Abstract
Hypothesis:
Site-specific variables that contribute to the pathogenesis of bronchopulmonary dysplasia (BPD) can be identified.
Objectives:
To evaluate the demographic, nutrition and growth characteristics of infants at risk for developing BPD at two neonatal intensive care units (NICUs: sites A and O).
Study Design:
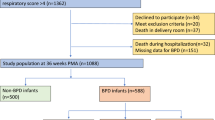
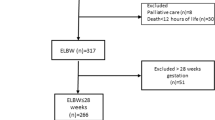
Records of 306 infants of <30 weeks gestational age (GA) who survived to at least 36 weeks postmenstrual age were retrospectively reviewed. Data were obtained for maternal and neonatal demographics, weights, total fluids, calories, carbohydrate, protein and fat intake at birth, 7, 14, 21 and 28 days of life.
Results:
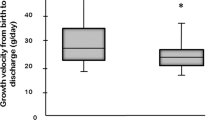
BPD rates were not different at the two sites. No statistical differences were noted in the incidence of maternal chorioamnionitis, pregnancy-induced hypertension or use of antenatal steroids among infants who developed BPD (n=169) and those who did not (n=137). White race, birth weight, respiratory distress syndrome requiring surfactant, sepsis and patent ductus arteriosus were significantly associated (all P⩽0.03) with BPD. After controlling for significant confounding variables, infants who developed BPD had significantly (P<0.001) less weight gain, received less calories and fat in the first postnatal month. In the 26 to 28 weeks GA group, the odds of getting BPD were 5.4 (95%CI: 1.4 to 21.3) times greater for site A than site O (P=0.017).
Conclusion:
Our analysis suggests that while some decrease in BPD can be achieved by focusing on ventilation/oxygen use, this approach is unlikely to impact on the youngest infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Abbreviations
- BW:
-
birth weight
- BPD:
-
bronchopulmonary dysplasia
- GA:
-
gestational age
- IVH:
-
intraventricular hemorrhage
- NEC:
-
necrotizing enterocolitis
- PMA:
-
postmenstrual age
- PDA:
-
patent ductus arteriosus
- PIH:
-
pregnancy-induced hypertension
- PNS:
-
postnatal steroids
- PVL:
-
periventricular leukomalacia
- RDS:
-
respiratory distress syndrome
- TPN:
-
total parenteral nutrition
References
Fanaroff AA, Hack M, Walsh MC . The NICHD neonatal research network: changes in practice and outcomes during the first 15 years. Semin Perinatol 2003; 27: 281–287.
Bhandari A, Bhandari V . Pathogenesis, pathology and pathophysiology of pulmonary sequelae of bronchopulmonary dysplasia in premature infants. Front Biosci 2003; 8: e370–380.
Egreteau L, Pauchard JY, Semama DS, Matis J, Liska A, Romeo B et al. Chronic oxygen dependency in infants born at less than 32 weeks' gestation: incidence and risk factors. Pediatrics 2001; 108: E26.
Jobe AH, Bancalari E . Bronchopulmonary dysplasia. Am J Respir Crit Care Med 2001; 163: 1723–1729.
Walsh MC, Yao Q, Gettner P, Hale E, Collins M, Hensman A et al. Impact of a physiologic definition on bronchopulmonary dysplasia rates. Pediatrics 2004; 114: 1305–1311.
Shennan AT, Dunn MS, Ohlsson A, Lennox K, Hoskins EM . Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics 1988; 82: 527–532.
Ballard JL, Novak KK, Driver M . A simplified score for assessment of fetal maturation of newly born infants. J Pediatr 1979; 95: 769–774.
Papile LA, Burstein J, Burstein R, Koffler H . Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1500?gm. J Pediatr 1978; 92: 529–534.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg 1978; 187: 1–7.
Avery ME, Tooley WH, Keller JB, Hurd SS, Bryan MH, Cotton RB et al. Is chronic lung disease in low birth weight infants preventable? A survey of eight centers. Pediatrics 1987; 79: 26–30.
Todd DA, Jana A, John E . Chronic oxygen dependency in infants born at 24–32 weeks' gestation: the role of antenatal and neonatal factors. J Paediatr Child Health 1997; 33: 402–407.
Van Marter LJ, Dammann O, Allred EN, Leviton A, Pagano M, Moore M et al. Chorioamnionitis, mechanical ventilation, and postnatal sepsis as modulators of chronic lung disease in preterm infants. J Pediatr 2002; 140: 171–176.
Redline RW, Wilson-Costello D, Hack M . Placental and other perinatal risk factors for chronic lung disease in very low birth weight infants. Pediatr Res 2002; 52: 713–719.
Viscardi RM, Muhumuza CK, Rodriguez A, Fairchild KD, Sun CC, Gross GW et al. Inflammatory markers in intrauterine and fetal blood and cerebrospinal fluid compartments are associated with adverse pulmonary and neurologic outcomes in preterm infants. Pediatr Res 2004; 55: 1009–1017.
Van Marter LJ, Allred EN, Pagano M, Sanocka U, Parad R, Moore M et al. Do clinical markers of barotrauma and oxygen toxicity explain interhospital variation in rates of chronic lung disease? The Neonatology Committee for the Developmental Network. Pediatrics 2000; 105: 1194–1201.
Stevens TP, Blennow M, Soll RF . Early surfactant administration with brief ventilation vs selective surfactant and continued mechanical ventilation for preterm infants with or at risk for respiratory distress syndrome. Cochrane Database Syst Rev 2004; 3: CD003063.
Khalaf MN, Brodsky N, Hurley J, Bhandari V . A prospective randomized, controlled trial comparing synchronized nasal intermittent positive pressure ventilation versus nasal continuous positive airway pressure as modes of extubation. Pediatrics 2001; 108: 13–17.
Santin R, Brodsky N, Bhandari V . A prospective observational pilot study of synchronized nasal intermittent positive pressure ventilation (SNIPPV) as a primary mode of ventilation in infants > or =28 weeks with respiratory distress syndrome (RDS). J Perinatol 2004; 24: 487–493.
Palta M, Gabbert D, Weinstein MR, Peters ME . Multivariate assessment of traditional risk factors for chronic lung disease in very low birth weight neonates. The newborn lung project. J Pediatr 1991; 119: 285–292.
Van Marter LJ, Pagano M, Allred EN, Leviton A, Kuban KC . Rate of bronchopulmonary dysplasia as a function of neonatal intensive care practices. J Pediatr 1992; 120: 938–946.
Oh W, Poindexter BB, Perritt R, Lemons JA, Bauer CR, Ehrenkranz RA et al. Association between fluid intake and weight loss during the first ten days of life and risk of bronchopulmonary dysplasia in extremely low birth weight infants. J Pediatr 2005; 147: 786–790.
Bhandari V, Brodsky N, Porat R . Improved outcome of extremely low birth weight infants with Tegaderm application to skin. J Perinatol 2005; 25: 276–281.
Davidson S, Schrayer A, Wielunsky E, Krikler R, Lilos P, Reisner SH . Energy intake, growth, and development in ventilated very-low-birth-weight infants with and without bronchopulmonary dysplasia. Am J Dis Child 1990; 144: 553–559.
Yu VY, Orgill AA, Lim SB, Bajuk B, Astbury J . Growth and development of very low birthweight infants recovering from bronchopulmonary dysplasia. Arch Dis Child 1983; 58: 791–794.
Weinstein MR, Oh W . Oxygen consumption in infants with bronchopulmonary dysplasia. J Pediatr 1981; 99: 958–961.
Brunton JA, Saigal S, Atkinson SA . Growth and body composition in infants with bronchopulmonary dysplasia up to 3 months corrected age: a randomized trial of a high-energy nutrient-enriched formula fed after hospital discharge. J Pediatr 1998; 133: 340–345.
Kurzner SI, Garg M, Bautista DB, Bader D, Merritt RJ, Warburton D et al. Growth failure in infants with bronchopulmonary dysplasia: nutrition and elevated resting metabolic expenditure. Pediatrics 1988; 81: 379–384.
Frank L, Sosenko IR . Undernutrition as a major contributing factor in the pathogenesis of bronchopulmonary dysplasia. Am Rev Respir Dis 1988; 138: 725–729.
Bhandari V, Fall P, Raisz L, Rowe J . Potential biochemical growth markers in premature infants. Am J Perinatol 1999; 16: 339–349.
Bhandari V, Burke G, Price M, Hussain N . Growth failure in infants developing severe BPD occurs by week 3 of postnatal life. Pediatr Res 1997; 41: 140A.
Wilson DC, McClure G, Halliday HL, Reid MM, Dodge JA . Nutrition and bronchopulmonary dysplasia. Arch Dis Child 1991; 66: 37–38.
deRegnier RA, Guilbert TW, Mills MM, Georgieff MK . Growth failure and altered body composition are established by one month of age in infants with bronchopulmonary dysplasia. J Nutr 1996; 126: 168–175.
Frank L . Antioxidants, nutrition, and bronchopulmonary dysplasia. Clin Perinatol 1992; 19: 541–562.
Helbock HJ, Motchnik PA, Ames BN . Toxic hydroperoxides in intravenous lipid emulsions used in preterm infants. Pediatrics 1993; 91: 83–87.
Sosenko IR, Rodriguez-Pierce M, Bancalari E . Effect of early initiation of intravenous lipid administration on the incidence and severity of chronic lung disease in premature infants. J Pediatr 1993; 123: 975–982.
Lucas A . Early use of lipid infusions in very low birth weight infants.J Pediatr 1994; 125: 329–330.
Bloom BT, Mulligan J, Arnold C, Ellis S, Moffitt S, Rivera A et al. Improving growth of very low birth weight infants in the first 28 days. Pediatrics 2003; 112: 8–14.
Bhandari V, Bizzarro MJ, Shetty AH, Zhong XA, Page GP, Zhang H et al. Familial and genetic susceptibility to major neonatal morbidities in preterm twins. Pediatrics 2006; in press.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Akram Khan, M., Kuzma-O'Reilly, B., Brodsky, N. et al. Site-specific characteristics of infants developing bronchopulmonary dysplasia. J Perinatol 26, 428–435 (2006). https://doi.org/10.1038/sj.jp.7211538
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211538
Keywords
This article is cited by
-
Vascular placental pathology and the relationship between hypertensive disorders of pregnancy and neonatal outcomes in very low birth weight infants
Journal of Perinatology (2018)
-
Alveolar formation is dysregulated by restricted nutrition but not excess sedation in preterm lambs managed by noninvasive support
Pediatric Research (2016)
-
The association between hypertensive disorders in pregnancy and bronchopulmonary dysplasia: a systematic review
World Journal of Pediatrics (2013)
-
Maternal preeclampsia and risk of bronchopulmonary dysplasia in preterm infants
Pediatric Research (2012)
-
Nutrition of preterm infants in relation to bronchopulmonary dysplasia
BMC Pulmonary Medicine (2011)