Abstract
Study design: Follow-up study of seven individuals with spinal cord injury (SCI) who completed a 9-month randomized control trial (RCT) of exercise training.
Objective: In a 9-month RCT conducted in our lab, individuals with SCI who participated in a twice-weekly supervised exercise training reported greater perceived quality of life (PQOL), and less stress and pain than a nonexercising control cohort. The present follow-up study examined the voluntary continuation of exercise training after the study ended and the persistence of the accrued psychosocial benefits.
Setting: Centre for Health Promotion and Rehabilitation, McMaster University, Hamilton, Ontario, Canada.
Methods: Five men and two women (age 42.3±3.6 years) with SCI (C5–T12; ASIA A–D 12.7±8.2 years postinjury) were invited to continue supervised exercise training twice weekly at the completion of the 9-month RCT. Exercise adherence, PQOL, stress and bodily pain were measured at a 3-month follow-up and were compared to values obtained at baseline, and at 3, 6 and 9 months during the intervention.
Results: There was a significant decrease in adherence at the 3-month follow-up compared to the overall 9-month adherence rate (42.7 versus 80.6%, respectively; P<0.01). There was also a significant decrease in PQOL (P<0.05) and a trend for increased pain (P=0.07) and stress (P=0.12), at follow-up compared to the end of the 9-month trial. Finally, there was a significant negative correlation between pain at the conclusion of the RCT and exercise adherence over the 3-month follow-up period (r=−0.91; P<0.01).
Conclusions: These findings emphasize the importance of continued exercise adherence to the maintenance of exercise-related increases in psychological well-being among individuals with SCI.
Similar content being viewed by others
Introduction
While muscle paralysis may be the most obvious consequence of spinal cord injury (SCI), individuals with paraplegia and tetraplegia are also susceptible to several other secondary health complications. Such health issues include a propensity to chronic pain and stress,1 and a reduction in perceived quality of life (PQOL).2 To emphasize the importance of these issues, it should be noted that several mechanisms may be responsible for the existence of chronic pain,3,4 which may coexist above, at and below the level of the SCI.5 The existence of this pain has been found to increase the already heightened stress levels in individuals with SCI and further decrease their quality of life.1 Finally, the perceptions of this pain may be quite intense. For example, in a survey of 200 individuals with SCI, 25% of the respondents described their pain as severe to extreme, 44% stated that their pain interfered with daily activities, and 37% of the individuals with higher level injuries and 23% of the individuals with lower level injuries reported that they would trade pain relief for loss of bladder, bowel or sexual function.6
In a 9-month randomized control trial (RCT) conducted in our centre, we found that regular aerobic and resistance training may reduce these health concerns in individuals with SCI regardless of the level or completeness of the injury.7 We also found that despite their immobility, dependence on others for transportation, and high susceptibility to illness, individuals with SCI may adhere to an exercise training programme outside of their own home with rates comparable to those found for the population at large. Specifically, their dropout rate over the 9-month RCT (48%) was very similar to the 50% dropout rate frequently cited for the able bodied.8 Further, those who completed the 9-month training programme had an attendance rate of 82.5%.
While these results were encouraging, it was unknown whether or not our participants would make the lifestyle change of adopting regular exercise into their weekly routine following completion of the study. Adherence to exercise is an important issue for individuals with SCI since they are at an increased risk of various secondary health complications, such as cardiovascular disease9 and type II diabetes,10 which are somewhat reversible with exercise training.11,12 Further, if their exercise habits became less regular, it was unknown how long their previously accrued benefits, in terms of pain and stress reduction and enhanced PQOL, would persist. The purpose of the present follow-up study was, therefore, to (i) determine the level of exercise adherence in a sample of individuals with SCI following their completion of a 9-month exercise training study, (ii) determine how long the previously accrued psychosocial benefits, such as pain and stress reduction and enhanced PQOL, would persist despite the expected reductions in exercise adherence, and (iii) make a preliminary examination of what factors may predict continued exercise adherence in this sample population.
Methods
Seven individuals (five male, two female subjects; age 42. 3 years) with chronic SCI (C5–T12; ASIA A–D; 3–23 years postinjury) participated in the present follow-up study. Participant characteristics are summarized in Table 1. All participants had previously completed a 9-month RCT in our laboratory examining the effects of exercise training on strength, arm ergometry performance and psychological well-being.7
In brief, all participants were in the intervention group of a much larger (n=34; 21 exercisers, 11 of whom successfully completed the 9 months of training; 13 sedentary controls, 12 of whom completed the study) supervised, progressive exercise study at a frequency of twice per week. Each session lasted approximately 90–120 min and involved a warm-up (wheeling and stretching), arm ergometry (approximately 15–30 min at a Borg (1–10 scale) rating13 of 3–4) and resistance training (three sets per exercise at approximately 70–80% of their one repetition maximum). Outcome measures, which included strength, arm ergometry performance and selected indices of psychological well-being, were tested at baseline, and after 3, 6 and 9 months of exercise training.
Following the completion of this RCT, all participants were invited to continue supervised exercise training in our accessible facility as they desired. Although 11 individuals successfully completed the 9 months of exercise training, only those who were not about to enrol in a subsequent exercise training study (utilizing body-weight supported treadmill training) were eligible for follow-up. Thus, seven individuals were included in the present investigation. It is important to note that these seven individuals were not disinterested in the subsequent exercise study, or unmotivated in general. They were simply ineligible because of (i) the completeness of their injury (ASIA A) or (ii) the time at which they completed the 9-month RCT, as this was not constant for all participants. It is also important to note that transportation to our training facility was not provided for any of our participants either during the 9-month RCT or during the present follow-up investigation. Finally, participants were unaware that their attendance was being monitored during the 3-month follow-up time period. Follow-up outcome measures included:
-
i)
Exercise adherence, defined as the percentage of available sessions that were attended (at a maximum of two per week). Attendance was monitored by the investigators, rather than being self-reported.
-
ii)
PQOL, as determined by the 11-item Perceived Quality of Life Scale,14 with four additional SCI-relevant items.15
-
iii)
Pain, as determined by two pain items from the Short-Form 36-Item Health Survey (SF-36).16
-
iv)
Stress, as determined by the 14-item Perceived Stress Scale (PSS).17
All participants gave informed consent before the administration of questionnaires. The study protocol was approved by the McMaster Research Ethics Board (MREB).
Results
Effects of the 9-month exercise intervention: A review
First, to summarize briefly the findings of the 9-month exercise training study, those in the intervention group (n=11) reported significantly less pain and stress after exercise training, and scored higher than the nonexercising controls (n=12) in overall quality of life (P<0.05).7 Of greater relevance however, a repeated measures analysis of covariance (ANCOVA), adjusted for baseline scores, showed that the seven individuals included in the present follow-up study had significant increases in quality of life after 9 months of exercise training (P=0.05), although they made no significant changes in pain or stress. This relative maintenance of perceived pain and stress, however, may be seen as beneficial, as the nonexercising control group showed nonsignificant increases in both measures over the 9-month period.
Exercise adherence and psychological well-being at follow-up
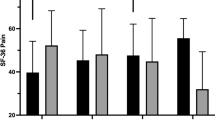
A repeated measures analysis of variance (ANOVA), with post hoc t-tests indicated that over the course of the 3-month follow-up period, there was a significant decrease in exercise adherence compared to the overall 9-month adherence rate (42.7 versus 80.6%, respectively; P<0.01). Separate repeated measure ANCOVAs, adjusted for baseline scores with post hoc t-tests, indicated a significant decrease in PQOL (P<0.05) (Figure 1) and a trend for increased pain (P=0.07) and stress (P=0.12) at 3-months follow-up compared to the end of the 9-month trial (Figure 2).
Finally, bivariate correlations indicated that there was a significant negative correlation between pain scores at the conclusion of the 9-month trial and adherence during the 3-month follow-up (r=−0.91; P<0.01) (Figure 3).
The relation between perceived pain at the conclusion of the 9-month exercise training study and exercise adherence during the 3-month follow-up period. The correlation was significant and negative (r=−0.91; P<0.01); thus, the greater one's pain at the conclusion of the 9-month RCT, the less likely he or she would be to adhere to exercise over the following 3 months
Discussion
The three main findings of this follow-up study, as they relate to our initial objectives are as follows. First, exercise adherence significantly decreased in our sample of participants following their completion of the 9-month exercise study. Second, any benefits that were accrued during the 9-month exercise trial, in terms of psychological well-being (ie improved PQOL and a relative maintenance of pain and stress), were not maintained when the frequency of exercise training sessions decreased. Third, our findings suggest that pain may be a potential predictor of whether individuals with SCI will adhere to exercise training outside of the research setting. This was evidenced by the significant negative correlation between pain at the conclusion of the 9-month trial and adherence during the 3-month follow-up, that is, the greater one's pain at the conclusion of the 9-month RCT, the less likely he or she would be to adhere to exercise over the following 3 months. Although our investigation was limited by a small, heterogeneous group of participants, our main findings were pronounced and significant, and therefore, we are confident regarding their validity.
These findings are relevant as they give insight into the exercise behaviour of individuals with SCI outside of the laboratory setting. To expand, although the high exercise adherence rates that were found in our initial RCT (for those who completed the entire 9 months) were extremely encouraging,7 it now seems apparent that the same compliance may not necessarily carry over to real-world practice. It is unclear why exercise participation decreased so dramatically in the 3-month follow-up to our RCT. It is likely that these seven individuals felt a sense of obligation and commitment to the study investigators that motivated them to exercise more frequently during the 9-month RCT than they would have spontaneously. Or perhaps, the presence of a goal (ie completing the 9-month study) was somewhat motivating during the 9-month RCT, and unfortunately similar goals were not so apparent afterwards. What we do know, however, is that perceptions of pain played a major role on exercise behaviours during the 3-month follow-up period. In spite of the fact that the individuals in the exercise group reported less pain after the 9-month RCT than did the nonexercising controls, they were not pain free.7 Our results suggested that the degree of pain after the 9-month RCT accounted for 83% of the variability in exercise adherence in our seven participants during the 3-month follow-up. When examining the relation between pain and exercise adherence, it is difficult to determine whether perceptions of pain cause decreases in exercise adherence or, alternately, if decreases in exercise participation cause increases in the perception of pain. However, in the present study, the pain measure in question (ie at 9 months) preceded the follow-up period, suggesting that it was actually the perceptions of pain that decreased exercise adherence, and not vice versa. Additional research, however, is necessary to further clarify this relation.
Given that perceptions of pain may play such a large role in the exercise behaviours of individuals with SCI, efforts should now concentrate on methods of addressing and alleviating pain in this population. Such pain relief may not only increase the quality of life, but it may also, as our findings suggest, increase the likelihood of exercise adherence in individuals with SCI. This increase in exercise participation may then, in turn, partially alleviate many of the secondary health complications associated with SCI and promote a better quality of life.
Conclusions
In individuals with SCI, continued exercise adherence may be particularly challenging, but necessary in order to maintain exercise-related increases in psychological well-being. In addition, pain may be a significant barrier to exercise adherence in individuals with SCI. Future studies are needed to investigate the role of pain relief as an agent to promote exercise adherence in this population.
References
Rintala DH et al. Chronic pain in a community-based sample of men with spinal cord injury: prevalence severity and relationship with impairment, disability, handicap, and subjective well-being. Arch Phys Med Rehabil 1998; 79: 604–614.
Westgren N, Levi R . Quality of life and traumatic spinal cord injury. Arch Phys Med Rehabil 1998; 79: 1433–1439.
Eide PK . Pathophysiological mechanisms of central neuropathic pain after spinal cord injury. Spinal Cord 1998; 36: 601–612.
Ragnarsson KT . Management of pain in persons with spinal cord injury. J Spinal Cord Med 1997; 20: 186–199.
Siddall PJ, Taylor DA, Cousins MJ . Classification of pain following spinal cord injury. Spinal Cord 1997; 35: 69–75.
Nepomuceno C et al. Pain in patients with spinal cord inury. Arch Phys Med Rehabil 1979; 60: 605–609.
Hicks AL et al. Long-term exercise training in persons with spinal cord injury: effects on strength, arm ergometry performance and psychological well-being. Spinal Cord 2003; 41: 34–43.
Dishman RK . Increasing and maintaining exercise and physical activity. Behav Ther 1989; 22: 345–378.
DeVivo MJ, Black KJ, Stover SL . Causes of death during the first 12 years after spinal cord injury. Arch Phys Med Rehabil 1993; 74: 248–254.
Bauman WA, Spungen AM . Disorders of carbohydrate and lipid metabolism in veterans with paraplegia or quadriplegia: a model of premature aging. Metabolism 1994; 43: 749–756.
Brenes G et al. High density lipoprotein cholesterol concentrations in physically active and sedentary spinal cord injured patients. Arch Phys Med Rehabil 1986; 67: 445–450.
Stewart BG et al. Body-weight support treadmill training (BWSTT) improves glucose tolerance in spinal cord injured (SCI) individuals. Fed Am Soc Exp Biol J 2002; 16: A449.
Borg GAV . Psychological bases of perceived exertion. Med Sci Sports Exerc 1970; 14: 377–381.
Patrick D, Danis M, Southerland LI, Hong G . Quality of life following intensive care. J Gen Int Med 1988; 3: 218–223.
Martin KA et al. Using exercise to enhance subjective well-being among people with spinal cord injury: the mediating influences of stress and pain. Rehabil Psychol (in press).
Ware JE, Sherbourne CD . The MOS 36-item short form health survey (SF-36). Conceptual framework and item selection. Med Care 1992; 30: 473–483.
Cohen S, Kamarch T, Mermelstein R . A global measure of perceived stress. J Health Soc Behav 1983; 24: 385–396.
Acknowledgements
We gratefully acknowledge the Ontario Neurotrauma Foundation for their financial support and the training assistance provided by the many undergraduate and graduate Kinesiology students. DS Ditor was the recipient of a studentship from the Ontario Neurotrauma Foundation.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Ditor, D., Latimer, A., Martin Ginis, K. et al. Maintenance of exercise participation in individuals with spinal cord injury: effects on quality of life, stress and pain. Spinal Cord 41, 446–450 (2003). https://doi.org/10.1038/sj.sc.3101487
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101487
Keywords
This article is cited by
-
Perceptions of a self-guided web-based exercise programme for shoulder pain after spinal cord injury: A qualitative study
Spinal Cord (2023)
-
Acute Intermittent Hypoxia as a Potential Adjuvant to Improve Walking Following Spinal Cord Injury: Evidence, Challenges, and Future Directions
Current Physical Medicine and Rehabilitation Reports (2020)
-
Psychophysiological Stress Response of a Paralympic Athlete During an Ultra-Endurance Event. A Case Study
Journal of Medical Systems (2019)
-
Health status of regularly physically active persons with spinal cord injury
Spinal Cord Series and Cases (2017)
-
Evaluation and Management of SCI-Associated Pain
Current Pain and Headache Reports (2016)