Abstract
Purpose
To assess the effect of hyaluronidase on eye and eyelid movements when used as an adjunct in sub-Tenon's anaesthesia.
Methods
A total of 60 patients who had sub-Tenon's anaesthesia prior to phacoemulsification surgery were divided into two equal groups in a double-masked randomised controlled fashion. Of these, Group A had 4 ml lignocaine 2%, while Group B had 4 ml lignocaine 2% with the addition of sodium hyaluronidase 75 IU/ml. Ocular motility, levator, and orbicularis oculi function were measured in all patients at 5 and 8 min. Levator function was scored from 0 (no function) to 3 (complete function) while orbicularis function was scored from 0 to 2. The score for ocular motility was the sum in four positions of gaze, each position scoring from 0 to 2. Results were compared using a nonparametric test.
Results
Group B achieved significantly better ocular and lid akinesia than Group A both at 5 and 8 min with P<0.01. The median scores for levator function at 5 and 8 min were 2 for Group A and 0 for Group B. For orbicularis function, the median scores at both time intervals were 2 for Group A and 1 for Group B. For ocular motility, the median score for Group A at 5 min was 3 and at 8 min was 2.5; for Group B at 5 min was 0.5 and at 8 min was 0.
Conclusions
The addition of hyaluronidase in sub-Tenon's anaesthesia has a significant effect in improving ocular and lid (levator and orbicularis) akinesia.
Similar content being viewed by others
Introduction
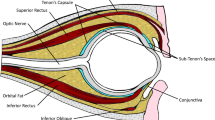
The sub-Tenon's block (STB) has become increasingly popular since its reintroduction as an anaesthetic technique for intraocular surgery.1 It is relatively quick and effective, and allows the use of a blunt cannula thereby avoiding the risk of a needle near the globe.
The role of hyaluronidase as an adjunct in local anaesthesia was first described by Atkinson2 in 1949, where he concluded that its use in retrobulbar anaesthesia produced a more effective akinesia of orbicularis and extraocular muscles.
Hyaluronidase is an enzyme that depolymerises hyaluronic acid, thereby aiding the spread of the local anaesthetic through the extracellular matrix.3 Its use in retrobulbar and peribulbar blocks has been open to question, especially with the improved spreading of newer local anaesthetic agents.4
The effect of hyaluronidase on ocular akinesia in sub-Tenon's anaesthesia has been reported in previous studies. Their results are conflicting, one such study showing it to facilitate the onset of ocular akinesia5 whereas another reports no difference.6 However, there is scant literature on its effect on levator and orbicularis function in sub-Tenon's anaesthesia.
Our study involved a randomised double-masked trial to assess the effect of the addition of hyaluronidase on ocular motility, orbicularis and levator function in sub-Tenon's anaesthesia.
Materials and methods
After receiving informed consent, 60 patients were chosen, all of whom were to undergo phacoemulsification and intraocular lens implantation. Ethical approval was not required as all methods used were well established in routine ophthalmic practice. Patients with eyelid pathology or a known allergy to lignocaine or hyaluronidase were not used. Also, those patients who had retinal detachment surgery with an explant or those with a conjunctival lesion, which would preclude the administration of a sub-Tenon's injection, were excluded.
Subjects were divided into two equal groups in a double-masked randomised controlled fashion. Patients were randomly allocated to either group by corresponding each of them to the letter A or B picked from a brown envelope. Group A received 4 ml lignocaine 2% only, while Group B received 4 ml lignocaine 2% with the addition of sodium hyaluronidase at a concentration of 75 IU/ml.
There was no statistically significant difference between the two groups in terms of age or gender (unpaired t-test). The patient demographics are shown in Table 1.
The blocks were performed by one of the three operators (SAA, MTD, and LY) either with or without the addition of hyaluronidase (see Table 1). Topical benoxinate 0.4% was applied before a wire eye speculum was used to hold the eyelids open. The conjunctiva was grasped in the inferonasal quadrant using Moorfields forceps and the conjunctiva and Tenon's capsule were cut and bluntly dissected using curved spring scissors. A 19-gauge sub-Tenon's cannula was introduced and the anaesthetic agent was slowly injected. A single ophthalmologist (TRGP), who was unaware of patient group allocation, assessed all of the blocks at 5 and 8 min post administration. The following movements were assessed: levator function, orbicularis oculi function, and ocular motility.
Grading for levator and orbicularis function was scored as shown in Table 2. The score for ocular motility was the sum of each movement measured in upgaze, downgaze, left gaze, and right gaze. Therefore, complete ocular akinesia would give a score of 0, whereas normal ocular motility would give a score of 8. The reduction of average score of at least 2, with the addition of hyaluronidase, was considered clinically important.
The observed scores did not follow a normal distribution and thus the nonparametric Mann–Whitney U test was used to assess the findings with a two-sided test at the 5% level of significance.
Results
All patients had normal levator function (score of 3), orbicularis function (score of 2), and ocular motility (score of 8) before injection. Table 3 presents the median lid and ocular motility scores at each time point with Mann–Whitney U test results for Groups A and B. The test results show that there is a significant difference (P<0.01) between Group A and Group B in levator function, orbicularis function, and ocular motility both at 5 and 8 min. Further tests with male and female specific data confirm this significant result except in the case of orbicularis function. Although orbicularis function shows a significant difference between the two groups for males (at 5 min: P=0.002 and at 8 min: P=0.008), there is no significant difference between the two groups for females (at 5 min: P=0.285 and at 8 min: P=0.228).
Percentage distribution of blocks for levator function, orbicularis function, and ocular motility are shown in Figures 1, 2 and 3, respectively. It is clear from these figures that there is a higher percentage of complete or partial blocks in Group B compared to those in Group A. Moreover, these percentages increase over time in both groups for levator function and ocular motility.
Discussion
The use of hyaluronidase as an adjunct in sub-Tenon's anaesthesia has been reported in previous studies with conflicting results in terms of final ocular akinesia. The results of these studies are summarised in Table 4. The purpose of our study was to assess its effect on ocular and lid function.
Two previous studies were performed using differing concentrations of hyaluronidase, one showing it to speed up its onset (with 150 IU/ml hyaluronidase)7 and the other showing it to be of no benefit (when 15 IU/ml).6 Rowley et al8 showed that the addition of only 30 IU/ml hyaluronidase to the STB significantly improved ocular akinesia.
Our study shows that the addition of hyaluronidase at a concentration of 75 IU/ml—this dose having been selected as an approximate average of previous studies—to 4 ml lignocaine 2% facilitates development of ocular akinesia, which may be desirable during cataract surgery so as to provide control of the eye for the surgeon and especially for the trainee. It is also shown to facilitate the development of lid paralysis, which carries several advantages. It provides good control of the lids so as to allow for a more effective draping technique. It also prevents any eye movements from involuntary blinking or voluntary squeezing of the eyelids.
Overall, our study showed there to be a statistically significant difference in orbicularis function with the addition of hyaluronidase (see Table 3). However, the greatest benefit of hyaluronidase in terms of total orbicularis akinesia (complete block 6.7%) was achieved only after 8 min of the injection but not after 5 min (see Figure 2). On the other hand, a stratified analysis of the data according to gender showed no significant difference for females (P>0.05). There is no obvious explanation for this result and a larger trial would underline the significance of this finding. Rowley et al showed that the reduction of eyelid movement was significantly better with the addition of 30 IU/ml hyaluronidase to the STB. However, lid movement was not assessed according to levator and orbicularis action separately, nor were the groups divided according to gender. Another study (see Table 4) showed that the addition of hyaluronidase to the anaesthetic solution resulted in effective akinesia of orbicularis oculi.9
There were no adverse effects during our study. However, recent cases of orbital swelling and acute orbital cellulitis following sub-Tenon's anaesthesia have been reported.10, 11 In future studies, exclusion criteria may be broadened to increase safety, thereby excluding any previous eye surgery or injury and any process which may occlude the sub-Tenon's space, such as scleritis. In conclusion, this study shows that hyaluronidase has a significant effect in improving ocular and lid akinesia when used as an adjunct in sub-Tenon's anaesthesia.
References
Stevens JD . A new local anaesthesia technique for cataract extraction by one quadrant sub-Tenon's infiltration. Br J Ophthalmol 1992; 76: 670–674.
Atkinson WS . Use of hyaluronidase with local anaesthesia in ophthalmology: preliminary report. Arch Ophthalmol 1949; 42: 628–633.
Vickers MD, Schneiden H, Wood-Smith FG . Drugs in Anaesthetic Practice, 6th ed. Butterworths: London, 1984, p 423.
Scott DB, Cousins MJ . Clinical pharmacology of local anaesthetic agents. In: Cousins MJ, Bridenbaugh PO (eds). Neural Blockade in Clinical Anaesthesia and Management of Pain. JB Lippincott: Philadelphia, USA, 1980, pp 103–104.
Alwitry A, Chaudhary S, Gopee K, Butler TK, Holden R . Effect of hyaluronidase on ocular motility in sub-Tenon's anaesthesia: randomized controlled trial. J Cataract Refract Surg 2002; 28: 1420–1423.
Moharib MM, Mitra S, Rizvi SG . Effect of alkalinization and/or hyaluronidase adjuvancy on a local anaesthetic mixture for sub-Tenon's ophthalmic block. Acta Anaesthesiol Scand 2002; 46: 599–602.
Guise P, Laurent S . Sub-Tenon's block: the effect of hyaluronidase on speed of onset and block quality. Anaesth Intensive Care 1999; 27 (2): 179–181.
Rowley SA, Hale JE, Finlay RD . Sub-Tenon's local anaesthesia: the effect of hyaluronidase. Br J Ophthalmol 2000; 84 (4): 435–436.
Rauz S, Subramaniam S . Sub-Tenon's anesthesia and orbicularis oculi function. Ophthalmic Surg Lasers 1997; 28 (9): 727–730.
Dahlmann AH, Appaswamy S, Headon MP . Orbital cellulitis following sub-Tenon's anaesthesia. Eye 2002; 16 (2): 200–201.
Kumar CM, Dowd TC, Dodds C, Boyce R . Orbital swelling following peribulbar and sub-Tenon's anaesthesia. Eye 2004; 18 (4): 418–420.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented at the Meeting of UKISCRS, Countess of Chester Hospital, Chester, UK 10 September 2004.
Rights and permissions
About this article
Cite this article
Aslam, S., Sarker, S., Tran-Dang, M. et al. Effect of hyaluronidase on ocular motility and eyelid function in sub-Tenon's anaesthesia: randomised controlled trial. Eye 20, 579–582 (2006). https://doi.org/10.1038/sj.eye.6701931
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701931
Keywords
This article is cited by
-
Efficacy of sub-Tenon's block using an equal volume of local anaesthetic administered either as a single or as divided doses. A randomised clinical trial
BMC Anesthesiology (2009)
-
Protein therapeutics: a summary and pharmacological classification
Nature Reviews Drug Discovery (2008)