Abstract
Study design: Investigation of bladder-filling sensation in 73 consecutive traumatic spinal cord injury (SCI) patients during laboratory cystometry.
Objectives: To determine the frequencies of bladder-filling sensation in SCI patients with complete lesions above T11 and below T10 and with incomplete lesions, to examine the quality of the preserved sensation, as well as to determine the potential for sensation-dependent bladder emptying in this patient group.
Setting: Physical Medicine and Rehabilitation Education and Research Hospital of Ministry of Health, Ankara, Turkey.
Methods: Bladder-filling sensation was investigated in 73 consecutive patients with traumatic SCI using continuous medium fill cystometry. Bladder-filling sensation was categorised as absent, partially preserved or preserved. Presence of bladder-filling sensation before intravesical pressure (Pves) reached 25 and 40 cmH2O, and simultaneous presence of bladder capacity of more than 150 ml were investigated as the measures of the quality of the sensation.
Results: Bladder-filling sensation was present to some degree in all incomplete SCI patients, in 82.4% of the patients with complete lesions below T10, and 38.9% of the patients with complete lesions above T11. There were statistically significant differences between three groups with respect to bladder sensation category (P<0.001). About 86% of the patients with incomplete lesions, 53% of the patients with complete lesions below T10 and 22% of those with lesions above T11 had bladder-filling sensation before Pves reached 25 cmH2O and simultaneous bladder capacity of more than 150 ml was present in 61.2, 41.2 and 22.2% of the patients in the groups, respectively. Bladder-filling sensation investigations were reliable in terms of bladder filling sensation category in 36 SCI patients who had second cystometric examination.
Conclusion: Presence of bladder-filling sensation in many of the SCI patients observed in this study revealed the potential for sensation-dependent bladder emptying in SCI patients, especially in the ones with complete lesions below T10 and the ones with incomplete lesions. This method may prevent early emptying attempts, unnecessary catheterisations and overdistension episodes and may improve the patient's self-esteem and quality of life. However, further studies on clinical experience and patient compliance for this method are needed.
Similar content being viewed by others
Introduction
Neurogenic voiding dysfunction is a common consequence of spinal cord injury (SCI) that can cause significant morbidity and reduce quality of life.1 Investigation and management of neurogenic voiding dysfunction are imperative because of the urological manifestations of SCI. The optimal method of bladder management should preserve renal function, minimise the risk of urothelial neoplasm and minimise urinary tract complications. In addition, patient comfort, convenience and quality of life are important factors in bladder management decisions.2 Clean intermittent catheterisation, spontaneous voiding with and without triggered voiding and/or bladder expression (in well-defined patients with regular urological follow-up), chronic urethral catheterisation and suprapubic catheterisation are bladder management alternatives.2,3,4,5 In SCI patients, intermittent catheterisation, spontaneous voiding and passive voiding by straining are performed in a time-dependent manner and generally on a regimen every 4–6 h.6,7 In such a time-dependent regimen, physiological changes in urinary excretion related to fluid intake or environmental changes (such as temperature alterations) may lead to unnecessary catheterisations and early emptying attempts or to bladder overdistension.6,7,8
The importance of perianal pinprick sensation and toe position sense in predicting the recovery of bladder function in SCI patients has been reported.9 Adequate sensory input is required for conscious bladder control and to store and expel urine at a convenient time and place.10,11 Therefore, evaluation of bladder-filling sensation, which guides daily urinary behaviour can provide additional relevant information during urodynamic studies.12,13 Bladder-filling sensation in SCI patients has been investigated in a few studies, which reported preservation of bladder-filling sensation in incomplete lesions and even in some of the complete lesions.14,15,16 Afferent activity arising in the bladder is conveyed to the central nervous system over both pelvic, pudental and hypogastric nerves.10,11,17 Hypogastric nerve (T11–L2)11,12 carries the bladder sensation by the most proximal spinal level among these three nerves.
The aim of our study was to evaluate the presence of bladder-filling sensation in SCI patients and to determine and compare the frequencies of preserved sensation in patients with complete lesions above and below the sensory innervation of bladder and in patients with incomplete lesions. We examined the reliability of the cystometric subjective bladder-filling sensation investigations in SCI patients. We also investigated the quality of the sensations preserved which may provide feedback from the bladder to the cerebral cortex. The main goal was to investigate the potential for sensation-dependent bladder emptying in SCI patients which may prevent both early emptying attempts and overdistension episodes, and may provide more physiological bladder emptying and improve quality of life.
Methods
Patients
A total of 73 consecutive patients with traumatic SCI who had been referred to the urodynamics laboratory because of voiding dysfunction and who had indication for urodynamic investigation were included in the study. They were 55 male and 18 female patients. The mean age was 33.8±11.2 years (range: 17–70, median: 32). The mean interval between the trauma and the examination was 13.7±24.3 months (range: 1–168, median: 6). In all, 52 patients (34 below T10 and 18 above T11) had a neurologic lesion corresponding with score A on the ASIA/IMSOP classification18 (complete lesion) and 21 had non-A (incomplete lesion). The level and type of the spinal cord lesion are given in Table 1. All of the patients were out of spinal shock and none had lower urinary tract symptoms prior to their SCI. None of the patients included had previous surgery of the urinary tract and at the moment of the test, none of the patients was on urodynamic drugs.
Urodynamic investigation
Urodynamic investigations were performed by the same investigator (first author) using a Libra+ (MMS, Enschede, The Netherlands) urodynamic measurement system. Each patient was positioned supine on a urological table. An 8Fr 2-lumen catheter was introduced transurethrally for bladder filling and was fixed on the body surface with tape. The bladder was emptied. Continuous medium fill cystometry was performed at 50 ml/min with room temperature sterile saline. Blood pressure monitoring was not carried out during the cystometric examinations, but signs or symptoms of autonomic dysreflexia were strictly monitored, especially in the patients who had cervical and higher thoracic lesions.
The patients were informed about the bladder-filling sensations (first sensation of bladder filling, first desire to void and strong desire to void)12,13 before the investigation and were asked to report all sensations related to bladder filling, but not to report if they do not feel anything. Explanations for the sensations were as follows: (1) ‘first sensation of bladder filling’ was described as initial sensation of bladder filling (a vague sensation felt in the lower pelvis and could easily be ignored). (2) ‘First desire to void’ was explained as a familiar constant sensation that normally lead a person to pass urine at the next convenient moment, but voiding could be delayed. It is felt in the lower abdomen and did not disappear during further filling but became gradually stronger. (3) ‘Strong desire to void’ was described as a constant almost uncomfortable sensation in the perineal region or urethra and was felt as a strong urge or great tension. The bladder was considered to be full, voiding as no longer to be postponed.
The patients were not allowed to watch the screen or pump of the urodynamic measurement system during the test. Each sensation was marked on the cystometric curve. Intravesical pressures (Pves) were measured. Although subtracted detrusor pressure was not derived, the characters of the cystometric tracings were consistent with detrusor activity. We believe that the reported disadvantages of rectal pressure monitoring, that is, poor pressure recording because of low or inappropriate insertion of rectal catheter, contact of the rectal transducer to rectal walls or faeces, rectal motility and contractions, detrusor activity influenced with rectal stimulation19,20,21,22,23,24 are more prominent in SCI patients because of the increased reflex activity and the possibility of inconsistent results is higher in this patient group due to higher and instable rectal pressure measurements. Filling ended when the patient had a strong desire to void or a significant void or leak occurred or when Pves reached 50 cmH2O or infused volume reached 500 ml without any sensation. Filling was also stopped if the patient reported any type of discomfort or asked for not to continue. At the end of the examination, the patients who had any sensation during the bladder filling were asked whether the sensation they had perceived was the same as the sensation before the trauma or different in quality or magnitude. Then bladder-filling sensation was categorised as 1=absent, 2=partially preserved (different in quality or magnitude), 3=preserved (same as it was before the trauma). Presence of bladder-filling sensation before specific Pves and simultaneous presence of a defined bladder capacity was also investigated. Presence of bladder sensation before dangerous Pves is important in the prevention of upper urinary tract damage. The resting Pves range between 12 and 32 cmH2O in normal subjects22 and pressures greater than 40 cmH2O has resulted in upper urinary tract deterioration in the long term.25 Bladder capacity of more than 150 ml has been reported as the criterion for balanced bladder.26 In this study, presence of bladder-filling sensation in Pves lower than 25 and 40 cmH2O, and presence of bladder capacity of more than 150 ml at the same time were investigated as the measures of the quality of the sensation. Reliability of bladder-filling sensation investigations in terms of bladder sensation category was tested in 36 patients who had second cystometric investigation for periodic follow-up or for evaluation of the improvement by medical treatment. The mean interval between the two investigations was 50.8±45.8 days (range: 18–191, median: 28). The relationship between bladder filling sensation category and the interval between trauma and the urodynamic examination was also investigated in patients with incomplete lesions and in patients with complete lesions above T11 and below T10 separately.
Statistical analysis
The SPSS software Version 8.0 was used for data analysis. The data were expressed as the mean and standard deviation or as frequencies when appropriate. The groups (incomplete, complete above T11 and complete below T10) were compared by χ2 test for bladder-filling sensation category. The frequencies of the patients in each of the groups who had bladder-filling sensation before specific Pves and the patients who had bladder capacity of more than 150 ml at the same time were also determined. The Spearman's nonparametric correlation test was performed for testing the reliability of cystometric investigations in terms of bladder-filling sensation category and for investigating the relationship between bladder-filling sensation category and the interval between trauma and the urodynamic examination. The level P<0.05 was used as a cutoff level for statistical significance.
Results
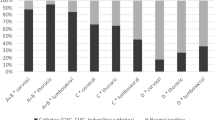
The frequencies of the patients with incomplete and complete lesions in bladder-filling sensation categories were significantly different according to the χ2 test results (P<0.001) (Table 2).
The frequencies of the patients with complete lesions above T11 and below T10 and with incomplete lesions for bladder-filling sensation categories were also significantly different (P<0.001) (Table 3). There were statistically significant differences between complete lesion above T11 and incomplete lesion groups (P<0.001), between complete lesion below T10 and incomplete lesion groups (P<0.001) and between complete lesion above T11 and below T10 groups (P=0.001).
The frequencies of the presence of any bladder-filling sensation (preserved+partially preserved) were 21/21 (100%) for patients with incomplete lesions, 7/18 (38.9%) for patients with complete lesions above T11, and 28/34 (82.4%) for patients with complete lesions below T10. The number of patients who have any bladder sensation preserved were 14/17 (82.4%) for complete lumbosacral lesions, 9/11 (81.8%) for T12 complete lesions, 5/6 (83.3%) for T11 complete lesions, 1/2 (50%) for T10 complete lesions, 1/1 (100%) for T9 complete lesions and 1/5 (20%) for T8 complete lesions. The frequencies of the presence of first sensation of bladder filling and first and strong desire to void sensations in patients with complete lesions above T11 and below T10 and with incomplete lesions are presented in Table 4.
The frequencies of any sensation before Pves of 25 and 40 cmH2O and presence of bladder capacity of more than 150 ml at the same time in the three groups are shown in Table 5.
The reliability of bladder-filling sensation investigations was tested in 36 patients who had second cystometric investigation, 11 with incomplete lesions, eight with complete lesions above T11 and 17 with complete lesions below T10. Spearman's nonparametric correlation test was performed for testing the reliability of cystometric examinations in terms of bladder-filling sensation category and the correlation coefficient was 1.0 (P<0.01) for all groups. Although discordance was observed in first sensation of bladder filling and first and strong desire to void sensations in some of the patients, bladder-filling sensation category did not change in any patient. There was discordance in first sensation of bladder filling and first and strong desire to void sensations in six patients. Three patients (T5 ASIA A, T6 ASIA A, T12 ASIA A) reported strong desire to void in the first examination, but not in the second, which was performed after oxybutinin administration. The remaining three patients had complete lumbosacral lesions. One patient did not report first desire to void but reported first sensation of bladder filling and strong desire to void in the first examination. He reported all the three sensations separately in the second examination, which was carried out after oxybutinin therapy. The other two patients who had complete lumbosacral lesions reported first sensation of bladder filling and strong desire to void but did not report first desire to void in one of the examinations.
There were no significant correlations between bladder-filling sensation category and the interval between trauma and the urodynamic examination in 21 patients with incomplete lesions (r=0.016, P=0.944), in 18 patients with complete lesions above T11 (r=−0.121, P=0.631), and in 34 patients with complete lesions below T10 (r=−0.058, P=0.748).
In the study, only one autonomic dysreflexia episode was observed, which was in a man with C6 ASIA B lesion. During the cystometric examination, he reported the three sensations separately and sequentially, but complained of blurred vision and piloerection just after he reported strong desire to void at 313 ml and 24 cmH2O. A detrusor contraction occurred and Pves reached 41 cmH2O. The bladder emptied immediately and the symptoms disappeared. The patient was told not to postpone emptying the bladder after he felt strong desire to void in order to avoid any autonomic dysreflexia episodes and was given oxybutinin. In the second examination, which was performed 1 month later, strong desire to void was reported at 478 ml and 21 cmH2O and no signs or symptoms of autonomic dysreflexia were observed.
Discussion
Investigation and management of neurogenic voiding dysfunction are mandatory in SCI patients. Bladder-filling sensation examination is an important part of the investigation. In our study, all patients with incomplete spinal cord lesions had bladder-filling sensation, which is in parallel with the results of a previous report.15 Interestingly, 67.3% of the patients with complete lesions had bladder-filling sensation to some degree. Preservation of bladder sensation in complete spinal cord lesions has also been reported previously.15,16 According to these reports, 15/42 (35.7%)15 and 11/48 (22.9%)16 SCI patients with complete lesions have bladder sensation independent of the level of injury. In another study, in which 57 patients with conus medullaris and cauda equina injury with preserved perianal sensation in 13 (23%) and absent or diminished in 44 (77%) were evaluated, bladder sensation was reported as present in 29 patients (51%) and diminished or absent in 28 (49%).14 In our study, investigation of the patients with complete lesions revealed preservation of bladder sensation in 38.9% of the patients with lesions above the spinal level of sensory innervation of bladder (above T11) and in 82.4% of the patients with lesions below the spinal level of sensory innervation of the bladder (below T10). Patients with complete lesions above T11 and below T10 and with incomplete lesions were significantly different in terms of filling sensation category, which raised the need of different clinical approaches for each group. In our study, we accepted hypogastric nerve (T11–L2)11,12 as the most proximal sensory innervation of bladder with respect to spinal level. Preservation of bladder sensation in nine of 11 patients with T12 complete lesions (81.8%), and five of six patients with T11 complete lesions (83.3%) further supported that bladder-filling sensation is carried by these segments. We have few patients with T10 and T9 complete lesions, which would provide any information about the sensory innervation of the bladder by these segments, but only one of the five patients with T8 complete lesions (20%) have preserved bladder-filling sensation. The high percentage of preserved sensation in patients with complete lesions observed in our study may be a reflection of the higher number of patients with lesions below T10.
The completeness of spinal cord lesions is determined by the examinations of pinprick and light touch sensations of the perianal area and the voluntary contraction of the external anal sphincter.18 In patients with complete lesions below T10, the bladder still has some innervation for filling sensation and at least one segment still carries the bladder sensation. The preserved bladder-filling sensation in patients with complete lesions above T11 can be explained by the assumption that some neurological tracts in the spinal cord that carry bladder-filling sensation and are different from the ones that carry pinprick and light touch sensations may be spared in SCI patients. Moreover, Wyndaele16 proposed that it would seem advisable that completeness of spinal cord lesion should only be accepted after evaluation of lower urinary tract sensation.
The frequencies of presence of first sensation of bladder filling and first and strong desire to void sensations in patients with incomplete lesions and with complete lesions above T11 and below T10 were similar to the frequencies observed when the patients were classified as ‘sensation absent’ or ‘any bladder sensation present’. Only in the complete lesion below T10 group was there a discrepancy among these sensations. First sensation of bladder filling was present in 79.4%, but first and strong desire to void sensations were present in 67.6% of these patients. This may be due to hypercompliance of the bladder in some patients in this group. First sensation of bladder filling was felt, but first and strong desire to void sensations were not felt because of low Pves, although high intravesical volumes are reached. Another explanation may be the preservation of the segments that carry the sensation from the first sensor located at the trigone and the damage of the pathways that carry the desire to void from second sensors within the bladder body.27 An important finding to be mentioned here is that bladder sensation was described as pain, tension or burning sensation by some of the patients rather than a desire to void in our study.
Short-term and long-term reproducibilities of bladder-filling sensation have been reported previously.28 In our study, bladder-filling sensation investigations were reliable with respect to bladder-filling sensation category in 36 patients who had second cystometric investigation, 11 with incomplete lesions, eight with complete lesions above T11 and 17 with complete lesions below T10. Correlation coefficient was 1.0. Although discordance was observed in first sensation of bladder filling and first and strong desire to void sensations in some of the patients, bladder-filling sensation category did not change in any patient. In six patients, discordance in first sensation of bladder filling and first and strong desire to void sensations was observed. All the six patients had complete lesions. Three patients with thoracic lesions had hyper-reflexic detrusor and were given oxybutinin. These patients reported strong desire to void in the first examination but not in the second, which was performed after oxybutinin administration. Hypercompliance due to oxybutinin treatment and low Pves, although high intravesical volumes are reached, may be the possible explanation. The remainder were patients with complete lumbosacral lesions. One patient did not report first desire to void but reported first sensation of bladder filling and strong desire to void in the first examination in which a rapid and a strong detrusor contraction occurred 2 min after first sensation of bladder filling and led to a rapid increase in Pves. This rapid change possibly resulted in difficulty in reporting and determining the first and strong desire to void sensations separately and sequentially. In the second examination, which was carried out after oxybutinin therapy, the patient reported all the three sensations separately. The other two patients who had complete lumbosacral lesions reported first sensation of bladder filling and strong desire to void, but did not report first desire to void in one of the examinations which may be due to poor cooperation.
There were no significant correlations between bladder-filling sensation category and the interval between trauma and the urodynamic examination in the patients with incomplete lesions, in the patients with complete lesions above T11 and in the ones with complete lesions below T10. Although discordance was observed in first sensation of bladder filling and first and strong desire to void sensations in some of the patients, according to our results, there is no change in the bladder-filling sensation in terms of bladder-filling sensation category at different times from injury.
About 86% of the patients with incomplete lesions, 53% of the patients with complete lesions below T10 and 22% of the ones with lesions above T11 had some type of bladder-filling sensation before Pves reached 25 cmH2O, which is a relatively safe Pves. Although there was no major change in complete lesion above T11 and incomplete lesion groups, the percentage of the patients with preserved bladder sensation rose from 53 to 73.5% in complete lesion below T10 group when 40 cm H2O was used as the upper limit. About 61% of the patients with incomplete lesions, 41% of the patients with complete lesions below T10 and 22% of the ones with lesions above T11 had bladder-filling sensation before Pves reached 25 cmH2O and had bladder capacity of more than 150 ml at the same time. Only in the complete lesion below T10 group, the percentage rose (from 41 to 61.8%) when the pressure limit was 40 cmH2O. Although 40 cmH2O is a high Pves, because of the hyper-reflexic nature of the bladder, rapid changes in Pves from the ones that do not evoke sensation, to significantly high pressures may occur and the first sensation sometimes appears at higher Pves in some of the SCI patients. These rapid changes may also lead to difficulty in reporting and determining the different sensations separately and sequentially. For example, when a strong detrusor contraction occurs, the patient may report only strong desire to void, or first sensation of bladder filling and first and strong desire to void sensations may be felt in a very short time.
As mentioned before, the patients in the study were not taking any medication with known action on bladder function at the time of examination. Marked changes were reported in intravesical pressure and volume at which various filling sensations occurred after bethanechol administration, which is a cholinergic agent.29,30 Knowing that improvements can be achieved in bladder capacity and Pves by some urodynamic drugs such as oxybutinin, which has anticholinergic activity, we can speculate that restoring a conscious bladder with safe Pves and a sufficient capacity seems possible in many of the SCI patients, especially in those with complete lesions below T10 and with incomplete lesions. This can be achieved by the communication of the physician with the patient during cystometric studies. The patients should learn the sensations at safe Pves and appropriate bladder volumes with the help of the physician. Regular urodynamic follow-up will maintain reliable bladder sensation. We believe that re-education of bladder-filling sensation in SCI patients not only acts as a guide for bladder emptying but also may protect some of the patients from autonomic dysreflexia episodes due to bladder overdistension. The patient who experienced an autonomic dysreflexia episode in our study is a good example. He learned the bladder sensation prior to autonomic dysreflexia and never postponed bladder emptying when he felt this type of sensation for avoiding any autonomic dysreflexia episodes. Although we did not have any other autonomic dysreflexia episodes, the contribution of autonomic dysreflexia symptoms to the perceived sensation of bladder filling in higher level injury patients may be possible and should be kept in mind.
According to our data, sensation-dependent bladder emptying seems possible in many SCI patients. Prevention of inappropriate emptying attempts, and more physiological urinary behaviour can be achieved by this method. However, the persistence and magnitude of bladder sensation in different conditions during daily life and the compliance of the patients to sensation-dependent bladder-emptying regimen should be investigated by further studies. This is an initial study. Patients with higher lesions require routine life-long urologic follow-up and periodic bladder-filling sensation examinations as upper tract deterioration can potentially occur.
Conclusion
To summarise, bladder-filling sensation is present to some degree in all incomplete SCI patients, in more than 80% of the patients with complete lesions below T10, and about 39% of the patients with complete lesions above T11. Bladder-filling sensation investigations are reliable in SCI patients when bladder-filling sensation is categorised as absent, preserved and partially preserved
The results of this study also revealed the potential for sensation-dependent bladder emptying in SCI patients especially in those with complete lesions below T10 and with incomplete lesions. This method may prevent early emptying attempts, unnecessary catheterisations and overdistension episodes. It may provide more physiological urinary behaviour and will improve the patient's self-esteem and quality of life. However, further studies on clinical experience and patient compliance for this method are needed.
References
Whiteneck GG et al. Mortality, morbidity, and psychosocial outcomes of persons spinal cord injured more than 20 years ago. Paraplegia 1992; 30: 617–630.
Weld KJ, Dmochowski RR . Effect of bladder management on urological complications in spinal cord injured patients. J Urol 2000; 163: 768–772.
Madersbacher H . The various types of neurogenic bladder dysfunction: an update of current therapeutic concepts. Paraplegia 1990; 28: 217–229.
Wyndaele JJ, Maes D . Clean intermittent self-catheterization: a 12-year followup. J Urol 1990; 143: 906–908.
Wyndaele JJ, Madersbacher H, Kovindha A . Conservative treatment of the neuropathic bladder in spinal cord injured patients. Spinal Cord 2001; 39: 294–300.
Anton HA, Chambers K, Clifton J, Tasaka J . Clinical utility of a portable ultrasound device in intermittent catheterization. Arch Phys Med Rehabil 1998; 79: 172–175.
De Ridder D, Van Poppel H, Baert L, Binard J . From time dependent intermittent self-catheterisation to volume dependent self-catheterisation in multiple sclerosis using the PCI 5000 Bladdermanager. Spinal Cord 1997; 35: 613–616.
Klevmark B . Natural pressure–volume curves and conventional cystometry. Scand J Urol Nephrol Suppl 1999; 201: 1–4.
Weiss DJ et al. Spinal cord injury and bladder recovery. Arch Phys Med Rehabil 1996; 77: 1133–1135.
de Groat WC . Anatomy and physiology of the lower urinary tract. Urol Clin North Am 1993; 20: 383–401.
de Groat WC . Mechanisms underlying the recovery of lower urinary tract function following spinal cord injury. Paraplegia 1995; 33: 493–505.
Wyndaele JJ . The normal pattern of perception of bladder filling during cystometry studied in 38 young healthy volunteers. J Urol 1998; 160: 479–481.
Wyndaele JJ, Wachter SD . Cystometrical sensory data from a normal population: comparison of two groups of young healthy volunteers examined with 5 years interval. Eur Urol 2002; 42: 34–38.
Pavlakis AJ, Siroky MB, Goldstein I, Krane RJ . Neurourologic findings in conus medullaris and cauda equina injury. Arch Neurol 1983; 40: 570–573.
Wyndaele JJ . Investigation of the afferent nerves of the lower urinary tract in patients with ‘complete’ and ‘incomplete’ spinal cord injury. Paraplegia 1991; 29: 490–494.
Wyndaele JJ . Correlation between clinical neurological data and urodynamic function in spinal cord injured patients. Spinal Cord 1997; 35: 213–216.
Comarr AE . Neurourology of spinal cord-injured patients. Semin Urol 1992; 10: 74–82.
Maynard Jr FM et al. International Standards for Neurological and Functional Classification of Spinal Cord Injury. American Spinal Injury Association. Spinal Cord 1997; 35: 266–274.
Abdel-Rahman M et al. Urorectodynamic evaluation of healthy volunteers. Urology 1982; 19: 559–564.
McCarthy TA . Validity of rectal pressure measurements as indication of intra-abdominal pressure changes during urodynamic evaluation. Urology 1982; 20: 657–660.
Bhatia NN, Bergman A . Urodynamic appraisal of vaginal versus rectal pressure recordings as indication of intra-abdominal pressure changes. Urology 1986; 27: 482–485.
James ED, Niblett PG, MacNaughton JA, Shaldon C . The vagina as an alternative to the rectum in measuring abdominal pressure during urodynamic investigations. Br J Urol 1987; 60: 212–216.
Al-Taher H, Sutherst JR, Richmond DH, Brown MC . Vaginal pressure as an index of intra-abdominal pressure during urodynamic evaluation. Br J Urol 1987; 59: 529–532.
Dmochowski R . Cystometry. Urol Clin North Am 1996; 23: 243–252.
McGuire EJ, Woodside JR, Borden TA, Weiss RM . Prognostic value of urodynamic testing in myelodysplastic patients. J Urol 1981; 126: 205–209.
Van Arsdalen KM, Hackler RH . Transureteroureterostomy in spinal cord injury patients for persistent vesicoureteral reflux: 6 to 14-year followup. J Urol 1983; 129: 1117–1119.
Klein LA . Urge incontinence can be a disease of bladder sensors. J Urol 1988; 139: 1010–1014.
Wyndaele JJ . Are sensations perceived during bladder filling reproducible during cystometry? Urol Int 1992; 48: 299–301.
O'Donnell PD, Hawkins WH . Effects of subcutaneous bethanechol on bladder sensation during cystometry. Urology 1993; 41: 452–454.
De Wachter S, Wyndaele JJ . Does bladder tone influence sensation of filling and electro-sensation in the bladder? A blind controlled study in young healthy volunteers using bethanechol. J Urol 2001; 165: 802–804.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Ersoz, M., Akyuz, M. Bladder-filling sensation in patients with spinal cord injury and the potential for sensation-dependent bladder emptying. Spinal Cord 42, 110–116 (2004). https://doi.org/10.1038/sj.sc.3101525
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101525
Keywords
This article is cited by
-
Urodynamic findings and therapeutic approaches for neurogenic lower urinary tract dysfunction in patients with thoracic spinal cord injury
Irish Journal of Medical Science (1971 -) (2023)
-
Combining different evaluations of sensation to assess the afferent innervation of the lower urinary tract after SCI
Spinal Cord (2021)
-
Ambulatory urodynamic monitoring assessment of dorsal genital nerve stimulation for suppression of involuntary detrusor contractions following spinal cord injury: a pilot study
Spinal Cord Series and Cases (2020)
-
The use of the neurologic exam to predict awareness and control of lower urinary tract function post SCI
Spinal Cord (2017)
-
The management of neurogenic lower urinary tract dysfunction after spinal cord injury
Nature Reviews Urology (2016)