and nucleolar translocation of HE4 and that HE4 overexpression induces resistance to antiestrogens. HE4 was found to interact with estrogen receptor-α (ER-α) and HE4 overexpression resulted in ER-α downregulation in vitro and in human ovarian cancers. We identified a novel role for importin-4 in governing the nuclear transport of HE4. Treatment with ivermectin, an importin inhibitor, blocked HE4/importin-4 nuclear accumulation and sensitized HE4-overexpressing ovarian cancer cells to fulvestrant and tamoxifen.
Similar content being viewed by others
Introduction
Ovarian cancer is the second most common gynecologic cancer and the fourth leading cause of cancer death in women in the United States resulting in over 15,000 deaths annually. Despite advancements in chemotherapeutics and treatment strategies the overall five year survival rate is only 44% and overall survival has not improved1.
Ovarian cancer initially presents as a chemo-responsive disease with over 80% of women responding to front line platinum based treatment. Despite this, the majority of women will ultimately relapse and develop drug resistant disease that is fundamentally incurable. Therefore the development of new methods of therapy such as biologics and targeted treatments are crucial for the advancement of ovarian cancer treatment and improving survival rates.
Estrogen receptors (ER) are known to be transcriptional regulators which suggest that their effects in neoplastic epithelial ovarian cancer (EOC) are mediated through estrogen regulated target genes. Numerous estrogen induced proteins have been characterized in ovarian cancer cell lines and might have a role in tumor progression2. Estrogen binds to the estrogen receptor (ER) which enters the nucleus to activate expression of genes involved in cell survival and proliferation, thus promoting tumor growth and progression3. Studies of ER mRNA expression in EOC versus normal controls indicate that estrogen signaling via ER may play an indispensable role in regulating ovarian epithelial cell function and loss of expression may be in part responsible for neoplastic transformation4.
Studies of ER-positivity (ER+) in EOC vary but overall approximately 60% of EOC are ER+2. Hormone therapy has been evaluated as a viable treatment approach for EOC5. For example, tamoxifen has been found to stabilize disease and increase progression free survival in 10% of women with advanced stage platinum resistant EOC6,7. Fulvestrant, another antiestrogen, was recently studied in a phase II study for treatment of recurrent EOC and was found to be well tolerated and to stabilize disease in 43% of patients8. Tamoxifen a selective estrogen receptor modulator (SERM) has been widely used as a hormonal therapy for EOC in clinical practice. Approximately 5–18% of women with recurrent EOC will have tumors that respond to tamoxifen treatment and those that respond have shown complete response rates (CRR) ranging from 0–56% in various studies and a mean CRR of 11%. Fulvestrant, which differs from tamoxifen due to its complete antagonist activity at the ER, has also been used in some studies with CRR of 8% and stable disease in 50% of patients2,9,10.
The therapeutic efficacy of tamoxifen in cancer therapy is thought to arise primarily from its antiproliferative action by binding competitively to the ER, thereby blocking the mitogenic effect of estradiol. Tamoxifen is able to induce apoptosis by induction of oxidative stress followed by mitochondrial dysfunction and activation of caspases. Tamoxifen has a direct antiproliferative effect on human ovarian carcinoma specimens and has been shown to delay the development of resistance to cisplatin in vitro in some ovarian carcinoma cell lines7,11.
Human epididymis protein 4 (HE4) is overexpressed in EOC and appears to have a role in ovarian cancer tumorigenesis. Little is known about the biologic function of the WFCD2 gene or its gene product HE4. However, there are hormonal responsive elements present within the WFCD2 promoter and we therefore hypothesized that steroid hormones could influence expression of HE4 in ovarian cancer.
Here we show that treatment of ovarian cancer cells with steroid hormones promote nuclear translocation of HE4. Additionally, we show that overexpression of HE4 decreases responsiveness to hormonal therapy in ovarian cancer cell lines and that this responsiveness can be restored by blocking HE4 from entering the nucleus. We propose that HE4 blocks hormone responsiveness through epigenetic modification. Finally, we report a novel mechanism for HE4 translocation to the nucleus and show that inhibiting HE4 nuclear translocation decreases cancer cell viability after treatment with anti-estrogens.
Results
Stable HE4 overexpression in SKOV3 epithelial ovarian cancer cells confers resistance against fulvestrant and tamoxifen
Using the ovarian cancer cell line SKOV3 we developed HE4 overexpressing clones. We evaluated the therapeutic potential of fulvestrant and tamoxifen in SKOV3 wild type (WT) and SKOV3 HE4-overexpressing clone-1 (C1), as well as in SKOV3 null vector (NV), a non HE4-overexpressing control for SKOV3 C1. An MTS cell viability assay was conducted with each treatment condition in triplicate (Fig. 1A, 1B).
HE4 overexpression confers resistance against antiestrogens in epithelial ovarian cancer cells and estrogen/antiestrogens upregulate HE4 expression.
(a–b) MTS cell viability assays for SKOV3 wild type (WT), null vector (NV) and stably HE4-overexpressing clone-1 (C1). Cells were treated overnight in serum-deprived media with various concentrations of fulvestrant (a) or tamoxifen (b) in triplicate. Fulvestrant and tamoxifen had little to no effect on SKOV3 C1 at concentrations that were cytotoxic to SKOV3 WT and NV. (c–d) Confocal images of fixed SKOV3 WT and OVCAR8 WT cells stained with HE4 primary antibody and corresponding DyLight fluorescent secondary antibody and chromatin staining (DAPI). Cells were stimulated with estradiol, tamoxifen, or fulvestrant overnight in serum-deprived media. Each of these resulted in increased nuclear or nucleolar HE4 expression relative to unstimulated cells.
Low micromolar concentrations of fulvestrant (1, 3.3, 10 μM) were found to be cytotoxic to SKOV3 WT and NV. However, no reduction in cell viability was observed in SKOV3 C1 at these concentrations. There was a significant difference in mean cell viability between SKOV3 C1 and SKOV3 WT or NV at all concentrations of fulvestrant, (p < 0.005). Similarly, 4 μM tamoxifen treatment reduced viability to 86% in SKOV3 WT and 87% SKOV3 NV, but only reduced viability to 98% in SKOV3 C1(p < 0.005).
17β-estradiol tamoxifen and fulvestrant upregulate HE4 nuclear expression in SKOV3 WT and OVCAR8 WT EOC cells
To determine whether 17β-estradiol and the antiestrogens fulvestrant and tamoxifen could modulate HE4 expression in EOC cells we stimulated 2 ovarian cancer cell lines, SKOV3 WT and OVCAR8 WT with estradiol, noncytotoxic concentrations of tamoxifen or fulvestrant,. Fixed cells were stained for HE4 and analyzed via confocal fluorescence microscopy (Fig. 1C, 1D). Stimulation with 1 μM estradiol increased nuclear HE4 expression in both SKOV3 and OVCAR8 WT relative to untreated cells, while 5 μM estradiol resulted in nucleolar accumulation of HE4. 1 μM tamoxifen and 500 nM fulvestrant also induced HE4 nucleolar expression in SKOV3 and OVCAR8 WT.
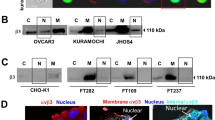
Estrogen receptor-α expression is down regulated in HE4-overexpressing SKOV3 C1
Estrogens and antiestrogens are known to mediate their effector functions primarily through estrogen receptor (ER). To determine basal expression of ER in ovarian cancer cells lines we probed cellular lysates from SKOV3 WT, NV and C1 for ER-α (Fig. 2A). ER-α was almost completely absent in HE4-overexpressing SKOV3 C1, compared to strong basal ER-α expression in SKOV3 WT and NV.
Estrogen receptor-α (ER-α) expression is abrogated in HE4-overexpressing SKOV3 C1 and HE4 interacts with ER-α.
(a) Cellular lysates of SKOV3 WT, NV and C1 grown to 80% confluency in serum-supplemented media were probed for ER-α. SKOV3 C1 demonstrated almost complete absence of ER-α expression, in comparison to SKOV3 WT and NV. (b) Confocal images of fixed SKOV3 NV and C1 cells stained ER-α primary antibody. Cells were either untreated or stimulated with estradiol or fulvestrant overnight in serum-deprived media. In SKOV3 NV, ER-α degraded and internalized to the nucleus upon stimulation with estradiol or fulvestrant, but ER-α signaling was absent in SKOV3 C1. (c) HE4 was immunoprecipitated from lysates of SKOV3 WT, NV and C1 cells with isotype-matched IgG as a control and western blot was performed. ER-α co-immunoprecipitation with HE4 was detected in SKOV3 WT and NV and was not present in SKOV3 C1. (d) Paraffin-embedded ovarian tissue samples from human patients were categorized based on HE4 serum levels and histopathological diagnosis. Tissues were deparaffinized and stained with ER-α primary antibody and examined with confocal microscopy. Serous and endometrioid HE4 low-expressing tumor tissues exhibited strong nuclear ER-α staining in epithelial cells. Meanwhile, serous HE4 high-expressing tissue demonstrated reduced ER-α staining in epithelial cell nuclei.
We also compared ER-α staining in SKOV3 NV vs. C1 using confocal fluorescence microscopy (Fig. 2B). Cells were either untreated or stimulated with estradiol, tamoxifen, or fulvestrant. Untreated SKOV3 NV cells exhibited basal expression of ER-α on their nuclear periphery, but ER-α was largely absent in untreated SKOV3 C1 cells. Upon stimulation with estradiol or antiestrogens, ER-α underwent nuclear internalization and degradation in SKOV3 NV. We also saw through confocal fluorescence microscopy that in SKOV3 WT, ER-α is expressed on the nuclear periphery (Supplementary Fig. 1) and that it exhibits nuclear internalization and degradation upon stimulation with estradiol, fulvestrant, or tamoxifen.
HE4 interacts with estrogen receptor-α
Co-immunoprecipitation was conducted to investigate the interaction between HE4 and ER-α using lysates from SKOV3 WT, NV and C1 cells using HE4 as bait (Fig. 2C). Co-immunoprecipitated lysates were prepared for western blot and probed for ER-α. SKOV3 WT and NV exhibited co-immunoprecipitation of ER-α with HE4, but the HE4-ER-α interaction was absent in HE4-overexpressing SKOV3 C1. We also examined the spatial relationship of HE4 and ER-α in SKOV3 WT cells using immunohistochemistry (Supplementary Fig. 2). Colocalization of ER-α and HE4 was observed in the nuclear periphery of untreated SKOV3 WT cells suggesting an interaction between HE4 and ER-α.
Nuclear ER-α expression is observed in human epithelial ovarian cancer tissue and HE4 overexpression in patient serum corresponds with decreased nuclear ER-α presence
Paraffin-embedded ovarian tissue samples from human patients were categorized based on HE4 serum levels and histopathological diagnosis. Tissue samples were deparaffinized and stained for ER-α (Fig. 2D). Epithelial ovarian cells in normal ovarian tissue (Panel A) exhibited cytoplasmic ER-α staining, while tumor tissue (Panels B–E) exhibited nuclear staining for ER-α. High HE4-expressing epithelial ovarian tissue (Panel C) demonstrated reduced nuclear ER-α staining in comparison to low HE4-expressing tissue. This was similar to our findings in cell culture and suggests that HE4 overexpression may result in decreased ER-α both in vitro and in vivo.
Stable HE4 overexpression in SKOV3 C1 leads to reduced 5-methylcytosine activity and decreased 5-methylcytosine content is observed in HE4-overexpressing human epithelial ovarian cancer tissue
Because the HE4-overexpressing vector used to stably transfect SKOV3 C1 cells may alter transcriptional activity to promote increased HE4 production and secretion, we postulated that epigenetic modifications may be present in SKOV3 C1. 5-methylcytosine (5 MC) antibody was used to distinguish the degree of DNA methylation in SKOV3 WT, NV and C1 cells (Fig. 3A). Nuclear 5 MC expression was consistently observed in SKOV3 WT and NV, but was largely absent with stable HE4 overexpression in SKOV3 C1.
Stable HE4 overexpression in SKOV3 C1 leads to reduced 5-methylcytosine activity.
(a) Confocal images of untreated SKOV3 WT, NV and C1 cells stained for nuclear expression of 5-methylcytosine (5 MC). Nuclear 5 MC expression was observed in SKOV3 WT and NV, but was largely absent in HE4-overexpressing SKOV3 C1. (b) SKOV3 NV and C1 were stimulated with exogenous recombinant HE4 in serum-deprived media overnight and stained for 5 MC. Recombinant HE4 resulted in increased 5 MC activity in SKOV3 NV, but did not impact 5 MC expression in SKOV3 C1 cells with preexisting cellular machinery for HE4 overexpression. (c) Paraffin-embedded ovarian human tissue samples were categorized based on HE4 serum levels and histopathological diagnosis and stained with 5 MC primary antibody. Nuclear 5 MC activity was present in normal ovarian tissue and benign serous tumor tissue, but this nuclear expression was abrogated in HE4 high-expressing serous and endometrioid tumor tissue.
In order to further study whether nuclear 5 MC content would be altered following exposure to exogenous HE4, SKOV3 NV and C1 were incubated with recombinant HE4 and stained with 5 MC antibody (Fig. 3B). Recombinant HE4 resulted in increased 5 MC activity in SKOV3 NV, compared to the cells' basal state. However, there was no effect on nuclear 5 MC expression in SKOV3 C1, suggesting that stable intracellular HE4 overexpression has a direct effect on cytosine methylation.
We also analyzed 5 MC expression in human ovarian tissue samples. Normal ovarian tissue and benign ovarian masses exhibited high levels of 5 MC in epithelial cells (Fig. 3C). However, HE4-overexpressing serous and endometrioid cancer tissue lacked 5 MC nuclear staining; suggesting that the demethylation observed in SKOV3 C1 in cell culture may also be present in human ovarian cancer.
HE4 interacts with importin-4 for nuclear translocation
Macromolecules such as proteins and RNA can only enter the nucleus when assisted by importins. Importins bind these molecules in the cytoplasm and then interact with the nuclear pore complex to gain entry into the nucleus12; importin-assisted transport is therefore crucial for a variety of cellular processes, including viral disease and oncogenesis13,14. We investigated whether importin was involved in mediating HE4 nuclear accumulation following stimulation with estrogens. Untreated SKOV3 WT cells were stained for importin-4 and HE4 and analyzed using confocal fluorescence microscopy (Fig. 4A). Strong colocalization was observed between HE4 and importin-4, both inside the nucleus and on the nuclear periphery. This suggests that importin plays a role in nuclear translocation of HE4.
Importin-4 interacts with HE4 to facilitate nuclear transport.
(a) Confocal microscopy of unstimulated SKOV3 WT cells in serum-supplemented media, stained for HE4 (green fluorescence) and importin-4 (red fluorescence). Strong colocalization (yellow-colored regions) was observed between HE4 and importin-4. (b) Co-immunoprecipitation was conducted using lysates from untreated SKOV3 WT, NV and C1 cells, with HE4 as the primary bait antibody and isotype-matched IgG as a control. In a second set of lysates, importin-4 was used as bait. Western blot was performed and probed for importin-4 primary antibody. An increase in importin-4 co-immunoprecipitation was detected in HE4-overexpressing SKOV3 C1, compared to WT and NV (blot is cropped for image clarity, uncropped image is pictured in supplementary material). (c) Confocal microscopy of unstimulated SKOV3 C1 cells in serum-supplemented media, stained for HE4 (red fluorescence) and importin-4 (green fluorescence). In addition to strong colocalization between HE4 and importin-4, basal levels of nuclear HE4 expression were increased relative to SKOV3 WT.
Co-immunoprecipitation was then performed in SKOV3 WT, NV and C1 cells, with HE4 as the primary bait antibody. Western blot was performed and probed for importin-4 (Fig. 4B). Compared to SKOV3 WT and NV, HE4-overexpressing SKOV3 C1 exhibited increased co-immunoprecipitation of importin-4 with HE4, suggesting that HE4 overproduction in C1 may necessitate a greater degree of importin-4 expression as well as activity. SKOV3 C1 cells were stained for importin-4 and HE4 and analyzed using confocal fluorescence microscopy (Fig. 4C). SKOV3 C1 exhibited higher basal nuclear and nucleolar HE4 expression than SKOV3 WT and this HE4 nuclear accumulation was accompanied by colocalization with importin-4.
Ivermectin, an importin inhibitor, blocks HE4 nuclear translocation
Ivermectin, an FDA-approved anti-parasitic drug used to treat nematode infections in humans, was recently identified as an inhibitor of importin-mediated nuclear transport15. We first studied whether treatment with ivermectin alone would induce cytotoxicity in SKOV3 WT, NV and C1 using an MTS viability assay (Supplementary Fig. 3). Cells were treated with ivermectin concentrations ranging from 0–90 μM. Ivermectin was largely non-cytotoxic up to 10 μM and its IC-50 was found to be approximately 30 μM in SKOV3 WT and NV and between 30–90 μM in SKOV3 C1.
In order to investigate ivermectin's potential to inhibit importin-mediated HE4 nuclear transport, we pretreated SKOV3 WT and OVCAR8 WT cells with a sub-toxic 7.5 μM ivermectin concentration. Cells that received the ivermectin pretreatment were co-administered 7.5 μM ivermectin along with estradiol or fulvestrant, while non-pretreated cells were only stimulated with estradiol or fulvestrant.
Cells were then stained with HE4 antibody and examined by confocal fluorescence microscopy (Fig. 5A, 5B). In both SKOV3 and OVCAR8 WT, ivermectin treatment alone did not affect the health or morphology of cells, compared to untreated control. Stimulation with estradiol or fulvestrant alone resulted in increased HE4 nuclear and nucleolar staining, as previously observed (Fig. 1C, 1D). However, when ivermectin treatment was combined with estradiol or fulvestrant stimulation, nuclear and nucleolar translocation of HE4 was largely inhibited. This represents a clear ability for ivermectin to block HE4 nuclear entry by inhibiting importin. We investigated whether ivermectin could also induce a similar suppression of HE4 nuclear translocation in SKOV3 C1 (Supplementary Fig. 4). As observed previously, HE4 and importin colocalization was seen in nucleoli at low levels and treatment with estradiol or fulvestrant resulted in upregulation of nuclear and nucleolar expression of colocalized HE4 and importin. Ivermectin pre-treatment inhibited importin expression and significantly decreased HE4 transport to the nucleus.
Ivermectin, an importin inhibitor, inhibits HE4 nuclear translocation and sensitizes HE4-overexpressing SKOV3 C1 to fulvestrant and tamoxifen treatment.
(a–b) Confocal microscopy of SKOV3 WT and OVCAR8 WT cells stained with HE4 primary antibody. Cells were pre-treated ivermectin, followed by stimulation with estradiol or fulvestrant and co-administration of ivermectin in serum-free media overnight. Ivermectin treatment inhibited nuclear and nucleolar HE4 translocation typically induced by estradiol and fulvestrant in both SKOV3 and OVCAR8 WT. (c–d) MTS cell viability assay was performed in triplicate in SKOV3 WT, NV and C1. Cells were either untreated or pretreated with ivermectin, followed by overnight treatment in serum-free media with various concentrations of fulvestrant and tamoxifen. Cells that received ivermectin pretreatment were also co-administered ivermectin along with the fulvestrant or tamoxifen. Ivermectin treatment sensitized SKOV3 C1 to concentrations of fulvestrant and tamoxifen that were non-cytotoxic without ivermectin. Furthermore, the viability levels of SKOV3 C1 cells sensitized by ivermectin to fulvestrant and tamoxifen were comparable to those of SKOV3 NV.
Ivermectin treatment sensitizes HE4-overexpressing SKOV3 C1 to the antiestrogen drugs fulvestrant and tamoxifen
Given that treatment with tamoxifen or fulvestrant had significantly decreased cell viability in SKOV3 WT and NV but not SKOV3 C1 and that ivermectin blocks translocation of HE4 to the nucleus we conducted an MTS cell viability assay to study whether ivermectin treatment could help sensitize SKOV3 C1 to fulvestrant and tamoxifen. SKOV3 WT, NV and C1 were either untreated or pretreated with ivermectin followed by treatment with fulvestrant or tamoxifen.
No significant difference was found in cell viability between untreated SKOV3 C1 cells and SKOV3 C1 cells treated only with ivermectin (Fig. 5C, 5D). However, when combined with 10 μM fulvestrant, ivermectin treatment reduced SKOV3 C1 cell viability to 77% relative to the untreated control, while 10 μM fulvestrant alone resulted in 109% viability relative to untreated control. With 20 μM fulvestrant and ivermectin treatment, SKOV3 C1 viability was 60% compared to 91% with 20 μM fulvestrant alone, relative to the untreated control. The mean cell viability with ivermectin co-treatment was significantly reduced compared to with fulvestrant alone at 5, 10 and 20 μM (p < 0.008). Furthermore, SKOV3 C1 viability levels with ivermectin and fulvestrant combined were comparable to those of SKOV3 NV, suggesting that ivermectin may have helped to reduce chemoresistance in SKOV3 C1 by inhibiting importin-mediated HE4 nuclear accumulation.
When ivermectin treatment was combined with 2.5 μM tamoxifen, SKOV3 C1 exhibited 79% viability relative to the untreated control, in comparison to 2.5 μM tamoxifen alone, which resulted in 107% viability relative to untreated control (p = 0.0008). Similarly, 5 μM tamoxifen in combination with ivermectin decreased viability to 17% in comparison to 96% viability with 5 μM tamoxifen alone (p < 0.0001).
Discussion
Fulvestrant and tamoxifen are widely employed as hormonal therapies in breast cancer16,17 and their use has also been proposed in epithelial ovarian cancer, as these tumors have been found to be hormonally responsive5. Up to 63% of EOC have been found to express estrogen receptors18. Platinum-resistant ovarian cancer carries a poor prognosis and response rate to second line chemotherapies is low with significant toxicity. The selective estrogen receptor modulator (SERM) tamoxifen was evaluated as a second-line therapy in cases of advanced platinum-resistant epithelial ovarian cancer and was found to increase progression-free survival (PFS) with minimal attributable toxicity7. Fulvestrant is an estrogen antagonist that competitively binds to the estrogen receptor with a much greater affinity than estrogen or tamoxifen and is FDA-approved for use in breast cancer patients19,20. Fulvestrant was recently investigated in a phase II trial for use in multiply-recurrent epithelial ovarian cancer and was observed to be well-tolerated while inhibiting progression of disease in 43% of patients8.
Although these findings suggest a favorable role for hormonal therapy in some cases of epithelial ovarian cancer (EOC), the effect of HE4 overexpression on hormonal responsiveness has not been characterized. Here we found that SKOV3 WT, an ER-positive cell line, as well as null vector-transfected SKOV3 (NV), expressed basal levels of ER-α but that ER-α was almost completely down regulated in HE4-overexpressing SKOV3 C1, as demonstrated by both western blot and fluorescence staining. Thus, stable overexpression of He4 in SKOV3 Clone-1 promoted resistance to fulvestrant and tamoxifen. We also found that HE4 translocated to the nuclei or nucleoli of SKOV3 and OVCAR8 wild type cells following stimulation with 17β-estradiol or sub-toxic concentrations of fulvestrant or tamoxifen. This suggested that HE4 signaling is responsive to estrogens and antiestrogens; indeed, genomic analysis of the HE4 promoter region identified several hormonal responsive elements including estrogen receptor (ER) and RAR-related orphan receptor A (RORA), which may play a role in HE4 upregulation in ovarian cancer21.
Confocal fluorescence for ER-α also showed that ER-α internalized to the nucleus upon stimulation with estrogens and antiestrogens. We also observed spatial colocalization of HE4 with ER-α in SKOV3 WT, as well as co-immunoprecipitation of ER-α with HE4 in both SKOV3 WT and NV, indicating an interaction between the two proteins. However, co-immunoprecipitation of HE4 and ER-α was absent in SKOV3 C1, again suggesting that downregulation of ER-α occurs following stable HE4 overexpression. This pattern of ER-α downregulation was similarly observed in human EOC tissue, where benign and cancerous tissue from HE4 low-expressing patients exhibited strong nuclear ER-α staining. Meanwhile, serous EOC tissue from a HE4 high-expressing patient showed reduced nuclear ER-α, suggesting that HE4 and ER-α interaction may be present both in vitro and in vivo.
While the exact mechanism of ER-α suppression in SKOV3 C1 is unclear, epigenetic modifications to the ER-α gene have been identified in ER negative breast cancers22,23. In the case of SKOV3 C1, the HE4-overexpressing transfection vector may alter transcriptional activity to promote stable increased HE4 production and secretion. The degree of 5-methylcytosine (5 MC) staining was compared between SKOV3 WT, NV and C1, as DNA cytosine methylation is one of the best-characterized epigenetic modifications and aberrant methylation can result in dysregulation of gene expression and tumorigenesis24,25. 5 MC nuclear expression was frequently observed in SKOV3 WT and NV, but was largely absent in SKOV3 C1 in comparison. In addition, stimulation with exogenous recombinant HE4 increased 5 MC activity in SKOV3 NV, but did not affect 5 MC expression in SKOV3 C1. The known cytotoxic effects of recombinant HE4 may enhance 5 MC staining as a survival response of SKOV-3 cells against this stressor. In human ovarian tissue samples, nuclear 5 MC staining was present throughout normal ovaries and benign ovarian masses, but was almost entirely absent in serous and endometrioid EOC tissue from patients who had high serum levels of HE4.
These findings may indicate that HE4 overexpression can lead to demethylation and reduced 5 MC expression, as a means to promote transcriptional activity conducive to HE4 overproduction. If demethylated regions in the HE4 promoter are upstream of hormonal elements responsive to ER-α, then stable overexpression of these hormone response elements may downregulate ER-α gene expression. Alternatively, other hormonal responsive elements on the HE4 promoter may be more active than ER-α, such as RAR-related orphan receptor A (RORA), which has been shown to assist estradiol-mediated upregulation of gene expression26. Interestingly, tamoxifen and other antiestrogens have been shown to exhibit significant apoptotic effects even in ER-negative ovarian cancer cell lines, suggesting that hormone therapeutics may be able to influence HE4 expression and ovarian cancer cell toxicity independent of ER27.
Because nuclear and nucleolar translocation are likely key to HE4 signaling for oncogenic and chemoresistant functions28, we investigated whether importins might be involved in mediating HE4 nuclear transport. Importin-4 has been implicated in the shuttling of several proteins linked to cancer etiology, including vitamin D receptor (VDR) and hypoxia-inducible factor 1-α (HIF1α)29,30. We discovered a novel interaction between HE4 and importin-4, as evidenced by co-immunoprecipitation and strong spatial colocalization. In HE4 overexpressing SKOV3 C1, increased co-immunoprecipitation of importin with HE4 was observed, as well as increased nuclear and nucleolar colocalization of HE4 with importin. This pointed towards the inhibition of importin as a potential therapeutic means of targeting HE4 mediated signaling.
Ivermectin, a specific importin inhibitor15, was found to effectively inhibit nuclear and nucleolar accumulation of HE4 typically observed following stimulation with estradiol or fulvestrant. Ivermectin treatment also sensitized SKOV3 C1 to both fulvestrant and tamoxifen and cell viability was significantly reduced when ivermectin and antiestrogens were combined compared with antiestrogens alone. These therapeutic effects may have been mediated by inhibition of HE4 importin nuclear transport. Given that we tested a sub toxic concentration of ivermectin, administering ivermectin or other importin inhibitors in conjunction with standard therapeutics may prove beneficial for addressing chemoresistance in EOC particularly when it arises or is potentiated by HE4 overexpression.
Methods
Cell culture and cell viability assays
Human cell lines SKOV3 and OVCAR8 (epithelial ovarian adenocarcinomas) were obtained from the American Type Culture Collection (Manassas, VA, USA). Stably transfected HE4-overexpressing SKOV3 C1 cells, as well as null vector-transfected SKOV3 NV cells, were developed as previously described28. Cells were grown in T-75 culture flasks (Corning, New York, NY, USA) at 37°C/5%CO2 in complete DMEM medium (Gibco, Grand Island, NY, USA), supplemented with 10% fetal bovine serum (Gibco) and 1% penicillin/streptomycin (Gibco) following the supplier's recommendations. Cell viability with or without drug treatment was determined using the 96®Aqueous-One-Solution Assay (Promega, Madison, WI, USA). Briefly, cells (5,000/well) were plated in triplicate into 96-well plates (Corning) and allowed to adhere overnight before treatment with fulvestrant, tamoxifen, or ivermectin (Sigma-Aldrich, St. Louis, MO, USA). After overnight incubation for 18 hours with the appropriate treatment condition, the Promega MTS reagent was added at a 1:10 dilution in serum-supplemented RPMI medium (Gibco) for 1 hour and cell viability was quantified based on absorbance at 490 nm as previously described28 For MTS assays testing fulvestrant, tamoxifen, or ivermectin alone, SKOV3 WT, NV and C1 were allowed to adhere overnight with 5,000 cells per well, incubated with serum-free DMEM for 3 hours and treated overnight in serum-free DMEM with fulvestrant (0–10 μM), tamoxifen (0–4 μM), or ivermectin (0–90 μM). For MTS assays testing combined treatment with ivermectin and antiestrogens, SKOV3 WT, NV and C1 cells were either untreated or pretreated with 7.5 μM ivermectin for 3 hours in serum-free DMEM, followed by overnight incubation with 7.5 μM ivermectin and fulvestrant (0–20 μM), 7.5 μM ivermectin and tamoxifen (0–10 μM), or fulvestrant or tamoxifen without ivermectin. GraphPad Prism (GraphPad Software, La Jolla, CA) was used to conduct student's t-tests and calculate p values based on mean cell viability for each treatment condition.
Immunostaining for fluorescent confocal microscopy
10,000 cells/well were seeded and allowed to adhere overnight in Lab-Tek 8-well chamber slides (Sigma-Aldrich). Following the appropriate treatment condition, cells were fixed with 10% neutral buffered formalin, permeabilized and washed with PBS-Tween 20 0.05% (Sigma-Aldrich) three times. 5% horse serum (Sigma-Aldrich) in PBS-Tween was used to block slides and dilute antibodies. Cells were incubated with primary antibody overnight at 4°C, washed with PBS-Tween (3 × 5 minutes) and incubated with DyLight 488 or 595 secondary antibody (Jackson Laboratories, West Grove, PA, USA) for 1 hour at room temperature in the dark. Slides were washed with PBS-Tween (3 × 5 minutes) and cover-slipped with DAPI-containing mounting medium (Vector Labs, Burlingame, CA, USA). Confocal images were obtained and processed as described previously28.
Cell stimulations for confocal fluorescence
For HE4 staining following estrogen/antiestrogen stimulation, SKOV3 WT and OVCAR8 WT cells were serum-deprived for 3 hours and incubated overnight with 1 or 5 μM 17β-estradiol, 1 μM tamoxifen, or 500 nM fulvestrant. Cells were then stained for HE4 primary antibody (TA307787, Origene, Rockville, MD, USA) at 1:500, followed by Dylight 595 secondary antibody (1:1500). For ER-α staining following estrogen/antiestrogen stimulation, SKOV3 WT, NV and C1 cells were treated with the same conditions mentioned above and stained for ER-α primary antibody (#8644, Cell Signaling, Danvers, MA, USA) at 1:500, followed by Dylight 488 secondary antibody (1:1500). For importin-4 and HE4 staining, untreated SKOV3 WT and C1 cells in complete DMEM were stained for importin-4 (TA302524, Origene) at 1:2000 paired with Dylight 595 and HE4 paired with Dylight 488. For 5-methylcytosine staining, untreated SKOV3 WT, NV and C1 cells in complete DMEM were stained for 5-methylcytosine (sc-56615, Santa Cruz, CA, USA) at 1:500 paired with Dylight 595. SKOV3 NV and C1 cells were also stained for 5-methylcytosine following serum deprivation for 3 hours and overnight incubation with 10 ng of recombinant human HE4, isolated in-house. Finally, for HE4 staining following ivermectin treatment in combination with estradiol or fulvestrant, SKOV3 WT and OVCAR8 WT cells were treated with the same conditions described above for the MTS cell viability assay.
Western immunoblotting
Preparation of cell lysates, PAGE, immunoblotting and chemiluminescent detection were carried out as described previously31. GAPDH (sc47724-Santa Cruz) was probed as an internal loading control. Membranes were probed for HE4 (1:5000) or ER-α (1:1000) following stimulation with 17β-estradiol, fulvestrant, or tamoxifen.
Co-immunoprecipitation
1.5 million SKOV3 WT, NV, or C1 cells were seeded onto 100 mm dishes (Corning) and cultured to 80% confluency in complete DMEM media. Cells were rinsed in DPBS (Gibco), lysed and quantified as published earlier28. Lysates were adjusted to 1 μg/μl total protein concentration, with 500 μl lysate used for each IP reaction. Identical samples were prepared for pull-down antibody (HE4) and isotype-matched IgG control (#3900, Cell Signaling), with antibody concentration identical at 40 ng/μl. Further processing and PAGE analysis of samples was conducted as described earlier28. The resulting membranes were probed for ER-α (1:1000) or importin-4 (1:2000).
References
Surveillance, Epidemiology and End Results (SEER) Program Populations (1969–2009). National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics Branch. http://seer.cancer.gov/statfacts/html/ovary.html Date of access: 06/02/2014.
Cunat, S., Hoffmann, P. & Pujol, P. Estrogens and epithelial ovarian cancer. Gynecol Oncol 94, 25–32, 10.1016/j.ygyno.2004.03.026 (2004).
Sieh, W. et al. Hormone-receptor expression and ovarian cancer survival: an Ovarian Tumor Tissue Analysis consortium study. Lancet Oncol 14, 853–862, 10.1016/S1470-2045(13)70253-5 (2013).
Lau, K. M., Mok, S. C. & Ho, S. M. Expression of human estrogen receptor-alpha and -beta, progesterone receptor and androgen receptor mRNA in normal and malignant ovarian epithelial cells. P Natl Acad Sci USA 96, 5722–5727 (1999).
Makar, A. P. Hormone therapy in epithelial ovarian cancer. Endocrin-Relat cancer 7, 85–93 (2000).
Shirey, D. R. et al. Tamoxifen therapy of epithelial ovarian cancer. Obstet Gynecol 66, 575–578 (1985).
Karagol, H. et al. The efficacy of tamoxifen in patients with advanced epithelial ovarian cancer. Med Oncol 24, 39–43 (2007).
Argenta, P. A. et al. A phase II study of fulvestrant in the treatment of multiply-recurrent epithelial ovarian cancer. Gynecol Oncol 113, 205–209, 10.1016/j.ygyno.2009.01.012 (2009).
Yokoyama, Y. & Mizunuma, H. Recurrent epithelial ovarian cancer and hormone therapy. World J Clin Cases 1, 187–190, 10.12998/wjcc.v1.i6.187 (2013).
Hatch, K. D., Beecham, J. B., Blessing, J. A. & Creasman, W. T. Responsiveness of patients with advanced ovarian carcinoma to tamoxifen. A Gynecologic Oncology Group study of second-line therapy in 105 patients. Cancer 68, 269–271 (1991).
Zhou, R., Treeck, O., Horn, F. & Ortmann, O. Effects of prolonged tamoxifen treatment on receptor expression and apoptosis of ovarian cancer cells. Gynecol Oncol 96, 678–683, 10.1016/j.ygyno.2004.11.023 (2005).
Pryor, M. J. et al. Nuclear localization of dengue virus nonstructural protein 5 through its importin alpha/beta-recognized nuclear localization sequences is integral to viral infection. Traffic 8, 795–807, 10.1111/j.1600-0854.2007.00579.x (2007).
Moseley, G. W., Filmer, R. P., DeJesus, M. A. & Jans, D. A. Nucleocytoplasmic distribution of rabies virus P-protein is regulated by phosphorylation adjacent to C-terminal nuclear import and export signals. Biochemistry-US 46, 12053–12061, 10.1021/bi700521m (2007).
Hogarth, C. A., Calanni, S., Jans, D. A. & Loveland, K. L. Importin alpha mRNAs have distinct expression profiles during spermatogenesis. Dev Dynam 235, 253–262, 10.1002/dvdy.20569 (2006).
Wagstaff, K. M., Sivakumaran, H., Heaton, S. M., Harrich, D. & Jans, D. A. Ivermectin is a specific inhibitor of importin alpha/beta-mediated nuclear import able to inhibit replication of HIV-1 and dengue virus. Biochem J 443, 851–856, 10.1042/BJ20120150 (2012).
Vergote, I. & Abram, P. Fulvestrant, a new treatment option for advanced breast cancer: tolerability versus existing agents. Ann Oncol 17, 200–204, 10.1093/annonc/mdj047 (2006).
Howell, A. et al. Comparison of fulvestrant versus tamoxifen for the treatment of advanced breast cancer in postmenopausal women previously untreated with endocrine therapy: a multinational, double-blind, randomized trial. J Clin Oncol 22, 1605–1613, 10.1200/JCO.2004.02.112 (2004).
Slotman, B. J. & Rao, B. R. Ovarian cancer (review). Etiology, diagnosis, prognosis, surgery, radiotherapy, chemotherapy and endocrine therapy. Anticancer Res 8, 417–434 (1988).
Wakeling, A. E., Dukes, M. & Bowler, J. A potent specific pure antiestrogen with clinical potential. Cancer Res 51, 3867–3873 (1991).
Morris, C. & Wakeling, A. Fulvestrant (‘Faslodex’)--a new treatment option for patients progressing on prior endocrine therapy. Endocrin-Relat Cancer 9, 267–276 (2002).
Berry, N. B. et al. Transcriptional targeting in ovarian cancer cells using the human epididymis protein 4 promoter. Gynecol Oncol 92, 896–904, 10.1016/j.ygyno.2003.12.024 (2004).
Yoshida, T. et al. Distinct mechanisms of loss of estrogen receptor alpha gene expression in human breast cancer: methylation of the gene and alteration of trans-acting factors. Carcinogenesis 21, 2193–2201 (2000).
Counts, J. L. & Goodman, J. I. Alterations in DNA methylation may play a variety of roles in carcinogenesis. Cell 83, 13–15 (1995).
Robertson, K. D. DNA methylation and human disease. Nat Rev Genet 6, 597–610, 10.1038/nrg1655 (2005).
Bird, A. DNA methylation patterns and epigenetic memory. Gene Dev 16, 6–21, 10.1101/gad.947102 (2002).
Gu, F. et al. Inference of hierarchical regulatory network of estrogen-dependent breast cancer through ChIP-based data. BMC Syst Biol 4, 170, 10.1186/1752-0509-4-170 (2010).
Ercoli, A. et al. Comparative study on the induction of cytostasis and apoptosis by ICI 182,780 and tamoxifen in an estrogen receptor-negative ovarian cancer cell line. Int J Cancer 76, 47–54 (1998).
Moore, R. G. et al. HE4 (WFDC2) gene overexpression promotes ovarian tumor growth. Sci Rep 4, 3574, 10.1038/srep03574 (2014).
Miyauchi, Y. et al. Importin 4 is responsible for ligand-independent nuclear translocation of vitamin D receptor. J Biol Chem 280, 40901–40908, 10.1074/jbc.M509347200 (2005).
Chachami, G. et al. Transport of hypoxia-inducible factor HIF-1alpha into the nucleus involves importins 4 and 7. Biochem Bioph Res Co 390, 235–240, 10.1016/j.bbrc.2009.09.093 (2009).
Lange, T. S. et al. Apoptotic and chemotherapeutic properties of iron (III)-salophene in an ovarian cancer animal model. Drug Des Devel Ther 3, 17–26 (2009).
Acknowledgements
This study was supported by a ‘Swim Across America’ grant to R.G.M. and R.K.S. R.G.M. is also supported by NCI grant RO1 CA136491-01.
Author information
Authors and Affiliations
Contributions
E.L., A.H. and R.K.S. conceived and designed the experiments. Cell culture, western blots, confocal microscopy and MTS assays were conducted by E.L., A.H. and N.R. Co-immunoprecipitations were performed by N.Y. and K.K. Manuscript was written by A.H., E.L. and R.K.S. and was edited by R.G.M. All authors read and approved the manuscript.
Ethics declarations
Competing interests
R.G.M. and R.K.S. are listed as co-inventors on a patent (US61/493881). Patent was assigned to Women and Infants Hospital of Rhode Island. Other authors declare that no competing interest exists.
Electronic supplementary material
Supplementary Information
Supplementary Data Set
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Lokich, E., Singh, R., Han, A. et al. HE4 expression is associated with hormonal elements and mediated by importin-dependent nuclear translocation. Sci Rep 4, 5500 (2014). https://doi.org/10.1038/srep05500
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep05500
This article is cited by
-
ZNF703 promotes tumor progression in ovarian cancer by interacting with HE4 and epigenetically regulating PEA15
Journal of Experimental & Clinical Cancer Research (2020)
-
Quantitative proteomics revealed energy metabolism pathway alterations in human epithelial ovarian carcinoma and their regulation by the antiparasite drug ivermectin: data interpretation in the context of 3P medicine
EPMA Journal (2020)
-
Anti-parasite drug ivermectin can suppress ovarian cancer by regulating lncRNA-EIF4A3-mRNA axes
EPMA Journal (2020)
-
Tissue HE4 Expression Discriminates the Ovarian Serous Carcinoma but Not the Uterine Serous Carcinoma Patients. A New Adjunct to the Origin of the Tumor Site
Pathology & Oncology Research (2020)
-
WAP four-disulfide core domain protein 2 gene(WFDC2) is a target of estrogen in ovarian cancer cells
Journal of Ovarian Research (2016)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.