Abstract
OBJECTIVE: A significant increase in the triplet birth rate has occurred recently. This rise is of concern, as these infants are historically reported to be at risk of adverse outcome. Thus, we examined the outcome of triplet births in a large contemporary case series.
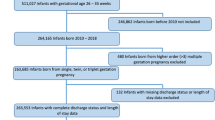
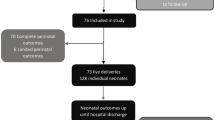
STUDY DESIGN: Since 1993, detailed clinical data have been collected on all patients admitted to our Neonatal Intensive Care Unit. We retrospectively analyzed this database to examine triplet outcome.
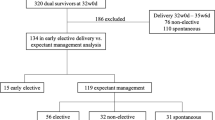
RESULTS: A total of 51 consecutive sets of triplets were born over a 9-year period. The mean birth weight for triplets was 1789±505 g, mean gestational age was 32.6±2.7 weeks, with discordancy present in 17.6% of neonates. Complications of prematurity were infrequent. Triplet survival to discharge was 96%.
CONCLUSIONS:This large contemporary case series of triplets demonstrates excellent survival with low associated morbidity. These data suggest that there may no longer be medical justification for offering selective fetal reduction to parents with triplet pregnancies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Centers for Disease Control and Prevention. Contribution of assisted reproduction technology and ovulation- inducing drugs to triplet and higher-order multiple births—United States, 1980–1997. JAMA 2000;284:299–300.
Martin JA, Park MM . Trends in Twin and Triplet Births: 1980–97. National Vital Statistics Reports 1999;47(24):2.
Macones GA, Shemmer G, Pritts E, et al. Multifetal reduction of triplets to twins improves perinatal outcome. Am J Obstet Gynecol 1993;169:982–986.
Yaron Y, Bryant-Greenwood PK, Dave N, et al. Multifetal pregnancy reduction of triplets to twins: Comparison with non-reduced triplets and twins. Am J Obstet Gynecol 1999;180:1268–1271.
Boulet P, Hedon B, Pelliccia G, et al. Effects of selective reduction in triplet gestation: a comparative study of 80 cases managed with or without this procedure. Fertil Steril 1993;60:497–503.
Martin JA, MacDorman MF, Mathews TJ . Triplet Births: Trends and Outcomes, 1971–94. National Vital Statistics Reports. Series 21, No. 55, 1997; p 7.
Tarter JG, Khoury A, Barton JR, et al. Demographic and obstetric factors influencing pregnancy outcomes in twin gestations. Am J Obstet Gynecol 2002;18:910–912.
Evans MI, Dommergues M, Wapner RJ, et al. Efficacy of trans-abdominal multifetal pregnancy reduction: collaborative experience among the world's largest centers. Obstet Gynecol 1993;82:61–66.
Angel JL, Kalter CS, Morales WJ, et al. Aggressive perinatal care for the high-order multiple gestations: Does good perinatal outcome justify aggressive assisted reproductive techniques. Am J Obstet Gynecol 1999;181:253–259.
Evans MI, Berkowitz RL, Wapner RJ, et al. Improvement in outcomes of multifetal pregnancy reduction with increased experience. Am J Obstet Gynecol 2001;184:97–103.
Anstaklis AJ, Drakakis P, Vlazakis GP, et al. Reduction of multifetal pregnancies to wins does not increase obstetric or perinatal risks. Hum Reprod 1999;14:1338–1340.
Bell MJ, Ternberg JL, Feigin RD, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg 1978;187:1–7.
Papile LA, Burstein J, Burstein R, et al. Incidence and evolution of sub-ependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1500 g. J Pediatr 1978;92:529–534.
Volpe JJ . Hypoxic–ischemic encephalopathy: neuropathology and pathogenesis. In: Neurology of the Newborn. 3rd ed. Philadelphia, PA: WB Saunders; 1987.
Anonymous. An international classification for retinopathy of prematurity. The Committee for the Classification of Retinopathy of Prematurity. Arch Ophthalmol 1994;102:1130.
Smith-Levitin M, Kowalik A, Birnholz J, et al. Selective reduction of multifetal pregnancies to twins improves outcome over non-reduced triplet gestations. Am J Obstet Gynecol 1996;175:878–882.
Kaufman GE, Malone FD, Harvey-Wilkes KB, et al. Neonatal morbidity and mortality associated with triplet pregnancy. Obstet Gynecol 1998;91:342–348.
Suri K, Bhandari V, Lerer T, et al. Morbidity and mortality of preterm twins and higher-order multiple births. J Perinatol 2001;21:293–299.
Leondires MP, Ernst SD, Miller BT, et al. Triplets: outcomes of expectant management versus multifetal reduction for 127 pregnancies. Am J Obstet Gynecol 2000;183:454–459.
Maayan-Metzger A, Naor N, Sirota L . Comparative outcome study between triplet and singleton preterm newborns. Acta Paediatr 2002;91:1208–1211.
Author information
Authors and Affiliations
Additional information
This case series of 51 consecutive sets of triplets demonstrates low morbidity rates and excellent survival rates with contemporary neonatal care.
Rights and permissions
About this article
Cite this article
Barr, S., Poggi, S. & Keszler, M. Triplet Morbidity and Mortality in a Large Case Series. J Perinatol 23, 368–371 (2003). https://doi.org/10.1038/sj.jp.7210950
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7210950
This article is cited by
-
Abnormal maternal echocardiographic findings in triplet pregnancies presenting with dyspnoea
Wiener klinische Wochenschrift (2016)
-
Five cases of dizygotic triplet pregnancy following assisted reproductive techniques
Reproductive Medicine and Biology (2005)