Abstract
Numerous findings indicate alterations in brain serotonin systems in obsessive-compulsive disorder (OCD). We investigated the in vivo availability of thalamus–hypothalamus serotonin transporters (SERT) in patients with DSM-IV OCD who displayed prominent behavioral checking compulsions (OC-checkers). Four hours after injection of [123I]-2β-carbomethoxy-3β-(4-iodophenyl)tropane ([123I]-β-CIT), single photon emission computed tomography (SPECT) scans were performed in 24 medication-free non-depressed OC-checkers and 24 age- and gender-matched healthy controls. For quantification of brain serotonin transporter availability, a ratio of specific to non-displaceable [123I]-β-CIT brain binding was used (V″3=(thalamus and hypothalamus−cerebellum)/cerebellum). Drug-free non-depressed OC-checkers showed an 18% reduced brain serotonin transporter availability in the thalamus and hypothalamus, as compared with healthy control subjects (1.38±0.19 vs 1.69±0.21; p<0.001). There was a strong negative correlation between severity of OC symptomatology (Y-BOCS scores) and SERT availability (r=−0.80; p<0.001). Moreover, we found a significant positive correlation between illness duration and serotonin transporter availability (r=0.43; p<0.05). This first report of significantly reduced [123I]-β-CIT binding in the thalamus–hypothalamus region in OC-checkers suggests reduced brain serotonin transporter availability, which is more pronounced with increased severity of OC symptomatology and short duration of illness. The results provide direct evidence for an involvement of the serotonergic system in the pathophysiology of OCD.
Similar content being viewed by others
INTRODUCTION
Obsessive-compulsive disorder (OCD) is a clinically defined condition characterized by intrusive and distressing thoughts, images or impulses (obsessions), and by repetitive mental or behavioral acts (compulsions).
The past two decades have seen advances in neuropsychiatric research providing growing evidence supporting a neurobiological basis of OCD (Goodman et al, 1992; Hollander et al, 1992; Insel, 1992; Prichep et al, 1993; Saxena et al, 1998; Saxena and Rauch, 2000). This is currently believed to involve a disturbance in frontocortical–subcortical neuroanatomical pathways, including the orbitofrontal cortex, the basal ganglia, and the thalamus–hypothalamus, and neurochemical abnormalities of central serotonergic functioning. The hypothesis of a serotonergic dysfunction in OCD has arisen mainly as an indirect conclusion based on neuropharmacologic studies supporting a high selectivity of drug response in OCD to serotonin reuptake inhibiting agents (Leonard et al, 1988; Goodman et al, 1990). Radioligands used in neuroimaging techniques allow for the study of central neurotransmitter systems. [123I]-2β-carbomethoxy-3β-(4-iodophenyl)tropane ([123I]-β-CIT), a radiotracer with high affinity to monoamine transporters (Innis et al, 1991; Boja et al, 1992), can be used to mark the central dopamine (DAT) and serotonin transporters (SERT) of the human brain in vivo with the aide of single photon emission computed tomography (SPECT) (Brücke et al, 1993; Kuikka et al, 1993; Pirker et al, 2000). β-CIT accumulates in specific areas of the brain, these being primarily striatal, diencephalic, midbrain, and brainstem regions (Innis et al, 1991; Laruelle et al, 1993). The density of DAT in the striatum is much higher than that of SERT. In vivo displacement studies in nonhuman primates have demonstrated that β-CIT uptake in the striatum consists predominantly of its binding to DAT (Laruelle et al, 1993). β-CIT uptake in the remaining regions (thalamus, hypothalamus, midbrain, and pons) is believed to be mainly related to SERT availability as demonstrated by in vivo displacement and autoradiographic post-mortem studies (Laruelle et al, 1993; Staley et al, 1994; Pirker et al, 1995).
Clinical studies in psychiatric research using β-CIT and SPECT have shown increased SERT availability in acutely abstinent cocaine-dependent patients (diencephalon and brainstem; Jacobsen et al, 2000) and in OCD patients (midbrain-pons; Pogarell et al, 2003), whereas reduced SERT status has been revealed in patients with major depression (brainstem; Malison et al, 1998), alcoholism (brainstem; Heinz et al, 1998b), seasonal affective disorder (thalamus–hypothalamus; Willeit et al, 2000), bulimia (thalamus–hypothalamus; Tauscher et al, 2001), and OCD (midbrain–brainstem; Stengler-Wenzke et al, 2004). Thus, the only two studies to ever demonstrate specific serotonergic abnormities in patients with OCD to date were, as previously mentioned, that of Pogarell et al (2003), which showed a 25% increase in SERTs in the midbrain–pons area and that of Stengler-Wenzke et al (2004), which revealed a significantly reduced SERT availability in the midbrain and brainstem.
The aim of the present study was to investigate serotonergic function in the thalamus–hypothalamus area in untreated OCD patients by measuring SERT availability with β-CIT SPECT.
As patients diagnosed with obsessive-compulsive disorder often represent a very heterogeneous group clinically, only OC-checkers were enrolled in this study in order to obtain as homogeneous a patient group as possible. These OC-checkers, who were medication-free and who were only included if they did not display any clinically relevant depressive symptomatology, were compared to a group of healthy control subjects.
PATIENTS AND METHODS
Subjects
The study population consisted of 24 non-depressed patients diagnosed with a DSM-IV 300.3 OCD (American Psychiatric Association, 1994), 11 female patients, 13 male patients, ranging in age from 19 to 57 years and 24 age- and gender-matched healthy control subjects ranging in age from 21 to 60 years. The mean age was 37.5±11.8 years in the patient group and 36.0±13.7 years in the healthy control group (Table 1). All OCD patients were OC-checkers, whose main OC symptomatology was required to consist of compulsive checking rituals. They were consecutively recruited from the specialized outpatient clinic for OCD of the Department of Psychiatry, University Hospital of Vienna. Both patients and controls were non-smokers. Alcohol consumption was not allowed from 1 week before the day of the tracer injection until completion of the study.
Demographic and clinical information on the longitudinal course of illness, previous treatment attempts, and other psychiatric diagnoses were obtained using a semistructured clinical interview based on DSM-IV and by reviewing medical records and contacting previous psychiatrists directly. Patients with present or past substance abuse or present or past psychiatric diagnoses other than OCD were not included in the study. All patients were diagnosed by consensus of the authors using DSM-IV criteria for OCD and had displayed prominent behavioral checking compulsions for a duration of at least 2 years. All patients had been free of psychotropic agents for at least 6 months before the investigation. No patient had been treated with other somatic treatments (eg electroconvulsive therapy). Urine β-HCG tests were performed to exclude pregnancy in female subjects.
Further inclusion criteria were a score on the Yale–Brown Obsessive-Compulsive Scale (Y-BOCS) (Goodman et al, 1989a, 1989b) of at least 16 and a maximum Hamilton Depression Scale score of 13 (HAMD17) (Hamilton, 1960). OCD patients with a main OC symptomatology other than compulsive checking rituals or with depressive symptomatology were excluded from the study.
The rating scales were administered immediately before SPECT imaging and yielded mean Y-BOCS scores of 25.1±5.0 (range 16–35) and mean HAMD17 scores of 6.4±3.02. The mean age at onset of obsessive-compulsive symptoms, as reported by the patients, was 21.8±8.8 years and the mean duration of illness 15.6±11.1 years (Table 1).
The 24 age- and gender-matched healthy volunteers, who had not received psychotropic medication within the previous year, served as the control group. These control subjects were without past or present neurological or psychiatric disorder, and had no history of neurological or psychiatric disorders in their first-degree relatives, according to SCID-1/NP (Structured Clinical Interview for DSM-IV, Non-patient Edition; First et al, 1996). The study was approved by the local ethics committee. Written informed consent for participation in this study was obtained from each subject after the procedure had been fully explained by the research physicians of both the Department of Psychiatry and the Department of Nuclear Medicine.
SPECT Imaging and Data Analysis
[123I]-β-CIT was synthesized according to the method of Neumeyer et al (1991) with several modifications described earlier (Brücke et al, 1993). After blockade of thyroid uptake with 600 mg sodium perchlorate orally 30 min before tracer application, subjects received a mean dose of 131 MBq (±17 SD; 3.5 mCi±0.4 SD) [123I]-β-CIT intravenously as a single bolus. The SPECT studies were performed 4 h after tracer injection using a triple-headed rotating scintillation camera (Siemens Multispect 3, Knoxville, TN, USA) with a resolution of 9 mm full-width at half-maximum in the transaxial plane. Camera heads were equipped with medium energy collimators. The subject's head was placed in the head holder by means of a laser beam system with the infraorbitomeatal plane aligned perpendicular to the rotational axis. A chin-strap device was used to minimize movement of the head during the scan. Data acquisition and analysis were performed using the ICON software package for the Siemens Multispect 3 camera. For each scan, a total of 180 frames were collected in a step and shoot mode. SPECT imaging lasted for 20 min (20 s per frame).
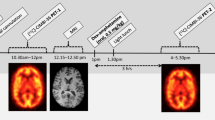
Cross-sections (3.5 mm thick), oriented parallel to the canthomeatal plane, were reconstructed by filtered back projection (Butterworth filter, cutoff frequency 0.7, order 7) in 128 × 128 matrices. Attenuation correction was performed assuming uniform attenuation within an ellipse drawn around the head contour (attenuation coefficient=0.120/cm). Circular regions of interest (ROIs) were placed in a midline area corresponding to the thalamus and hypothalamus (size: 32 voxels each; voxel size 3.5 × 3.5 × 3.5 mm3) on 5–6 consecutive axial sections (Figure 1). Irregular ROIs were drawn in areas corresponding to the left and right cerebellar hemisphere (60 voxels each). All ROIs were drawn with the help of a brain atlas (Talairach and Tournoux, 1988) by one and the same examiner, who was blind to the clinical status of the subjects. Values of the four circular midline ROIs with the highest count rate (usually from one slice below the maximum of striatal binding downwards; area corresponding to thalamus and hypothalamus) were pooled together to form a ‘thalamus–hypothalamus’ region (constant volume of interest 5.5 cm3) and the average counts/voxel were calculated. Values of both cerebellar ROIs in three consecutive axial slices of maximal cerebellar activity were averaged. Cerebellar activity was assumed to represent nonspecific bound and free activity because it is known that the density of DATs and SERTs in the cerebellum is very low (Bäckström et al, 1989; De Keyser et al, 1989).
Axial [123I]-β-CIT SPECT images at the level of the striatum (left) and cerebellum (right) with ROIs in the thalamus (left) and the cerebellar hemispheres (right). Image acquisition 4 h post-injection. The level of radioactivity is color coded from black (low) through green, yellow, red, and white (high) and scaled to the maximum of the study.
Ratios between mean counts in the target region (thalamus and hypothalamus) and the cerebellum were calculated. This ratio minus 1 (region/cerebellum−1), also denoted as V″3 or BP2, represents specific/non-displaceable binding and is assumed to be directly related to the binding potential at the time of equilibrium (Mintun et al, 1984; Laruelle et al, 1994; Malison et al, 1998).
Statistical Analysis
Descriptive analyses of clinical and SPECT variables were given as means and SD. t-Tests were used to compare statistical differences between OCD patients and control subjects regarding mean age and regional [123I]-β-CIT uptake. Pearson product moment correlation coefficients were calculated to study correlations between [123I]-β-CIT binding and markers for the severity of OCD such as Y-BOCS scores, duration of illness, age at onset, and age. As a control for the effects of age, gender, age at onset of OCD, duration of illness, and severity of illness, a multiple linear regression analysis was performed with thalamus–hypothalamus β-CIT binding ratios as dependent variable and age, gender, age at onset, duration of illness, and severity as independent variables. Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS version 12.0.0 for Microsoft Windows, SPSS Inc., Chicago, IL). The p<0.05 level was considered statistically significant.
RESULTS
Patients and age- and gender-matched healthy controls did not differ significantly in mean age (37.5±11.8 vs 36.0±13.7; p=0.70). The median of age was 35.0 in the patient group and 32.5 in the healthy controls, respectively. Using a non-parametric test age was likewise equally distributed in patient and control groups (z=−0.506; p=0.61; Mann–Whitney U-test).
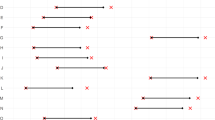
Single photon emission computed tomography investigations performed 4 h after injection of [123I]-β-CIT revealed that its uptake in the brain was significantly reduced (by 18%) in the thalamus–hypothalamus of OC-checkers, as compared with healthy control subjects (V″3 SERT: 1.38±0.19 vs 1.69±0.21, t=5.364; p<0.001***) (Table 1; Figure 2). The individual ratios of specific to non-displaceable thalamus–hypothalamus [123I]-β-CIT binding ranged from 1.01 to 1.70 and 1.43 to 2.38 in the groups of patients and healthy control subjects, respectively.
There were no substantial differences between women and men within the patient group with regard to age, age at onset, duration of illness, Y-BOCS scores, or β-CIT binding ratios (Table 1). Likewise, the women and men of the healthy control group did not differ substantially in age or β-CIT ratios (Table 1).
Correlation analyses of imaging and clinical data within the patient group showed a significant negative association between thalamus–hypothalamus β-CIT binding and obsessive-compulsive scores as assessed by Y-BOCS (r=−0.80; p<0.001***) (Figure 3). Age and age at onset did not correlate significantly to the β-CIT ratios (r=0.22; p=0.30 and r=−0.20; p=0.34, respectively).
However, we found a significant positive correlation between SERT availability in the thalamus–hypothalamus and duration of illness (r=0.43; p=0.048*) (Figure 4).
As multiple factors (severity of illness, duration of illness) seem to interfere with the SPECT measure, a multiple linear regression analysis was applied to assess the contribution of each independent variable (subject's age, gender, age at onset of OCD, OCD duration, and severity of illness) to β-CIT binding ratios. This multivariate statistical model showed that both the severity of illness and the duration of illness had significant impact on β-CIT binding (B=−0.030±0.005; t=−6.185; p<0.001 and B=0.006± 0.002; t=2.424; p<0.05 respectively); the other variables were not significant.
Within the control group there was no significant correlation between age and thalamus–hypothalamus β-CIT binding (r=−0.38; p=0.12).
DISCUSSION
The major finding of our study was a significant reduction (18%) in SERT availability in the thalamus–hypothalamus region in 24 OCD patients as compared to 24 age- and gender-matched healthy control subjects.
To the authors' knowledge, there have been four studies investigating SERT availability in OCD patients published up to now: one PET study and three β-CIT SPECT studies. These previous studies produced conflicting results: Simpson et al (2003) performed a PET study on 11 patients and 11 matched healthy subjects using the selective SERT ligand [11C]McN 5652. Neither region of interest analysis nor voxel-wise analysis of the data revealed changes in SERT availability. Likewise, one [123I]-β-CIT SPECT study of 15 OCD patients found no changes in SERT availability in the thalamus, midbrain, or pons as compared to matched healthy subjects (van der Wee et al, 2004). Pogarell et al (2003) investigated SERT availability in nine OCD patients with β-CIT SPECT. OCD patients showed a 25% higher SERT availability in the midbrain–pons region compared with healthy controls. By contrast, another recent β-CIT SPECT study in 10 OCD patients found significantly reduced SERT availability in the midbrain and brainstem and a trend towards lower β-CIT binding ratios in the thalamic–hypothalamic area (Stengler-Wenzke et al, 2004).
Differences in methodology and patient sampling make a direct comparison of these studies difficult. Sample sizes were considerably smaller than in the present study. All previous studies included heterogeneous groups of OCD patients reducing the chance of finding abnormalities related to a particular subtype of OCD, for example, with predominant compulsions. Moreover, there were considerable differences in severity of OCD in the patient groups as well. Only van der Wee et al (2004) presented a clear cutoff score of 16 in recruiting subjects; the other studies did not use inclusion cutoff scores. The mean values of the Y-BOCSs in the individual studies ranged from 20 to 30. It is noteworthy that significant reductions in β-CIT binding in SERT-rich brain areas were only found in studies with a mean Y-BOCS score ⩾25. Pogarell et al (2003) also included OCD patients with comorbid depressive symptomatology. It is known that depression influences the SERT status (Malison et al, 1998; Willeit et al, 2000). The studies also varied as to their control subjects. Only in the investigations of Simpson et al (2003), van der Wee et al (2004), and in our study were the groups matched for age and gender. Pogarell et al (2003) chose the occipital cortex as reference region, whereas van der Wee et al (2004), Stengler-Wenzke et al (2004), and our study used the cerebellum. Our choice was based on the fact that SERT binding was detectable in the occipital cortex but not in the cerebellum (Bäckström et al, 1989).
Van der Wee et al (2004) revealed significantly increased striatal dopamin transporter availability in OCD. DAT binding in the substantia nigra contributes to midbrain β-CIT binding (Staley et al, 1994) and may thus confound SERT measurement in this region.
Another technical difference between the studies is the different SPECT acquisition times. SPECT imaging was performed 24 h after injection of β-CIT in the studies by Pogarell et al (2003) and Stengler-Wenzke et al (2004) and 4 h post-injection by van der Wee et al (2004) and in the study at hand. Kinetic studies of β-CIT uptake in SERT-rich brain areas showed a peak in tracer uptake in the thalamus–hypothalamus at 4 h post-injection, followed by stable uptake up to 10 h, and a slow decrease up to 24 h post-injection. Owing to a concomitant slow but steady decline in uptake in the cerebellum from 4 h on, a higher stability of binding ratios in SERT-rich brain areas was observed on day 2, suggesting that a state of true equilibrium is reached between 20 and 24 h (Pirker et al, 2000). This suggests that SPECT imaging of SERTs with β-CIT should ideally be performed during this time period. However, conditions are close to true equilibrium between 4 and 10 h postinjection. Pirker et al (1995) compared β-CIT binding in the thalamus–hypothalamus area in depressed patients treated with the SSRI citalopram with a group of control subjects of comparable age and were able to demonstrate a highly significant binding reduction in patients on citalopram. The binding reduction of β-CIT in the thalamus–hypothalamus area in patients treated with citalopram was virtually the same at 4 and at 20 h postinjection (ratios (thalamus−hypothalamus/cerebellum)−1: −47 vs −45%, respectively) (Pirker et al, 1995), suggesting that both time points are feasible for the measurement of SERTs with [123I]-β-CIT SPECT.
For a long time there has been experimental data supporting the hypothesis that serotonin plays a special role in OCD (Zohar et al, 1987, 2004; Goodman et al, 1992). Disturbances of neurotransmitter modulation seem to be relevant in OCD (Baumgarten and Grozdanovic, 1998) because of the clinical efficacy of drugs that act on serotonin re-uptake sites (for a review, see Cartwright and Hollander, 1998).
The significant reduction of β-CIT binding in our investigation was in line with earlier studies in psychiatric disorders with suspected serotonergic dysfunction (eg major depression, seasonal affective disorder, bulimia), which showed a decrease in SERT availability (Malison et al, 1998; Willeit et al, 2000; Tauscher et al, 2001). The reduced SERT availability in our OCD patients (checking subtype) may reflect a low serotonin tone and is consistent with the serotonin hypothesis of OCD. However, it remains unclear whether the reduced binding of [123I]-β-CIT in this SERT-rich brain region represents a genuine reduction of serotonergic neurons that may result in low serotonin levels, or represents a reduced availability of intact serotonin binding sites for the radiotracer owing to an increased level of synaptic serotonin. We hold the latter for improbable owing to the mode of action of SSRIs, which enhance synaptic serotonin levels. It might be speculated, however, that transporter availability is closely correlated with the affinity of re-uptake sites for transporter-binding drugs. As this feature would permit the use of [123I]-β-CIT SPECT for monitoring therapeutic response, it would be valuable to further explore this possibility.
Interestingly, Pogarell et al (2003) found an elevated SERT availability in midbrain—pons of OCD patients (mixed subtypes), which was interpreted as an increased SERT number with higher capacity or an increased binding of the radiopharmaceutical to SERT owing to lower endogenous serotonin levels. On the basis of our data, it seems more likely that downregulation of SERT evolves to preserve a high tone of intrasynaptic serotonin as it is effectively targeted in SSRI treatments.
Recent investigations found that different subtypes of OCD resulted in variations in therapy outcome. Severity of OC symptomatology and duration of illness are also linked with therapy outcome (Mataix-Cols et al, 1999; Shetti et al, 2005; Storch et al, 2006). Both the severity and the duration of illness had significant impact on β-CIT binding in our study. Thus, it is conceivable that owing to the correlations with severity and duration of illness, β-CIT binding could be identified as a predictor for the course of illness. Further studies are necessary to investigate this.
In our investigation we found a significant negative correlation between the severity of OC-symptomatology (Y-BOCS scores) and β-CIT binding. This indicates that patients with a more pronounced severity of OC symptomatology will show more significantly reduced SERT availability. This result is in agreement with a β-CIT SPECT study in patients with Tourette's syndrome (TS), a disorder characterized by chronic tics often accompanied by obsessive-compulsive symptoms (OCD-spectrum disorder). Heinz et al (1998a) found a significant negative correlation between midbrain β-CIT binding and vocal tic severity in these patients. Correlations between β-CIT ratios and OCD severity (Y-BOCS scores) were also calculated in all previously mentioned β-CIT OCD studies. However, no significant correlations were found in any of these investigations. Again one must keep in mind that these negative results are most likely dependent upon the heterogeneity of the OCD patients, because not only our study with a homogeneous subtype but also that of Heinz et al (1998a) in TS patients showed significant correlations.
Another finding of our study was that we observed a significant association between duration of illness and β-CIT binding. Those patients with a shorter duration of illness displayed the most markedly reduced thalamic-hypothalamic SERT availability. An explanation for this finding could be that reduced β-CIT binding is a marker of illness that disappears substantially in the course of disease owing to adaptive processes or therapeutic interventions (eg treatment with cognitive-behavior therapy (CBT) or pharmacological treatment). As [123I]-β-CIT is displaceable by synaptic levels of serotonin, another explanation would also be possible, that is, that reduced synaptic serotonin occurs with increased disease duration. Furthermore, no other variable correlated to [123I]-β-CIT binding indices.
Several assumptions form the basis for attempting to measure SERT availability with [123I]-β-CIT and SPECT. First of all, the ligand must be selective for those transporters. In vivo and in vitro studies showed that the thalamus–hypothalamus contains negligible amounts of dopamine transporters (Laruelle et al, 1993; Staley et al, 1994). In addition to binding to SERT and DAT, β-CIT has a relatively high affinity for norepinephrine transporters (NET). Autoradiography studies in the rat showed high densities of NET in the thalamus and hypothalamus, locus coeruleus, and other brain stem nuclei (Tejani-Butt, 1992). In a PET study in non-human primates, 50% of β-CIT binding in the thalamus was able to be displaced by the SERT ligand, citalopram. A displacement of approximately 50% of β-CIT binding in this area was also observed with the non-selective NET ligands desipramine and mazindol, indicating that thalamic uptake represents binding to both SERTs and NETs (Farde et al, 1994). However, in another in vivo displacement study in primates, citalopram markedly reduced β-CIT uptake in midline regions whereas the selective norepinephrine uptake inhibitor maprotiline had no affect on brain β-CIT uptake (Laruelle et al, 1993). In line with this result, in an autoradiographic study of the post-mortem human brain, β-CIT binding in the thalamus and hypothalamus was able to be completely displaced by citalopram, indicating that β-CIT binding in these areas is almost exclusive to SERT (Staley et al, 1994). In contrast to previous findings of high thalamic NET density in rat brain, an autoradiographic study in the cat found only weak labeling of all but one small thalamic subnuclei with the NET-selective ligand nisoxetine (Charnay et al, 1995), suggesting that some of the inconsistencies regarding the displacement of thalamic β-CIT binding in the literature may be owing to interspecies differences in NET density. As a matter of fact, a recent autoradiographic study in the human brain using the selective NET ligand (S,S)-[18F]FMeNER-D2 failed to detect specific binding in the thalamus (Schou et al, 2005). In summary, data on the contribution of NET binding to the β-CIT signal in the thalamus are inconsistent, whereas evidence clearly suggests that the major part of the signal in this area represents SERT binding. Changes in NET availability may have contributed to our observation of thalamic–hypothalamic β-CIT binding in OCD. However, evidence favours alterations in SERT availability as the explanation for our observations.
The reduced SERT availability observed in our patient group most likely indicates a reduced density of SERT in the thalamus–hypothalamus region. An alternative explanation would be increased SERT occupancy by elevated levels of synaptic serotonin in our target region. However, there is no clear evidence for altered synaptic serotonin levels in untreated OCD and the response to SSRIs in this disorder is rather suggestive of decreased than increased serotonin levels. Moreover, acute tryptophan depletion failed to worsen OCD symptoms in treated as well as in untreated OCD patients (Barr et al, 1994; Berney et al, 2006). Thus, we think that increased SERT occupancy by elevated synaptic serotonin is an unlikely explanation for the overall reduced SERT availability in our OCD group. However, a comparison between β-CIT with findings from McN- or DASB-PET using ligands which are not displaceable by synaptic serotonin will further clarify this issue in the future.
To our knowledge, ours is the first study to suggest a significant reduction in thalamic–hypothalamic SERT availability in OC-checkers as measured with [123I]-β-CIT SPECT. Reduced SERT availability, especially in the thalamus–hypothalamus, is of particular interest for future research investigating the specific pathophysiology of OCD. Owing to our results one must consider whether this is of etiological importance in the pathogenesis of OCD or whether it may be related to adaptive or compensatory regulation processes or whether it is an unrelated epiphenomenon of different etiology. Future research may aide in clarifying the processes involved in the in vivo regulation of SERT availability in OCD.
References
American Psychiatric Association (1994). Diagnostic and Statistical Manual of Mental Disorders, 4th edn. American Psychiatric Press: Washington, DC.
Bäckström I, Bergström M, Marcusson J (1989). High affinity [3H] paroxetine binding to serotonin uptake sites in human brain tissue. Brain Res 486: 261–268.
Barr LC, Goodman WK, McDougle CJ, Delgado PL, Heninger GR, Charney DS et al (1994). Tryptophan depletion in patients with obsessive-compulsive disorder who respond to serotonin reuptake inhibitors. Arch Gen Psychiatry 51: 309–317.
Baumgarten HG, Grozdanovic Z (1998). Role of serotonin in obsessive-compulsive disorder. Br J Psychiatry 173 (Suppl 35): 13–20.
Berney A, Sookman D, Leyton M, Young SN, Benkelfat C (2006). Lack of effects on core obsessive-compulsive symptoms of tryptophan depletion during symptom provocation in remitted obsessive-compulsive disorder patients. Biol Psychiatry 59: 853–857.
Boja JW, Mitchell WM, Patel A, Kopajtic TA, Carroll FI, Lewin AH et al (1992). High-affinity binding of [125I]RTI-55 to dopamine and serotonin transporters in rat brain. Synapse 12: 27–36.
Brücke T, Kornhuber J, Angelberger P, Asenbaum S, Frassine H, Podreka I (1993). SPECT imaging of dopamine and serotonin transporters with [123I]-β-CIT. Binding kinetics in the human brain. J Neural Trans Gen Sect 94: 137–146.
Charnay Y, Leger L, Vallet PG, Hof PR, Jouvet M, Bouras C (1995). [3H]Nisoxetine binding sites in the cat brain: an autoradiographic study. Neuroscience 69: 259–270.
Cartwright C, Hollander E (1998). SSRIs in the treatment of obsessive-compulsive disorder. Depress Anxiety 8 (Suppl 1): 105–113.
De Keyser J, De Backer JP, Ebinger G, Vauquelin G (1989). [3H]GBR-12935 binding to dopamine uptake sites in the human brain. J Neurochem 53: 1400–1404.
Farde L, Halldin C, Müller L, Suhara T, Karlson P, Hall H (1994). PET study of [11C] β-CIT binding to monoamine transporters in the monkey and human brain. Synapse 16: 93–103.
First MB, Spitzer RL, Gibbon M, Williams JBW (1996). Structured Clinical Interview for DSM-IV Axis I Disorders, Non-patient Edition (SCID-1/NP). American Psychiatric Press: Washington, DC.
Goodman WK, McDougle CJ, Price LH (1992). The role of serotonin and dopamine in the pathophysiology of obsessive compulsive disorder. Int Clin Psychopharmacol 7 (Suppl 1): 35–38.
Goodman WK, Price LH, Delgado PL, Palumbo J, Krystal JH, Nagy LM et al (1990). Specificity of serotonin reuptake inhibitors in the treatment of obsessive-compulsive disorder. Comparison of fluvoxamine and desipramine. Arch Gen Psychiatry 47: 577–585.
Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR et al (1989b). The Yale-Brown obsessive compulsive scale. II. Validity. Arch Gen Psychiatry 46: 1012–1016.
Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL et al (1989a). The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry 46: 1006–1011.
Hamilton M (1960). A rating scale for depression. J Neurol Neurosurg Psychiatry 23: 56–62.
Heinz A, Knable MB, Wolf SS, Jones DW, Gorey JG, Hyde TM et al (1998a). Tourette's syndrome: [123I]-β-CIT SPECT correlates of vocal tic severity. Neurology 51: 1069–1074.
Heinz A, Ragan P, Jones DW, Hommer D, Williams W, Knable MB et al (1998b). Reduced central serotonin transporters in alcoholism. Am J Psychiatry 155: 1544–1549.
Hollander E, DeCaria CM, Nitescu A, Gully R, Suckow RF, Cooper TP et al (1992). Serotonergic function in obsessive-compulsive disorder. Behavioral and neuroendocrine responses to oral m-chlorophenylpiperazine and fenfluramine in patients and healthy volunteers. Arch Gen Psychiatry 49: 21–28.
Innis R, Baldwin R, Sybirska E, Zea Y, Laruelle M, Al-Tikriti M et al (1991). Single photon emission computed tomography imaging of monoamine reuptake sites in primate brain with [123I]-β-CIT. Eur J Pharmacol 200: 369–370.
Insel TR (1992). Toward a neuroanatomy of obsessive-compulsive disorder. Arch Gen Psychiatry 49: 739–744.
Jacobsen LK, Staley JK, Malison RT, Zoghbi SS, Seibyl JP, Kosten TR et al (2000). Elevated central serotonin transporter binding availability in acutely abstinent cocaine-dependent patients. Am J Psychiatry 157: 1134–1140.
Kuikka JT, Bergström KA, Vanninen E, Laulumaa V, Hartikainen P, Länsiemies E (1993). Initial experience with single photon emission tomography using iodine-123-labelled 2β-carbomethoxy-3β-(4-iodophenyl)tropane in human brain. Eur J Nucl Med 20: 783–786.
Laruelle M, Baldwin RM, Malison RT, Zea-Ponce Y, Zoghbi SS, Al-Tikriti M et al (1993). SPECT imaging of dopamine and serotonin transporters with [123I]-β-CIT: pharmacological characterization of brain uptake in nonhuman primates. Synapse 13: 295–309.
Laruelle M, Wallace E, Seibyl JP, Zea-Ponce Y, Zoghbi SS, Neumeyer JL et al (1994). Graphical, kinetic, and equilibrium analyses of in vivo [123I]-β-CIT binding to dopamine transporters in healthy human subjects. J Cereb Blood Flow Metab 14: 982–994.
Leonard H, Swedo S, Rapoport JL, Coffey M, Cheslow D (1988). Treatment of childhood obsessive compulsive disorder with clomipramine and desmethylimipramine: a double-blind crossover comparison. Psychopharmacol Bull 24: 93–95.
Malison RT, Price LH, Berman R, van Dyck CH, Pelton GH, Carpenter L et al (1998). Reduced brain serotonin transporter availability in major depression as measured by [123I]-2β-carbomethoxy-3β-(4-iodophenyl)tropane and single photon emission computed tomography. Biol Psychiatry 44: 1090–1098.
Mataix-Cols D, Rauch SL, Manzo PA, Jenike MA, Baer L (1999). Use of factor-analyzed symptom dimensions to predict outcome with serotonin reuptake inhibitors and placebo in the treatment of obsessive-compulsive disorder. Am J Psychiatry 156: 1409–1416.
Mintun M, Raichle M, Kolbourn M, Wooten G, Welch M (1984). A quantitative model for the in vivo assessment of drug binding sites with positron emission tomography. Ann Neurol 15: 217–227.
Neumeyer JL, Wang S, Milius RA, Baldwin RM, Zea-Ponce Y, Hoffer PB et al (1991). [123I]-2β-carbomethoxy-3β-(4-iodophenyl)tropane (β-CIT): high-affinity SPECT radiotracer of monoamine reuptake sites in brain. J Med Chem 34: 3144–3146.
Pirker W, Asenbaum S, Hauk M, Kandlhofer S, Tauscher J, Willeit M et al (2000). Imaging serotonin and dopamine transporters with 123I-β-CIT SPECT: Binding kinetics and effects of normal aging. J Nucl Med 41: 36–44.
Pirker W, Asenbaum S, Kasper S, Walter H, Angelberger P, Koch G et al (1995). β-CIT SPECT demonstrates blockade of 5-HT uptake sites by citalopram in the human brain in vivo. J Neural Transm Gen Sect 100: 247–256.
Pogarell O, Hamann C, Pöpperl G, Juckel G, Choukèr M, Zaudig M et al (2003). Elevated brain serotonin transporter availability in patients with obsessive-compulsive disorder. Biol Psychiatry 54: 1406–1413.
Prichep LS, Mas F, Hollander E, Liebowitz M, John ER, Almas M et al (1993). Quantitative electroencephalographic subtyping of obsessive-compulsive disorder. Psychiatry Res 50: 25–32.
Saxena S, Brody AL, Schwartz JM, Baxter LR (1998). Neuroimaging and frontal-subcortical circuitry in obsessive-compulsive disorder. Br J Psychiatry 35 (Suppl): 26–37.
Saxena S, Rauch SL (2000). Functional neuroimaging and the neuroanatomy of obsessive-compulsive disorder. Psychiatr Clin North Am 23: 563–586.
Schou M, Halldin C, Pike VW, Mozley PD, Dobson D, Innis RB et al (2005). Post-mortem human brain autoradiography of the norepinephrine transporter using (S,S)-[18F]FMeNER-D2. Eur Neuropsychopharmacol 15: 517–520.
Simpson HB, Lombardo I, Slifstein M, Huang HY, Hwang DR, Abi-Dargham A et al (2003). Serotonin transporters in obsessive-compulsive disorder: a positron emission tomography study with [11C] McN 5652. Biol Psychiatry 54: 1414–1421.
Shetti CN, Reddy YC, Kandavel T, Kashyap K, Singisetti S, Hiremath AS et al (2005). Clinical predictors of drug nonresponse in obsessive-compulsive disorder. J Clin Psychiatry 66: 1517–1523.
Staley JK, Basile M, Flynn DD, Mash DC (1994). Visualizing dopamine and serotonin transporters in the human brain with the potent cocaine analogue [125I]RTI-55: In vitro binding and autoradiographic characterization. J Neurochem 62: 549–556.
Stengler-Wenzke K, Müller U, Angermeyer MC, Sabri O, Hesse S (2004). Reduced serotonin transporter-availability in obsessive-compulsive disorder (OCD). Eur Arch Psychiatry Clin Neurosci 254: 252–255.
Storch EA, Larson MJ, Shapira NA, Ward HE, Murphy TK, Geffken GR et al (2006). Clinical predictors of early fluoxetine treatment response in obsessive-compulsive disorder. Depress Anxiety 23: 429–433.
Talairach J, Tournoux P (1988). Coplanar Stereotaxic Atlas of the Human Brain. Thieme Medical: New York, NY.
Tauscher J, Pirker W, Willeit M, de Zwaan M, Bailer U, Neumeister A et al (2001). [123I]-β-CIT and single photon emission computed tomography reveal reduced brain serotonin transporter availability in bulimia nervosa. Biol Psychiatry 49: 326–332.
Tejani-Butt SM (1992). [3H]-Nisoxetine: a radioligand for quantification of norepinephrine uptake sites by autoradiography or homogenate binding. J Pharmacol Exp Ther 260: 427–436.
van der Wee NJ, Stevens H, Hardeman JA, Mandl RC, Denys DA, van Megen HJ et al (2004). Enhanced dopamine transporter density in psychotropic-naive patients with obsessive-compulsive disorder shown by [123I]-β-CIT SPECT. Am J Psychiatry 161: 2201–2206.
Willeit M, Praschak-Rieder N, Neumeister A, Pirker W, Asenbaum S, Tauscher J et al (2000). [123I]-β-CIT SPECT imaging shows reduced brain serotonin transporter availability in drug-free depressed patients with seasonal affective disorder. Biol Psychiatry 47: 482–489.
Zohar J, Kennedy JL, Hollander E, Koran LM (2004). Serotonin-1D hypothesis of obsessive-compulsive disorder: An update. J Clin Psychiatry 65 (Suppl 14): 18–21.
Zohar J, Mueller EA, Insel TR, Zohar-Kadouch RC, Murphy DL (1987). Serotonergic responsivity in obsessive-compulsive disorder. Comparison of patients and healthy controls. Arch Gen Psychiatry 44: 946–951.
Acknowledgements
We thank Mr Harald Frassine and Mr Miladin Radosaljevic, technologists, for their excellent assistance in the performance of [123I]-β-CIT SPECT procedures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zitterl, W., Aigner, M., Stompe, T. et al. [123I]-β-CIT SPECT Imaging Shows Reduced Thalamus–Hypothalamus Serotonin Transporter Availability in 24 Drug-Free Obsessive-Compulsive Checkers. Neuropsychopharmacol 32, 1661–1668 (2007). https://doi.org/10.1038/sj.npp.1301290
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1301290
Keywords
This article is cited by
-
Serotonin depletion impairs both Pavlovian and instrumental reversal learning in healthy humans
Molecular Psychiatry (2021)
-
Serotonin transporter binding is increased in Tourette syndrome with Obsessive Compulsive Disorder
Scientific Reports (2019)
-
Motivation and value influences in the relative balance of goal-directed and habitual behaviours in obsessive-compulsive disorder
Translational Psychiatry (2015)
-
Imaging of serotonin transporters with [123I]FP-CIT SPECT in the human hypothalamus
EJNMMI Research (2013)
-
Central serotonin transporter levels are associated with stress hormone response and anxiety
Psychopharmacology (2011)