Abstract
The molecular pathology of bladder cancer has been the subject of considerable interest and mutation of the p53 gene, which has been associated with more invasive bladder cancer, has been widely studied. Further, there is evidence that p53 inactivation (either mutation or protein dysregulation), independent of stage, may be predictive of bladder cancer progression. In an effort to avoid possible biases associated with selection of more advanced cases, we examined p53 inactivation in a population-based study of bladder cancer in New Hampshire, using both mutation and immunohistochemical methods. We found the overall prevalence of mutation to be approximately 10%, while immunohistochemical analysis suggests that approximately 66% of the tumours have dysregulated p53 at the protein level. There was a significant association of mutation with persistent p53 staining, but there remained a marked number of tumours discordant for mutation and aberrant p53 immunohistochemistry. Based upon immunohistochemical staining alone, intensity rather than extent of p53 staining was more strongly related to tumour invasiveness. Additionally, all tumours with a mutation in exon 8 stained intensely. Taken together, this suggests that intense staining represents a distinct phenotype of dysfunctional protein. Our data indicate that population-based approaches to somatic alteration of p53 in bladder cancer are crucial to understanding the relationship of p53 changes to aetiology and the outcome of this disease, and further suggest that the pattern of immunohistochemical staining may represent distinct, discernible phenotypes.
Similar content being viewed by others
Main
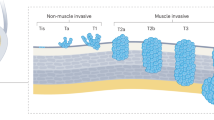
Approximately 60 000 new cases of bladder cancer will be diagnosed in the United States in 2003 (Jemal et al, 2003). This disease occurs predominantly in Caucasians, with other racial/ethnic groups having at least a 50% lower incidence. Regardless of racial or ethnic group, the male-to-female ratio of disease incidence approaches three to one (Jemal et al, 2003). Bladder cancer occurs overwhelmingly in one histologic cell type (transitional cell), although squamous cell carcinoma and adenocarcinoma of the bladder do occur rarely (Silverman et al, 1996). At the time of its initial diagnosis, bladder cancers tend to be of lower stage (Larsson et al, 2003). These noninvasive tumours tend to have a significantly higher survival rate (Larsson et al, 2003; Soloway et al, 2003). Yet, many early-stage bladder cancers will recur and remain superficial and noninvasive for extended periods, while a minority can become invasive and life threatening. The factors that are responsible for altering the noninvasive phenotype of these cancers remain poorly appreciated.
It is clear that inactivation of the p53 pathway is important in bladder cancer, as the number of tumours having p53 mutations increases with the degree of invasiveness of the tumour. At the same time, a large fraction of early-stage disease displays altered p53 staining, suggesting that the p53 pathway is disrupted in some fashion. The significance of this discordance is unclear; stabilisation of nuclear protein could indicate that the protein is mutant, but might also reflect an altered activation pathway for p53 or disrupted turnover kinetics. P53 protein in the cell is tightly regulated, with negligible antibody staining noted in normal tissues. However, inhibition of degradation, mutation or enhanced production of p53 protein (or some combination of these) could all result in antibody recognition of the protein and thus abnormal staining.
Our understanding of the p53 pathway in bladder cancer derives largely from hospital-based and retrospective studies that have captured advanced stage patients undergoing surgery for their disease (Spruck et al, 1994; Silverman et al, 1996; Smith et al, 2003; Soloway et al, 2003). Population-based approaches have been used to avoid possible biases attributable to the study of aggressive and invasive disease (Berggren et al, 2001; Larsson et al, 2003). Overall, the prevalence of mutation has varied quite widely, with the larger and population-based studies tending to report a smaller prevalence of mutation (Sidransky et al, 1991; Fujimoto et al, 1992; Cordon-Cardo et al, 1994; Berggren et al, 2001). Studies indicate that the presence of mutation at p53 markedly increases with stage and grade of disease (Spruck et al, 1994; Berggren et al, 2001; Smith et al, 2003). This has led some to suggest that there could be a very sharp boundary between the different disease categories (Larsson et al, 2003). The few studies that compared both immunohistochemical staining and p53 mutation found appreciable staining in tumours harbouring mutations, as expected (Esrig et al, 1993; Cordon-Cardo et al, 1994; Oyasu et al, 1995; Vet et al, 1995; Abdel-Fattah et al, 1998; Bernardini et al, 1999). These studies also observed a surprising number of discordant samples where p53 immunohistochemistry (IHC) was positive but no mutation was detectable.
Both the early-stage tumours lacking persistent staining and those cancers with p53 staining may later undergo p53 mutation and become aggressive and invasive. Thus, one might expect the immunohistochemical p53 staining pattern to differ between tumours with stabilised wild-type p53 protein and those in which the protein is mutant. To examine the characteristics of positive staining for p53 protein in bladder tumours systematically, we evaluated both p53 mutation and immunohistochemical staining of p53 in a population-based sample of bladder cancers from inhabitants of New Hampshire. We sought to determine the associations of p53 mutation with clinical stage and grade of tumour in the general population setting and elucidate the relationship of staining characteristics, mutation and the clinical and pathologic features of the tumours.
Materials and methods
Study population
Residents of New Hampshire aged 25–74 years, diagnostic from July 1, 1994 to June 30, 1998, were identified by a rapid reporting system of the New Hampshire State Cancer Registry (Karagas et al, 1998). Briefly, by state law, practitioners are required to provide a report of cancer patient after diagnosis. Study participants completed an extensive interview to obtain information on demographic traits and carcinogen exposure (Karagas et al, 1998).
Pathology reports and paraffin-embedded tumour specimens were requested from the treating physician/pathology laboratories. Bladder tumours were reviewed by one pathologist and classified according to the WHO classification of bladder tumours. DNA was extracted by a previously reported method (Nelson et al, 1998). Briefly, three 20-μm sections were cut and transferred into tubes with digestion buffer. After microwave treatment and centrifugation, the paraffin ring was removed. Paraffin-free tissue pellets were suspended in digestion buffer with proteinase K. Supernatants containing DNA lysate were boiled to denature the residual protease.
Immunohistochemistry
Immunohistochemical staining of paraffin-embedded slides was performed using the avidin–biotin complex technique. For each case, a single representative slide was selected for staining and histologic evaluation. Briefly, slides were deparaffinised and hydrated into water. Slides underwent antigen retrieval in Citra solution using the Biocare Decloaking Chamber (Biocare Medical, Walnut Creek, CA, USA). Staining of p53 was performed using a monoclonal antibody (BioGenex, San Ramon, CA, USA) at a 1 : 100 dilution on the Optimax I-6000 Immunostainer (BioGenex). An appropriate positive control was used in each staining run, and each slide was stained with a negative control. The intensity of nuclear staining was graded on a semiquantitative scale (0–3), rating intensity in the dominant pattern within the tumour. In addition, the percentage of positively staining tumour cells was scored (negative, 1–9%, 10–49%, or ⩾50%).
Mutation analysis
SSCP analysis of p53 exons 5–9 was performed on all bladder tumour samples. Exons were amplified by PCR containing fluorescence dye-labelled primers. Previously reported primer sequences for each exon were used (Toguchida et al, 1992). In all, 1 μl of PCR product and 1 μl TAMRA-350 size standard (Applied Biosystems, Foster City, CA, USA) were denatured in 4 μl of formamide/blue-dextran denaturing buffer at 95°C for 5 min, and then loaded onto MDE gels. Gel electrophoresis was carried out on a DNA autosequencer ABI Prism 377 (Applied Biosystems), with an external cooling system (Thermo NESLAB Portsmouth, NH, USA) attached for gels run at 25°C. Genescan 3.1 software (Applied Biosystems) was used for fragment analysis. Samples with variant SSCP bands were purified using Centri-Sep columns (Princeton Separations Adelphia, NJ, USA) and directly sequenced by a DNA autosequencer ABI Prism 377 using the Big Dye Terminator v3.0 sequencing kit (Applied Biosystems) according to the manufacturer's instructions. The data were analysed with the Sequencing Analysis 3.3 software (Applied Biosystems) and Sequencher 4.1 software (Gene Codes Corporation, Ann Arbor, MI, USA).
Statistical analysis
We examined the prevalence of p53 mutation, persistent staining (⩾50%) and strong intensity (3+) by patient demographic characteristics and tumour histology and stage. We also used the disease group classification described by Larsson (Larsson et al, 2003), which distinguished patient survival. We estimated the prevalence odds ratios (POR) and 95% confidence intervals (CI) of patient demographic and tumour traits for each p53 mutation, persistent staining and strong intensity separately, using a log-linear model with adjustment for the other factors. We also calculated the sensitivity, specificity and predictive positive values to evaluate the concordance between p53 mutation and the two immunohistochemistry parameters (i.e., persistent staining and strong intensity). We further performed a logistic regression analysis to contrast those with tumours containing both mutation and positive immunohistochemistry with tumours that had no evidence of either a p53 mutation or positive immunohistochemistry. Lastly, we compared the number of tumours with intensity staining and the number of tumours with invasive disease by the type of p53 mutation using a χ2 test. Due to the sparse numbers of tumours, we grouped the low-grade tumours (G1 and G2) together when necessary.
Results
Pathology materials of 421 of 438 (92%) cases were independently reviewed. Of those re-reviewed, 11 (3%) were deemed non-cancerous by the study pathologist. In addition to these cases, we excluded the tumours from a subject who had multiple tumours of two histologies and tumours from the 15 non-white subjects. Of the remaining tumours, we performed mutational analysis on 330 tumours, and assessed persistent staining and staining intensity in 356 tumours. There were no significant clinical or demographic differences comparing those patients included and excluded for p53 study. The overall prevalence of p53 mutation was 9.1% (30 out of 330; Table 1). There was no statistically significant difference in mutation prevalence by gender or age, although there were more mutations in women than men. The prevalence of p53 mutation increased from 4.6% for the noninvasive low-grade tumours to 19.4% for the noninvasive high-grade tumours (POR=4.4; 95% CI=1.5–12.5) and to 15.4% for invasive tumours (POR=3.4; 95% CI=1.4–8.0). Likewise, the prevalence of mutation clearly increased with more advanced disease group (using the Larsson classification (Larsson et al, 2003)), with a POR of 4.8 (95% CI=1.8–12.8) for T2 tumours compared to TaG1-G2 tumours (Table 1).
The same tumours were evaluated for p53 presence using immunohistochemical staining, using separate criteria for the extent of staining (⩾50% of the cells in the tumour having evidence of persistent p53 protein) and intensity (scored as 0, 1, 2 or 3). When these data were analysed, we also observed no effect of gender or age on inactivation of p53 (Table 1). Strong intensity of staining (3 vs <3) was associated with tumour invasiveness and grade; 63% (60 out of 96) of the invasive tumours had an intensity rating of 3, while only 6% (13 out of 218) of the noninvasive tumours were intensely stained (POR=10.8; 95% CI=5.9–19.9). Again, with the Larsson disease group classification (Larsson et al, 2003), the POR for T2 tumours was increased for intense p53 staining (POR=12.4; 95% CI=6.3–24.2) compared to TaG1–G2 tumours. There was a much less marked association of positive IHC staining with invasive disease when the criteria were based on the proportion of positively staining cells (⩾50%) (Table 1).
Table 2 (a) and (b) provides the relationship between the different measures of p53 alteration. The sensitivity and specificity were both higher for intense IHC staining than persistent staining when compared with p53 mutation (Table 2 (a)). Persistent staining alone was far more prevalent than intense staining, although there was a significant correlation between the two measures (Table 2 (b)).
In an effort to refine our estimates of the clinical factors associated with alterations of the p53 pathway, we compared the tumours containing both a p53 mutation and evidence of inactivation by IHC with those that were wild type for IHC and mutation (Table 3). P53 inactivation clearly increased with tumour grade (Table 3). Also, the classification of bladder cancers by disease group indicated a substantial increase in prevalence of both persistent and intense p53 staining in the presence of mutation associated with more aggressive disease (Table 3).
We further examined whether the pattern of p53 staining was related to a part of the p53 gene (i.e. a specific exon). As is evident in Table 4, all of the mutations in exon 8 were associated with intense staining. Four of the five tumours with exon 8 mutations were invasive. Compared with all other exons, there was a significant association of intense staining with a mutation in exon 8 of the p53 gene (P=0.02).
Discussion
We used a population-based approach to examine somatic inactivation of the p53 gene in bladder cancer. We observed the overall prevalence of p53 mutation to be approximately 10%. This is similar to that reported by Berggren et al (2001) in a large, non-hospital-based study in Sweden. Other studies that selected for hospitalised cases and specifically patients who undergo cystectomy report much higher frequencies of p53 mutation (Sidransky et al, 1991; Fujimoto et al, 1992; Cordon-Cardo et al, 1994). This is likely attributable to the clear association of p53 mutation with disease grade and stage. In our study (as well as almost all others), the prevalence of mutation increases with degree of invasiveness, and hospitalised patients will certainly be more likely to have more invasive disease that requires medical intervention. This suggests that p53 mutations normally occur late in the evolution of bladder tumours and that they are associated with a rapid, invasive phenotype.
The significance of the discordance between IHC-positive tumours and p53 mutation is unclear, although it is commonly reported (Gao et al, 2000; Babjuk et al, 2002; Doak et al, 2003). This discordance may suggest several hypotheses. It is often assumed that stabilisation of nuclear protein indicates that the protein is mutant. However, the presence of wild-type protein may indicate that p53 is functionally inactive because of alterations in the pathways that lead to its activation. Candidates for alteration in this pathway clearly include the MDM2 protein, which is responsible for catalysing the ubiquitination and degradation of p53. MDM2 is often altered in bladder cancer (Lu et al, 2002), and thus should be evaluated in concert with examination of p53 for persistent and intense staining, as well as with mutation. Regardless of the mechanism, in the case where the p53 protein is normal, but persistent staining is detectable, its function is most likely dramatically altered. It is clearly possible (perhaps even likely) that tumour clones with mutations in the p53 gene have features distinct from tumours that have other alterations in the pathway.
Importantly, our data suggest that the histologic character of staining (i.e. intensity of staining vs percent) is more indicative of tumour aggressiveness. Intense staining might occur when p53 is completely inactivated and the protein becomes more densely distributed in the nucleus of the cell. At the same time, an increased number of cells with positive (but less intense) staining may reflect a distinct form of pathway inactivation where activation or the protein is altered. Our data are consistent with this hypothesis in that we found at least some specificity for mutations; all of the mutations in exon 8 were associated with intense staining.
Finally, our data further suggest that additional work is needed to fully understand the underlying reason for the discordance between p53 protein persistence in early-stage bladder cancer. It seems clear that multiple mechanisms of p53 alteration are detected by immunohistochemical staining, and these differences may be associated with the characteristics of the bladder tumour. In addition, detection of aberrant p53 protein (along with proteins in the p53 pathway) using antibody-mediated methods can likely be made more sensitive and specific for detecting clinically important endpoints.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Abdel-Fattah R, Challen C, Griffiths TR, Robinson MC, Neal DE, Lunec J (1998) Alterations of TP53 in microdissected transitional cell carcinoma of the human urinary bladder: high frequency of TP53 accumulation in the absence of detected mutations is associated with poor prognosis. Br J Cancer 77: 2230–2238
Babjuk M, Soukup V, Mares J, Duskova J, Sedlacek Z, Trkova M, Pecen L, Dvoracek J, Hanus T, Kocvara R, Novak J, Povysil C (2002) The expression of PAX5, p53 immunohistochemistry and p53 mutation analysis in superficial bladder carcinoma tissue. Correlation with pathological findings and clinical outcome. Int Urol Nephrol 34: 495–501
Berggren P, Steineck G, Adolfsson J, Hansson J, Jansson O, Larsson P, Sandstedt B, Wijkstrom H, Hemminki K (2001) p53 mutations in urinary bladder cancer. Br J Cancer 84: 1505–1511
Bernardini S, Adessi GL, Billerey C, Chezy E, Carbillet JP, Bittard H (1999) Immunohistochemical detection of p53 protein overexpression versus gene sequencing in urinary bladder carcinomas. J Urol 162: 1496–1501
Cordon-Cardo C, Dalbagni G, Saez GT, Oliva MR, Zhang ZF, Rosai J, Reuter VE, Pellicer A (1994) p53 mutations in human bladder cancer: genotypic versus phenotypic patterns. Int J Cancer 56: 347–353
Doak SH, Jenkins GJ, Parry EM, Griffiths AP, Shah V, Baxter JN, Parry JM (2003) Characterisation of p53 status at the gene, chromosomal and protein levels in oesophageal adenocarcinoma. Br J Cancer 89: 1729–1735
Esrig D, Spruck III CH, Nichols PW, Chaiwun B, Steven K, Groshen S, Chen SC, Skinner DG, Jones PA, Cote RJ (1993) p53 nuclear protein accumulation correlates with mutations in the p53 gene, tumor grade, and stage in bladder cancer. Am J Pathol 143: 1389–1397
Fujimoto K, Yamada Y, Okajima E, Kakizoe T, Sasaki H, Sugimura T, Terada M (1992) Frequent association of p53 gene mutation in invasive bladder cancer. Cancer Res 52: 1393–1398
Gao JP, Uchida T, Wang C, Jiang SX, Matsumoto K, Satoh T, Minei S, Soh S, Kameya T, Baba S (2000) Relationship between p53 gene mutation and protein expression: clinical significance in transitional cell carcinoma of the bladder. Int J Oncol 16: 469–475
Jemal A, Murray T, Samuels A, Ghafoor A, Ward E, Thun MJ (2003) Cancer statistics, 2003. CA Cancer J Clin 53: 5–26
Karagas MR, Tosteson TD, Blum J, Morris JS, Baron JA, Klaue B (1998) Design of an epidemiologic study of drinking water arsenic exposure and skin and bladder cancer risk in a US population. Environ Health Perspect 106(Suppl 4): 1047–1050
Larsson P, Wijkstrom H, Thorstenson A, Adolfsson J, Norming U, Wiklund P, Onelov E, Steineck G (2003) A population-based study of 538 patients with newly detected urinary bladder neoplasms followed during 5 years. Scand J Urol Nephrol 37: 195–201
Lu ML, Wikman F, Orntoft TF, Charytonowicz E, Rabbani F, Zhang Z, Dalbagni G, Pohar KS, Yu G, Cordon-Cardo C (2002) Impact of alterations affecting the p53 pathway in bladder cancer on clinical outcome, assessed by conventional and array-based methods. Clin Cancer Res 8: 171–179
Nelson HH, Wiencke JK, Gunn L, Wain JC, Christiani DC, Kelsey KT (1998) Chromosome 3p14 alterations in lung cancer: evidence that FHIT exon deletion is a target of tobacco carcinogens and asbestos. Cancer Res 58: 1804–1807
Oyasu R, Nan L, Szumel RC, Kawamata H, Hirohashi S (1995) p53 gene mutations in human urothelial carcinomas: analysis by immunohistochemistry and single-strand conformation polymorphism. Mod Pathol 8: 170–176
Sidransky D, Von Eschenbach A, Tsai YC, Jones P, Summerhayes I, Marshall F, Paul M, Green P, Hamilton SR, Frost P, Vogelstein B (1991) Identification of p53 gene mutations in bladder cancers and urine samples. Science 252: 706–709
Silverman D, Morrison A, Devesa S (1996) Bladder Cancer. In Cancer Epidemiology and Prevention, Schottenfeld D, Fraumeni JJ (eds), pp 1156–1179. New York, NY: Oxford University Press
Smith ND, Rubenstein JN, Eggener SE, Kozlowski JM (2003) The p53 tumor suppressor gene and nuclear protein: basic science review and relevance in the management of bladder cancer. J Urol 169: 1219–1228
Soloway MS, Bruck DS, Kim SS (2003) Expectant management of small, recurrent, noninvasive papillary bladder tumors. J Urol 170: 438–441
Spruck III CH, Ohneseit PF, Gonzalez-Zulueta M, Esrig D, Miyao N, Tsai YC, Lerner SP, Schmutte C, Yang AS, Cote R, Dubeau L, Nicholas PW, Hermann GG, Steven K, Horn T, Skinner DG, Jones PA (1994) Two molecular pathways to transitional cell carcinoma of the bladder. Cancer Res 54: 784–788
Toguchida J, Yamaguchi T, Dayton SH, Beauchamp RL, Herrera GE, Ishizaki K, Yamamuro T, Meyers PA, Little JB, Sasaki MS, Weichselbaum RR, Yandell DW (1992) Prevalence and spectrum of germline mutations of the p53 gene among patients with sarcoma. N Engl J Med 326: 1301–1308
Vet JA, Bringuier PP, Schaafsma HE, Witjes JA, Debruyne FM, Schalken JA (1995) Comparison of P53 protein overexpression with P53 mutation in bladder cancer: clinical and biologic aspects. Lab Invest 73: 837–843
Author information
Authors and Affiliations
Corresponding author
Additional information
This publication was made possible by grant number 5 P42 ES05947 and ES07373 from the NIEHS. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIEHS. Also supported by ES00002
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Kelsey, K., Hirao, T., Schned, A. et al. A population-based study of immunohistochemical detection of p53 alteration in bladder cancer. Br J Cancer 90, 1572–1576 (2004). https://doi.org/10.1038/sj.bjc.6601748
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6601748
Keywords
This article is cited by
-
Immune profiles and DNA methylation alterations related with non-muscle-invasive bladder cancer outcomes
Clinical Epigenetics (2022)
-
p53 null phenotype is a “positive result” in urothelial carcinoma in situ
Modern Pathology (2022)
-
Facteurs pronostiques biologiques des cancers de la vessie. Interactions avec la radiothérapie
Bio tribune magazine (2010)
-
Arsenic exposure predicts bladder cancer survival in a US population
World Journal of Urology (2010)
-
P53 immunoexpression as a prognostic marker for human astrocytomas: a meta-analysis and review of the literature
Journal of Neuro-Oncology (2010)