Key Points
-
Assessment of pulpal health is important prior to placing indirect restorations, however, in some situations this is difficult as is the decision whether to root canal treat or not.
-
A tooth that requires root canal treatment should initially be evaluated as to its importance within the dentition, periodontal health and restorative status as well as from an endodontic point of view.
-
Critical assessment of root filled teeth and their long term prognosis is important prior to placing the definitive indirect restoration.
Key Points
Restoration of the endodontically treated tooth
-
1
Restoration of the root-filled tooth: pre-operative assessment
-
2
Tooth preparation for post–retained restorations
-
3
Post and core systems, refinements to tooth preparation and cementation
-
4
Weakened anterior roots – intraradicular rehabilitation
Abstract
This is the first in a series of four papers related to the management of root canal treated teeth. When teeth compromised by extensive restorations become non-vital, suggestions have been given as to how root canal treatment can be carried out with the greatest chance of success. Once root canal treated, either by a previous dentist or by the current dentist, a review of the assessment process that should be carried out prior to placing costly indirect definitive restorations is given. It will be clear that post-retained restorations are mainly reserved for anterior or single-rooted teeth, posterior teeth rarely requiring a post for core retention. The second paper in this series describes the basic tooth preparation that should be carried out prior to placing a post. Depending on the type of post system used, further modifications to tooth preparation may be required and the cementation techniques may also have to be modified. The third paper therefore discusses the various post types, when and how they should be used for optimum results. The final paper addresses reinforcement and restoration of compromised root canals, such as those with immature, open apices, or those that have been over-prepared for previous post-retained restorations.
Similar content being viewed by others
Introduction
Posts have been used to restore non-vital teeth for many years. Early literature dating from over two hundred years ago documents the use of posts made from wood, gold or platinum. Wooden posts were retained in the root canal by absorption of moisture that caused them to swell and metal posts were fixed into place with wooden wedges, as cements had not yet been developed.1
In these early years, the role of microbes in the aetiology of pulpal and periradicular disease was not fully understood and therefore only a limited attempt was made at cleaning, shaping and obturating the root canal. This often caused persistent symptoms following the placement of a post in the root canal. Dentists then discovered that placing grooves in the wooden posts or root canal allowed drainage from the root canal and this alleviated the patient's symptoms. Endodontic treatment is aimed at removing microorganisms from the root canal system and providing a seal to prevent their re-entry. This should provide an environment that allows healing of the periradicular tissues.
Following successful root canal treatment, the tooth can remain as a functional unit within the dental arch providing the coronal tooth structure is adequately restored. The design of the definitive restoration depends very much on the amount of remaining tooth structure, the morphology of the tooth and its position in the dental arch. When there is minimal coronal tooth structure present, posts are required to improve the retention of the core material. The use of posts was originally thought to reinforce weakened, endodontically treated teeth and increase their fracture resistance.2,3 It is now accepted that this is not correct and in fact placing posts can often result in failure from iatrogenic perforation, root fracture or cement failure.4,5 More teeth are lost because of these reasons than from failure of the root canal treatment.6
Traditionally, posts and/or cores have been made from metal, either cast or prefabricated. When placed with care they have a high success rate. Weine et al (1991)7 reported only nine failures in 138 teeth restored with cast, tapered posts and cores after a ten-year period. Recently, non-metal alternatives such as ceramic and quartz fibre posts have been introduced into clinical practice and these will be discussed in the third paper in this series.
Irrespective of which post system or type of restoration is chosen for placement in a root canal treated tooth, it is important to carry out a thorough pre-operative clinical and radiographic assessment. This paper will review aspects of the assessment which will ensure appropriate timing, execution and design of definitive restorations for each individual clinical case.
Biological considerations
For many years dentists assumed that endodontic treatment resulted in a decrease in the moisture content of dentine causing teeth to become more brittle and therefore prone to fracture. This was based on a study which compared the moisture content of vital and non-vital teeth obtained from a dog.8 They found that there was 9% less moisture present in the calcified tissues of the non-vital teeth. In a more recent study the moisture content of vital and endodontically treated teeth was compared using matched pairs of contralateral human teeth extracted for prosthodontic reasons.9 There was no statistically significant difference in moisture content between the two groups suggesting that teeth do not become more brittle as a direct consequence of root canal treatment. However, it is likely that these would have been teeth from older patients with a history of repeated restorations and/or periodontal disease. As such there will generally be a lower moisture content because of tubular sclerosis, secondary and reactionary dentine formation. Whilst the evidence is limited, it does suggest that endodontic treatment is likely to have minimal effect on moisture content of the dentine.
The use of certain sealer cements may also affect the physical properties of root canal treated teeth. It has been shown that in sealers containing zinc oxide–eugenol, free zinc competes with calcium for binding sites on the surface of hydroxyapatite crystals.10 Whilst it is not known if an increase in zinc causes changes in the physical properties of dentine, it has been shown that the eugenol increases dentine microhardness.11
The collagen present in the organic matrix of dentine from root-filled teeth also differs from that of vital teeth in that there are a greater number of immature and fewer mature cross-links present in the former. It is possible that this difference in collagen structure may contribute to a decrease in tensile strength and an increase in brittleness.12 Whilst it is generally accepted that root canal treated teeth are more prone to fracture, the potential changes in biomechanical properties of dentine as a result of the root canal treatment are generally thought to have a relatively minor impact compared to other factors to be considered later in this paper that are more likely to weaken the tooth structure and to contribute to failure.
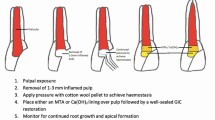
Vital teeth
Whilst this series of papers addresses the restoration of non-vital, root-treated teeth, it is relevant here to briefly discuss heavily restored teeth with pulps of a questionable prognosis. Teeth that have received repeated, previous restorations may have compromised pulpal health known as stressed pulp syndrome. These teeth should be carefully assessed and treated by root canal therapy if required, before commencing complex restorative dentistry.13 Vital teeth with a history of symptoms suggestive of irreversible pulpitis or those that have had direct pulp capping because of a carious exposure should also be considered for root canal treatment prior to placement of a definitive indirect restoration. In a retrospective study of 123 carious teeth that had been pulp capped, 44.5% had failed after five years and 79.7% had failed after ten years.14
Assessment of pulp vitality
Pulpal status is often difficult to establish as sensitivity testing is not always reliable and can produce false-negative and false-positive results. Thermal sensitivity testing using heat or cold is useful as pain from an injured pulp is often triggered or relieved by sudden temperature changes. The electric pulp tester (EPT) uses an electric current to excite a response from the pulpal tissue of the tooth. This, however, gives no information about the blood supply of the tooth, which determines its vitality. This often degenerates long before the nerve fibres and although a positive result would be received, the pulp is not in a healthy state.
There are many other difficulties with the electric pulp test, which can affect the reliability of the results obtained and lead to an incorrect diagnosis of pulp vitality.
-
In young patients the A-delta fibres, which respond to the EPT, are not fully developed, therefore a negative response may be recorded from a vital tooth.
-
The presence of saliva on the tooth can conduct the current to the adjacent teeth and gingival tissues, giving a positive response that does not originate from the tooth being tested.
-
Large restorations or thick linings may prevent the current from stimulating pulpal nerve tissue.
-
Molar teeth may have a combination of vital and non-vital canals and a positive reading will be recorded even though a canal is necrotic.
-
Teeth involved in splints or as part of a bridge may give a positive response as the electric current is transferred to adjacent vital teeth.
-
Tooth wear can lead to large areas of sclerotic dentine that may give a negative response although the tooth is vital.
-
Following trauma, the pulp may give a negative response because of temporary paraesthesia of the nerve fibres. If the tooth remains vital a positive neuronal response should occur within 30–60 days.
For these reasons the results from sensitivity testing are not always reliable and interpretation should be made with caution.
Pulp vitality and operative procedures
Pulp vitality may be lost as a result of trauma, caries and operative procedures. In a retrospective assessment of the periapical and clinical status of crowned teeth over 25 years, the proportion of teeth that remained vital following the placement of crowns was shown to remain high.15 Estimations of crowned teeth with a vital pulp and no signs of pulpal pathology were 98% after five years, falling to 83% after 25 years. These results would appear to be promising. However, the prevalence of periradicular periodontitis associated with crowned teeth in an adult Scottish population has also been investigated.16 In this study, 57% of crowned teeth were vital preparations and 19% of these had distinct radiographic signs of periradicular disease. Worryingly, 62% had widening of the periodontal membrane space indicating early periradicular pathology. It is known, however, that abutment teeth prepared as bridge retainers are at a higher risk of pulpal necrosis because of the more extensive tooth preparation required in order to achieve parallelism. Bergenholtz and Nyman (1984)17 showed that pulpal necrosis developed after several years in 15% of bridge abutment teeth compared to only 3% of non-abutment teeth restored following treatment for advanced periodontal disease (Fig. 1).
In those cases where crowned teeth require root canal treatment it is often tempting to gain access into the pulp chamber through the restoration. It is suggested that careful consideration be given to this approach especially in posterior teeth. Obtaining access through a full coverage restoration removes the dentine core and weakens the tooth. The cement seal is often disrupted and cutting the access preparation damages the occlusal surface of the restoration. Locating the root canals is often difficult as the metal casts a shadow and reduces visibility. Crowning may also have disguised the original tooth morphology and position in the arch and therefore searching for root canals can often lead to perforation.
It is recommended that whenever possible crowns should be dismantled prior to root canal treatment or re-treatment, and that a suitable resin replica temporary crown be provided. When a post exists there is no alternative to this procedure if a coronal rather than surgical approach to re-treatment is to be employed. A coronal approach will allow thorough cleaning of the root canal system however posts should be removed with care to avoid the risk of root fracture.
Restoration of root-filled teeth – pre-treatment assessment
The benefits of root canal treatment or re-treatment and the placement of an indirect restoration, both of which are time-consuming and expensive procedures, must be weighed against extraction of the tooth. Heroics should be avoided to retain teeth with a hopeless prognosis, however, there are clinical situations where extraction is not a preferred option either. In these situations the patient may wish to compromise by having treatment and retaining a tooth of a questionable long-term prognosis. In this situation a pragmatic approach has to be taken and is acceptable providing the patient is aware of the prognosis and is able to give informed consent. Once a decision has been made to save a root canal treated tooth, a careful evaluation is required prior to placement of definitive restorations such as a crown or bridge.
Following the usual history taking, extra-oral and intra-oral examinations, the tooth in question should be evaluated from the endodontic, periodontal, restorative and aesthetic point of view. For this a radiographic examination is essential.
Endodontic evaluation
Clinical endodontic tests should determine the condition of the supporting structures with regard to the presence of inflammation of the periodontal ligament and surrounding periradicular tissues. A positive test is suggestive of persistent or new pathology that may require further treatment prior to placement of the definitive restoration. It is preferable that a definitive restoration is placed on a tooth only when there is no uncertainty with regard to its periradicular status.
The following endodontic clinical tests should be carried out as part of the pre-operative assessment.
Percussion
Tenderness to percussion indicates the presence of periradicular inflammation. This inflammatory response and the resultant periradicular bone destruction are a result of host-derived inflammatory mediators that are induced by bacterial infection of the root canal. However, it is important to note that a negative test does not rule out the presence of inflammation and that a positive result may also be because of periodontal disease. The degree of the response to percussion tends to correlate to the extent of inflammation present.
Prior to testing the tooth in question a control tooth should be tested first to establish a basis for comparison. The incisal or occlusal surface is gently tapped with the end of a mirror handle. Care should be taken if tenderness on biting is a presenting symptom as gentle digital pressure alone may be sufficient to provoke a response. Interestingly, teeth with a chronic periradicular periodontitis often give a negative response to percussion testing.
Palpation
Palpation of the mucosa overlying the apex of a tooth will be tender if inflammation has reached the mucoperiosteum. It may be also possible to detect fluctuation, hardness or crepitus. Some healthy teeth with prominent roots may have fenestrations through the buccal alveolar bone and these can also be tender to palpation. The index finger should be pressed against the bone and a control site should also be included for comparison.
Presence of a sinus tract
The presence of a sinus indicates remaining infection within the root canal system with a periradicular exudate that has progressed through cancellous bone, the cortical plate and the mucoperiosteum to discharge through the mucosal surface. The tract may epithelialise if it has been present for a long time, however this will heal without further treatment on successful resolution of the periapical inflammation.18 The sinus tract will usually drain on the mucosa adjacent to the necrotic tooth. There are occasions, however, when the opening can be far from the involved tooth or drainage occurs through the periodontal ligament. It is therefore useful to place a fine gutta-percha cone into a sinus tract and take a radiograph to confirm the source of the infection rather than relying on the location of the sinus tract opening (Fig. 2).
Unsure as to whether this was due to a retained root following extraction of tooth 37 or because of problems associated with tooth 36 an ISO size 20 gutta percha point is placed into the sinus. Following radiographic examination with the gutta percha in situ it is clear that the sinus tracks from periradicular pathology is associated with tooth 36.
Mobility
The presence of tooth mobility may suggest the loss of connective tissue attachment and inflammation of the periodontal ligament that can be of pulpal or periodontal origin. An acute periradicular abscess may exert a pressure that will cause considerable tooth mobility. This, however, resolves quickly once drainage has been established. Other causes of tooth mobility include root fracture, trauma, occlusal trauma, orthodontic tooth movement and abnormally short roots, therefore further clinical tests are required to obtain a correct diagnosis.
Mobility is assessed by using the handles of two mirrors to apply pressure to the crown of the tooth from the buccal and lingual aspects and also vertically down the long axis of the tooth. The degree of movement obtained should be compared against that of a control tooth or teeth.
Grading of tooth mobility>
Grading of tooth mobility is as follows.19 Grade 0 No detectable movement or physiological movement up to 0.2 mm. Grade 1 Mobility of the crown 0.2–1 mm in the horizontal direction. Grade 2 Mobility of the crown of the tooth >1 mm in the horizontal direction. Grade 3 Mobility of the crown in both horizontal and vertical planes.
A movement of more than 2–3 mm horizontally or movement in a vertical direction suggests that the tooth would be unsuitable for complex treatment especially if the movement is primarily because of periodontal disease and not periradicular pathology.
It is not only important to look at the degree of tooth movement, but the fulcrum about which the movement takes place also gives valuable information. A fulcrum of movement more coronal to the apical third of the root would suggest that a root fracture was the cause. Following trauma, the adjacent teeth should also be observed as movement of more than one tooth enmasse would suggest a dentoalveolar fracture.
Diagnostic probing
Measuring pocket depths at as many sites as possible around the mouth will give an indication of past or present periodontal disease. Whilst generalised circumferential pocketing around teeth with the presence of plaque and calculus is diagnostic of periodontitis, the presence of a deep, narrow pocket may indicate a lesion of pulpal origin or the presence of a root fracture. The latter is the result of a sinus tract draining pus from the apex of a tooth to the oral cavity through the periodontal ligament.
Furcation involvement may result from an infected necrotic tooth as well as periodontal disease (Fig. 3). Bacterial toxins present in the pulp chamber reach the furcation area through accessory canals present on the floor of the pulp chamber. The incidence of furcation root canals ranges from 28% to 76%.20,21 It is therefore important that following root canal treatment gutta-percha is completely removed from the pulp chamber and the entire pulpal floor is covered with a resin-modified, glass-ionomer cement to seal such canals.
Periodontal evaluation
The prognosis of a tooth depends not only on satisfactory root canal and restorative treatment but also on the existing periodontal condition. Retrospective studies have suggested that patients with periodontal disease have a greater attachment loss if a root canal infection is also present.22,23 Jaoui et al (1995)24 evaluated 195 teeth in 35 patients with periodontitis who had received both endodontic and periodontal treatment and concluded that providing patients receive adequate supportive periodontal treatment, root canal treatment should not contribute to the risk of tooth loss for periodontal reasons. The importance of maintaining periodontal health is therefore critical to the long-term success of teeth that have been root canal treated and restored.
A complex relationship exists between the dental pulp and the periodontium. Pathways of potential communication between the two systems exist through the apical foramen, lateral root canals, furcation root canals, patent dentinal tubules and fracture lines within the root structure. The distribution of lateral canals has been reported as 17% in the apical third, 8.8% in the middle third and 1.6% in the coronal third of the root canal.25 In periodontal disease the development of a periodontal pocket may expose an accessory canal and allow bacteria to gain entry to the pulp.
It is important that combined perio-endo lesions are correctly diagnosed to ensure that the patient receives the correct treatment. A periodontal evaluation should include careful probing, vitality testing and radiographic assessment. Traditionally, perio-endo lesions were classified based upon the primary source of the infection.26 However, it is now thought to be more important to assess the pulpal status of the tooth and the presence or absence of a progressing periodontal lesion as these factors will influence the nature of treatment. Chapple and Lumley (1999)27 have suggested the following, simpler classification.
Endodontic lesion
Where a root filled tooth is concerned, remaining bacterial contamination may sustain an endodontic lesion and root canal re-treatment is required.
Periodontal lesion
A periodontal lesion that appears to be progressing requires periodontal treatment.
If the lesion appears stable (no bleeding on probing and stable attachment levels) periodontal treatment is not indicated.
Combined lesion
If because of residual bacteria within the root canal, periradicular periodontitis persists following root canal treatment, and there is also periodontal pathology, the tooth requires root canal re-treatment and periodontal treatment. The root canal re-treatment should be carried out first and the tooth re-assessed as to whether this was sufficient to heal the combined lesion without the need for periodontal treatment.
Root Perforations
Perforation of the root canal system may be iatrogenic, during or after root canal treatment, or pathological such as caries or resorptive defects. This results in a communication between the root canal space and the periodontium. When a microbial infection and/or an irritating restorative material are also present it is unlikely that healing will take place.28 The prognosis of the tooth depends on prevention or treatment of infection at the perforation site using a biocompatible material.
Iatrogenic perforations
Endodontic perforations
Endodontic perforations may occur because of over-instrumentation at any distance along the length of the root or in the furcation area of posterior teeth. Calcified pulp chambers or inadequate removal of the pulpal roof are also risk factors. Strip perforations frequently occur as a result of excessive enlargement of the coronal third of thin, concave roots causing a larger, oval-shaped defect that is difficult to repair. A zipping-type perforation may occur apically in curved canals.
Post placement perforations
Careful preparation of the root canal space and post size selection should avoid perforation, the details of which will be described in the second paper within the series. If a perforation should occur it is likely to cause significant periodontal damage, therefore early diagnosis and treatment are again important.
Pathological perforations
Inflammatory root resorption
Inflammatory root resorption can either be internal or external. Internal inflammatory root resorption may result in a communication between the root canal system and the periodontium before root canal treatment is attempted and the dentist should be aware of this. Internal resorption in vital teeth is characterised radiographically as an oval-shaped enlargement of the pulp chamber or root canal. The exact cause is not known but it frequently follows trauma, pulpal inflammation and calcium hydroxide pulpotomy. The process is rare, often asymptomatic and can quickly progress to cause a perforation. Early identification is important so that root canal treatment can be carried out to arrest the process.
External inflammatory root resorption can occur following trauma that results in damage to the periodontal ligament cells on the root surface. When this occurs in relation to a non-vital infected root canal system, inflammatory resorption can continue unchecked until the resorptive defect communicates with the root canal. Again, early detection of loss of vitality and inflammatory resorption following trauma is important as root canal treatment may arrest the inflammatory process before perforation occurs. External inflammatory root resorption is characterised radiographically as a loss of root outline on the mesial and distal surface associated with a periradicular radiolucency, or a radiolucency superimposed over the outline of the root canal if on the buccal or lingual surface of the root. To establish whether the external root resorption is on either the buccal or palatal root surface, a parallax technique needs to be employed taking two radiographs at different horizontal angles. A lesion that moves mesially when the radiograph tube is angled from the mesial will indicate a palatal or lingual resorptive defect and vice versa for buccal defects.
Diagnosis of root perforation
Diagnosis of a root perforation may only become evident during root canal treatment. Iatrogenic root perforations can sometimes be identified by the direct observation of persistent bleeding into the root canal, however the use of paper points may be needed to illustrate such bleeding. Radiography can also be used to demonstrate perforations, however, such images being only a two-dimensional representation, may fail to show buccal/palatal/lingual perforations when taken with a diagnostic file in place. A second film taken by shifting the radiographic beam angulation to the mesial or distal aspect may detect a file penetrating the buccal or palatal/lingual surface.
Apex locators are also useful in identifying perforations, and are used in the same way as to determine the location of the apical foramen. The diagnostic file is directed towards the opening made by the perforation. This will give a reading that the 'apex' has been reached at a shorter length than anticipated, therefore giving the vertical position of the perforation. If no local anaesthetic has been given, sudden unexpected pain during treatment may also indicate a perforation. Finally, operating microscopes are becoming increasingly popular and the magnification and bright operating light make it excellent for visualising the position and extent of a perforation. They are also useful when repairing the perforation.
Prognosis of root canal perforations
A favourable prognosis depends upon quick diagnosis and treatment to minimise injury and contamination of the surrounding periodontal ligament. Success depends on the following factors:
-
Location – coronal perforations above the gingival level have an excellent prognosis as the periodontium is not involved. Crestal root perforations are most susceptible to epithelial migration and rapid pocket formation, therefore having the lowest success rate following repair.29
-
Time elapsed until repair of perforation is carried out – a high success rate follows immediate repair of perforation site using an aseptic technique.30,31
-
Size of perforation – a small perforation is usually associated with less tissue destruction and inflammation and therefore a better prognosis.28
-
Amount of periodontal ligament irritation.
-
Biocompatibility of the material used for repair.
-
Ability of this material to provide a bacterial tight seal.
Most perforations can now be treated internally using the operating microscope and mineral trioxide aggregate (MTA).32 This material consists of fine particles which are hydrophilic and set in the presence of moisture. It is biocompatible and promotes tissue repair and regeneration.33 Either under- or over-filling a perforation defect with MTA does not appear to affect its ability to seal the root.34
Surgical repair of the perforation site may be necessary in the following circumstances:
-
large perforations;
-
inaccessibility through the root canal;
-
resorptive defects;
-
failure of healing following non-surgical repair;
-
large over-filling of the defect;
-
post and crown cemented in place;
-
large extensive coronal restorations.
Vertical Root Fracture
Vertical root fractures may occur following root canal treatment. This may be caused by over-zealous lateral compaction during obturation or post placement. The prognosis for these teeth is poor and most are extracted because of repeated decementation of post crown and/or the formation of deep periodontal defects and localised bone loss. As root fractures are often difficult to diagnose a careful examination is required. They are often mistaken for perio-endo lesions or failed endodontic treatment. In a study carried out on 92 teeth with vertical root fractures, confirmed following extraction, only one-third were correctly diagnosed by examining dentists.35 Transillumination and magnification are useful aids, however a correct diagnosis is often only confirmed after surgical exploration or extraction.
Novel treatments for root fractures have recently been reported that involve bonding the root segments together with adhesive resin cement. This has been tried by first extracting the tooth and following bonding, re-implanting it back into the socket.36 An alternative technique involving bonding through the root canal has also been described.37 Whilst these preliminary studies have given optimistic results the reality is that the poor prognosis remains and there are more predictable ways of replacing missing teeth such as bridges and implants.
The importance of the biological width in relation to crown margins
Before placing a definitive restoration it is important to ensure that the gingival tissues are clinically healthy. The probing depths should be less than 3 mm and there should be no bleeding on probing. When aesthetics are not important and there is sufficient coronal tooth structure, supragingival margins are recommended.38 Often teeth that have undergone or require root canal treatment have suffered from extensive caries or previous restorations that extend subgingivally. Placing subgingival crown margins encroaches on the biological width and results in persistent inflammation, loss of attachment, pocket formation and recession.
Biological width
The biological width is a band of gingival attachment measuring 2–3 mm from the alveolar bone to the most coronal aspect of the junctional epithelium, and comprises supracrestal fibre attachment and the epithelial attachment.39 Extension of a restorative margin into the gingival sulcus is a compromise but is often necessary for aesthetic or retentive reasons. When restorative margins encroach on the biological width it may lead to bacterial accumulation, inflammation, increased probing depths and/or gingival recession. If a restorative margin must be placed subgingivally, the marginal fit should be optimal, and the margins should extend only slightly into the gingival sulcus.
Where caries or crown margins extend subgingivally or where there is insufficient coronal tooth structure for an adequate ferrule to be created, a crown-lengthening procedure or orthodontic extrusion of the tooth may be necessary to achieve this and to allow placement of the crown margin in a supragingival position.40When crown-lengthening is performed, the final tooth preparation and restoration should be delayed to allow healing and establishment of a normal sulcular depth.41
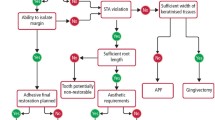
Restorative evaluation
Before carrying out root canal treatment or re-treatment a decision has to be made as to whether the tooth is restorable. Clinical examination of the tooth may reveal extensive caries, previous large restorations, fractures and/or advanced periodontal disease. When deciding if the tooth should be restored, its strategic importance within the dental arch should also be considered. If it is the most distally placed tooth and/or has an opposing tooth, then providing the endodontic and restorative procedures are predictable, it would be advantageous to attempt treatment. However, if a tooth is thought to be unrestorable the remaining dentition should be assessed so that other treatment options such as fixed bridgework, implants or removable prostheses can be discussed with the patient.
When treatment planning for the restoration of root canal treated teeth the following must be considered:
-
the amount of remaining tooth structure;
-
the anatomical position of the tooth;
-
the functional load on the tooth;
-
the aesthetic requirements of the tooth.
The amount of remaining tooth structure
A tooth may have undergone root canal treatment as a result of trauma, in particular a luxation injury and as a result may have a minimal access preparation. At the other extreme, root canal treatment may be the result of previous extensive restorative procedures that have weakened the tooth. A study carried out in vitro has shown that root canal treatment reduces cuspal stiffness by only 5%, whereas cutting a mesio–occlusal–distal (MOD) cavity reduces stiffness by 63% suggesting that root canal treatment per se does not weaken the tooth.42
The decreased strength observed in root canal treated teeth is because of the loss of coronal tooth structure and not directly as a result of the endodontic treatment. There is a direct relationship between the amount of remaining tooth structure and the ability of a tooth to resist occlusal forces.43 As the remaining tooth tissue decreases the possibility of fracture increases. Root canal treated teeth are often heavily restored and are further weakened by access preparation which destroys the pulpal roof and allows for greater flexing of the tooth under function. Gates-Glidden burs previously recommended for preparation of the coronal 4 mm of the root canal may also cause unnecessary loss of tooth structure.44 It is therefore important that these compromised teeth are restored with cuspal coverage restorations as soon as possible following completion of root canal treatment.
The anatomical position of the tooth
Anterior teeth
Anterior teeth do not need posts and full coverage crowns unless the teeth are heavily restored or there is a lack of coronal tooth structure to retain the core.45 As anterior teeth are inclined at an angle to the occlusal plane, the forces of occlusion are not directed along their long axis, making them more susceptible to fracture. Those teeth that are intact, apart from a minimal access cavity preparation, are at minimal risk of fracture and can be restored conservatively with composite resin,45 which has been shown to strengthen the tooth more than by placing a post.46
Posterior teeth
Posterior teeth carry greater occlusal loads and therefore require greater protection against possible fracture. Minimal occlusal access preparations in otherwise intact teeth may be restored conservatively using composite resin which has been shown to improve tooth stiffness.42 Teeth with existing restorations involving the marginal ridge or those with extensive loss of tooth structure require cuspal coverage restorations, either onlays or full coverage crowns.47
Wherever possible posts should be avoided in posterior teeth as the roots are often narrow and/or curved and post space preparation can lead to a strip or lateral perforation. Removal of radicular dentine to accommodate the post further weakens the tooth and may lead to fracture. Posts are not normally required for retention of the core in posterior teeth as there is normally sufficient coronal tooth structure present and mechanical undercut from the pulp chamber.
Intradental pins have been used for many decades to aid the retention of amalgam and composite cores, but threaded pins have a number of disadvantages, the first is they induce stresses and cause crazing in the dentine.48,49,50 In addition to this the fracture resistance of core materials is reduced by the presence of pins51 and catastrophic failure can occur. Other disadvantages include difficulty in contouring core material, microleakage around the pin and placement of pin into the pulp chamber or periodontal ligament.
Nayyar, Walton and Leonard (1980)52 reported a technique of amalgam core build-up where retention is gained from the pulp chamber and coronal part of the root canals (Fig. 4). Perforations and cracking are unlikely to occur as posts and pins are not required. Bonding of the core to tooth structure by using materials such as Panavia or those containing 4-META can also be used, aiding retention and decreasing the risk of coronal leakage.53,54,55 When using composite as a core material in the Nayyar technique, the pulpal floor should be sealed with a resin-modified glass-ionomer. Composite should not be placed in the coronal root canals, as this may be difficult to remove should root canal re-treatment be required. There is also evidence to suggest that placing the restorative material in the coronal part of the root canal is unnecessary as no difference in fracture resistance was found whether or not the root canals had been filled with core material.56
Functional load of the tooth
Tooth wear
Root-filled teeth that show signs of tooth wear, primarily as a result of attrition, possible bruxism and/or heavy occlusal loads especially in a lateral direction require a stronger foundation. Such teeth will have wear facets present or oppose teeth with wear facets and these teeth should be identified and, if heavily restored, restored with a post (if an anterior tooth), or a well retained core (if a posterior tooth) and a full coverage crown.57
Abutment teeth
Abutment teeth prepared for fixed or removable restorations undergo greater horizontal and torquing forces and therefore require more extensive protection and retentive features. Root canal treated teeth may not be suitable abutments in patients with a history of bruxism or those requiring a long span bridge as failure due to lack of retention or root fracture may be more likely.
Aesthetic evaluation
Pulpal necrosis and bleeding from ruptured blood vessels may stain dentine and cause tooth discoloration. When carrying out root canal treatment on anterior teeth, care should be taken to remove all pulpal remnants from the pulp horn areas and ensure that copious irrigation with sodium hypochlorite accompanies the instrumentation stage. Teeth with darkened roots and thin gingivae may cause an aesthetic problem in patients with a high smile line as the entire associated alveolus may appear dark. Metal or black carbon fibre posts in the root canal can also contribute to this discolouration and poor aesthetics, and should therefore be avoided. All-ceramic crowns are being used with increasing frequency and ideally a tooth-coloured post system should be used in conjunction with a composite core. This enables maximum translucency to be achieved and when used with adhesive resin cement a strong integrated restoration should result.
When an anterior tooth does not require crowning, aesthetics can be enhanced by removing excess gutta-percha from the pulp chamber to the level of the amelodentinal junction. The gutta-percha should be sealed with resin-modified glass-ionomer cement to prevent coronal leakage into the root canal and the access cavity restored using a light shade of composite resin to improve the translucency of the tooth. If the discolouration is severe, consideration could be given to non-vital bleaching.
Radiographic examination
On completion of the clinical examination a radiographic assessment is required. Radiographs are essential as they assist in confirmation of the diagnosis and help evaluate the success or failure of a proposed treatment. Radiographic technique should produce films of a consistently high standard to allow accurate interpretation. For endodontic purposes the paralleling technique produces the most accurate periradicular radiograph.58 When used correctly with the aid of film holders this technique should produce films that will have minimal distortion and superimposition. Radiographic interpretation requires a careful and thorough systematic examination using good illumination and magnification. Intra-oral radiographs can be viewed using a SDI radiograph viewer (JS Dental Manufacturing Ltd, PO Box 904, Ridgefield, CT06877) which blocks out any extraneous light that can impede radiographic interpretation and has a x2 magnifying lens incorporated (Fig. 5). Viewing radiographs under these conditions has been shown to significantly improve the diagnosis of apical pathology.59
Radiographic assessment may identify evidence of radicular and periradicular pathology such as infection, resorption, root fracture or perforations. The quality of existing root canal fillings can also be determined. These maybe under-filled, over-filled or poorly compacted with voids present. Inappropriate materials such as pastes or silver cones and the presence of posts or pins may be identified because of the different radiopacities of the materials.
The apical level of an existing root canal filling has an influence on the success of the treatment. In a clinical study, evaluation of 356 patients examined eight to ten years following root canal treatment showed that teeth with necrotic pulps and periradicular radiolucencies had a 94% success rate when the root canal filling was within 2 mm of the radiographic apex. The effect of over-filling or under-filling reduced the success rate to 76% and 68% respectively. If a tooth had an existing, inadequate root canal filling with a periradicular radiolucency, the prognosis was even poorer (62%) following re-treatment.60 Since endodontic treatment of a high standard is necessary to ensure a good long-term prognosis it is often necessary to re-treat teeth prior to provision of the final indirect restoration.61
Conclusions
This paper, which is the first in a series of four, has described the importance of a thorough pre-operative assessment of an individual tooth prior to the provision of the definitive indirect restoration for a heavily restored vital tooth and one that has been root canal filled.
A careful clinical and radiographic evaluation is always required in the first instance to determine if a tooth is restorable or if endodontic procedures are first required and will allow planning for the optimum design of restoration in each case.
References
Ingle JI, Teel S, Wands DH . Restoration of endodontically treated teeth and preparation for overdentures. In Ingle J I, Bakeland L (ed) Endodntics. 4th ed. pp 876–920. Malvern, PA: Williams and Watkins, 1994.
Sokol DJ . Effective use of current core and post concepts. J Prosthet Dent 1984; 52: 231–234.
Hunter AJ, Feiglen B, Williams JF . Effects of post placement on endodontically treated teeth. J Prosthet Dent 1989; 62: 166–172.
Guzy GE, Nicholls JI . In vitro comparison of intact endodontically treated teeth with and without endo-post reinforcement. J Prosthet Dent 1979; 42: 39–44.
Sorenson JA, Martinoff JT . Clinical significant factors in dowel design. J Prosthet Dent 1984; 52: 28–35.
Vire DE . Failure of endodontically treated teeth: Classification and evaluation. J Endod 1991; 17: 338–342.
Weine FS, Wax AH, Wenckus CS . Retrospective study of tapered, smooth post systems in place for 10 years or more. J Endod 1991; 17: 293–297.
Helfer AR, Melnick S, Schilder H . Determination of the moisture content of vital and pulpless teeth. Oral Surg, Oral Med, Oral Pathol 1972; 34: 661–670.
Papa J, Cain C, Messer HH . Moisture content of vital versus endodontically treated teeth. Endod Dent Traumatol 1994; 10: 91–93.
Jonck LM, Eriksson C, Comins NR . An EDX analysis of the root dentine in teeth treated endodontically with zinc oxide and eugenol. J Endod 1979; 5: 20–24.
Biven GM, Bapna MS, Heuer MA . Effect of eugenol and eugenol-containing root canal sealers on the microhardness of human dentin. J Dent Res 1972; 51: 1602–1609.
Rivera E, Yamauchi G, Chandler G, Bergenholtz G . Dentin collagen cross-links of root-filled and normal teeth. J Endod 1988; 14: 195 (Abstract).
Abou-Rass M . The stressed pulp condition: an endodontic-restorative diagnostic concept. J Prosthet Dent 1982; 48: 264–267.
Barthel CR, Rosenkranz B, Leuenberg A, Roulette JF . Pulp capping of carious exposures: treatment outcomes after 5 and 10 years: a retrospective study. J Endod 2000; 26: 525–528.
Valderhaug J, Jokstad A, Ambjornsen E, Norheim PW . Assessment of the periapical and clinical status of crowned teeth over 25 years. J Dent 1997; 25: 97–105.
Saunders WP, Saunders EM . Prevalence of periradicular periodontitis associated with crowned teeth in an adult Scottish subpopulation. Br Dent J 1998; 185: 137–140.
Bergenholtz G, Nyman S . Endodontic complications following periodontal and prosthetic treatment of patients with advanced periodontal disease. J Periodontol 1984; 55: 63–68.
Baumgarter JC, Pickett AB, Muller JT . Microscopic examination of oral sinus tracts and their associated periapical lesions. J Endod 1984; 10: 146–152.
Linde J, Nyman S, Lang NP . Treatment planning. In Linde J (ed) Clinical periodontology and implant dentistry. 4th ed. pp 414–431. Oxford: Blackwell Munksguard, 2003.
Burch JG, Hulen S . A study of the presence of accessory foramina and the topography of molar furcations. Oral Surg, Oral Med, Oral Pathol 1974; 38: 451–455.
Gutmann JL . Prevalence, location and patency of accessory canals in the furcation region of permanent molars. J Periodontol 1978; 49: 21–26.
Ehneuid H, Jansson LE, Lindskog SF, Blomlof LB . Periodontal healing in relation to radiographic attachment and endodontic infection. J Periodontol 1993; 64: 1199–1204.
Jansson lE, Ehnevid H, Lindskog SF, Blomlof LB . Radiographic attachment inperiodontitis-prone teeth with endodontic infection. J Periodontol 1993; 64: 947–953.
Jaoui L, Machtou P, ouhayoun JP . Long-term evaluation of endodontic and periodontal treatment. Int Endod J 1995; 28: 249–254.
De Deus QD . Frequency, location, and detection of lateral, secondary, accessory canals. J Endod 1975; 1: 361–366.
Simon JHS, Glick DH, Frank AL . The relationship of endodontic-periodontic lesions. J Periodontol 1972; 43: 202–208.
Chapple ILC, Lumley PJ . The periodontal-endodontic interface. Dent Update 1999; 26: 331–341.
Fuss Z, Trope M . Root perforations: classification and treatment choices based on prognostic factors. Endo Dent Traumatol 1996; 12: 255–264.
Petersson K, Hasselgen G, Tronstad L . Endodontic treatment of experimental root perforations in dog teeth. Endod Dent Traumatol 1985; 1: 22–28.
Seltzer S, Sinai I, Avgust D . Periodontal effects of root perforations before and during endodontic procedures. J Dent Res 1970; 49: 332–339.
Beavers RA, Bergenholtz G, Cox CF . Periodontal wound healing following intentional root perforations in permanent teeth of Macaca mulatto. Int Endod J 1986; 19: 36–44.
Holland R, Filho JAO, de Souza V, Nery MJ, Bernabé PFE, Dezan Jr E . Mineral trioxide aggregate repair of lateral root perforations J Endod 2001; 27: 281–284.
Torabinejad M, Chivian N . Clinical applications of mineral trioxide aggregate. J Endod 1999; 25: 197–205.
Lee SJ, Monsef M, Torabinejad M . Sealing ability of mineral trioxide aggregate for repair of lateral perforations. J Endod 1993; 19: 541–544.
Tamse A, Fuss Z, Lustig J, Kaplavi J . An evaluation of endodontically treated, vertically fractured teeth. J Endod 1999; 25: 506–508.
Kawai K, Masaka N . Vertical root fracture treated by bonding fragments and rotational replantation. Dent Traumatol 2002; 18: 42–45.
Sugaya T, Kawanami M, Noguchi H, Kato H, Masaka N . Periodontal healing after bonding treatment of vertical root fracture. Dent Traumatol 2001; 17: 174–179.
Schatzle M, Land NP, Anerud A, Boysen H, Burgin W, Loe H . The influence of margins of restorations of the periodontal tissues over 26 years. J Clin Periodontol 2001; 28: 57–64.
Goldberg PV, Higgenbottom FL, Wilson TG Jr . Periodontal considerations in restorative and implant therapy. Periodontology 2000 2001; 25: 100–109.
Davis JW, Fry HR, Krill DB, Rostock M . Periodontal surgery as an adjunct to endodontics, orthodontics, and restorative dentistry. J Am Dent Assoc 1987; 115: 271–275.
Brägger U, Lauchenauer D, Lang N . Surgical lengthening of the clinical crown. J Clin Periodontol 1992; 19: 58–63.
Reeh ES, Douglas WH, Messer HH . Reduction in tooth stiffness as a result of endodontic and restorative procedures. J Endod 1989; 15: 512–516.
Larson TD, Douglas WH, Geistfield RE . Effect of prepared cavities on the strength of teeth. Oper Dent 1981; 6: 2–5.
Hansen EK, Asmussen E . Cusp fracture of endodontically treated teeth restored with amalgam. Teeth restored in Denmark before 1976 versus after 1979. Acta Odontol Scand 1993; 51: 73–77.
McDonald AV, King PA, Setchell DJ . In vitro study to compare impact fracture resistance of intact root-treated teeth. Int Endod J 1990; 23: 304–312.
Trope M, Maltz DO, Tronstad L . Resistance to fracture of restored endodontically treated teeth. Endod Dent Traumatol 1985; 1: 108–111.
Panitvisai P, Messer HH . Cuspal deflection in molars in relation to endodontic and restorative procedures. J Endod 1995; 21: 57–61.
Chan KC, Denehy GE, Ivey DM . Effect of various retention pin insertion techniques on dentinal crazing. J Dent Res 1974; 53: 941.
Khera SC, Chan KC, Rittman BR . Dentinal crazing and interpin distance. J Prosthet Dent 1978; 40: 538–543.
Sivers JE, Johnson WT . Restoration of endodontically treated teeth. Dent Clin North Am 1992; 36: 631–650.
Koa EC, Hart S, Johnston WM . Fracture resistance of four core materials with incorporated pins. Int J Prosthet 1989; 2: 569–578.
Nayyar A, Walton RE, Leonard LA . An amalgam coronal-radicular dowel and core technique for endodontically treated posterior teeth. J Prosthet Dent 1980; 43: 511–515.
Bearn DR, Saunders EM, Saunders WP . The bonded amalgam restoration- a review of the literature and report of its use in the treatment of four cases of cracked-tooth syndrome. Quintess Int 1994; 25: 321–326.
Rueggeberg FA, Caughman WF, Gao F, Kovarik RE . Bond strength of Panavia EX to dental amalgam. Int J Prosthet 1989; 2: 371–375.
Cooley RL, Tseng EY, Barkmeier WL . Dentinal bond strengths and microleakage of a 4-META adhesive to amalgam and composite resin. Quintess Int 1991; 22: 979–983.
Saunders EM, Foley J, Saunders WP . Strength of root filled posterior teeth restored with various materials. J Dent Res 1995; 74: 471 (abstract 563).
Christensen GJ . Posts: necessary or unnecessary? J Am Dent Assoc 1996; 127: 1522–1526.
Glickman GN, Pileggi R . Preparation for treatment. In Cohen S, Burns R C (ed) Pathways of the pulp. 8th ed. pp 103–144. St Louis, Missouri: Mosby, 2002.
Patel N, Rushton VE, Macfarlane TV, Horner K . The influence of viewing conditions on radiological diagnosis of apical inflammation. Br Dent J 2000; 189: 40–42.
Sjögren U, Hagglund B, Sundqvist G, Wing K . Factors affecting the long-term results of endodontic treatment. J Endod 1990; 16: 498–504.
Ray HA, Trope M . Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration. Int Endod J 1995; 28: 12–18.
Author information
Authors and Affiliations
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Tait, C., Ricketts, D. & Higgins, A. Restoration of the root-filled tooth: pre-operative assessment. Br Dent J 198, 395–404 (2005). https://doi.org/10.1038/sj.bdj.4812187
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4812187
This article is cited by
-
A practitioner's guide to gutta-percha removal during endodontic retreatment
British Dental Journal (2017)
-
Root perforations: aetiology, management strategies and outcomes. The hole truth
British Dental Journal (2016)