Abstract
Objectives:
The purpose of the study was to study demographics of tuberculosis of spine and analyze factors that might affect neurological improvement in such patients.
Methods:
Of the 638 suspected cases of spinal tuberculosis, 312 cases with confirmed diagnosis with at least 1-year follow-up were selected for retrospective analysis. Two hundred cases who presented with neurological deficit were further divided into three groups—completely improved, partially improved and no improvement according to American Spinal Injury Association impairment scale (AIS) grading. All continuous variables and categorical variables were compared across groups.
Results:
A total of 209 (66.99%) patients had typical clinical presentation. A total of 264 (84.62%) had typical magnetic resonance imaging (MRI) presentation. Among 356 involved vertebrae, thoracic levels (T1-10) were most commonly affected in 163 (45.78%) followed by thoracolumbar (T11-L2) vertebrae in 98 (27.52%). In 250 patients (80.12%), disease was restricted to one or two adjoining vertebrae. At presentation, 112 (35.89%) patients were neurologically intact, whereas 97 (31%) were AIS D, 65 (20.83%) were AIS C, 8 (2.5%) were AIS B and 30 (9.61%) were AIS A. On statistical analysis, although three groups of patients with complete improvement, partial improvement and no improvement were similar in age, sex, radiological presentation, and co–morbidities and the presence of pulmonary tuberculosis, they were significantly different with regard to the levels of vertebral involvement, AIS grade at presentation, bladder and bowel involvement and its duration.
Conclusions:
In management of patients suffering from tuberculosis of spine, levels of vertebral involvement, AIS grade at presentation, bladder and bowel involvement and its duration significantly affect the final neurological improvement.
Similar content being viewed by others
Introduction
The incidence of bone and joint tuberculosis has increased in the past two decades mainly in relation with AIDS epidemic. In spite of advances in treatment someone in the world dies from tuberculosis every 15 s, and a person is newly infected with M. tuberculosis every second.1, 2 Tuberculosis spine is an important cause of non-traumatic spinal cord injury. In emerging countries, it may be the most common cause of non-traumatic spinal cord injury.3, 4, 5
The typical presentation of tuberculosis spine consists of pain with a localized deformity in the back, tenderness and typical night cries. Malaise, loss of weight, loss of appetite, night sweats and evening rise of temperature are the constitutional systemic symptoms. Patients may or may not have a neurological deficit.6 Magnetic resonance imaging (MRI) is the most commonly used diagnostic tool. Marrow edema, end plate disruption, paravertebral soft tissue, subligamentous collections and high signal of intervertebral disc on T2-weighted images are typical features with good-to-excellent sensitivity for spinal tuberculosis.7, 8 Thoracolumbar spine is reported as the most commonly affected level.9
Most patients of spinal tuberculosis present with mild to no neurological deficit.10, 11 Combination of conservative treatment in the form of anti-tubercular drugs and operative intervention such as simple decompression and stabilization has been reported to result in good clinical outcome in patients presenting with mild-to-moderate deficit.12, 13, 14 Although there are limited studies regarding factors affecting neurological recovery in tuberculosis of spine, delay in starting treatment, cord compression, spinal extension of abscess and involvement of more than two vertebras were considered bad prognostic factors in medically treated patients of spinal tuberculosis according to one study.15 Other studies have stated young age and surgical intervention as a favorable prognostic factor.16, 17 The purpose of the study was to study demographics of tuberculosis of spine and analyze factors that might affect neurological improvement in patients suffering from tuberculosis of spine.
Materials and methods
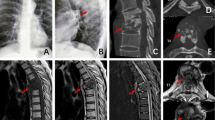
The records of all treated cases of tuberculosis of spine admitted from January 2009 to January 2015 at Indian Spinal Injuries Center at New Delhi, a tertiary care spine and rehabilitation center, were retrospectively analyzed. Of the 638 case records found, more than 1-year follow-up was available for 506 cases. Only 312 cases who were bacteriologically and/or histopathologically confirmed with at least 1-year follow-up were included in the study. Cases diagnosed only on the basis of clinco-radiological findings without bacteriologically and/or histopathologically correlation were excluded from the study. On analysis, 200 cases had neurological deficit on presentation. One of the authors was given only the MRI films, reports and history of all the patients to categorize them into typical and atypical (Figures 1 and 2) while keeping him blinded for the rest of the results. All cases who did not have typical presentation as discussed in introduction were categorized as atypical. MRI records were also used to analyze the level and number of vertebra affected by disease. Data were analyzed on various parameters including documented American Spinal Injury Association impairment scale (AIS),18 at the time of presentation and at final follow-up. All cases who presented with neurological deficit were divided into three groups: completely improved (AIS grade at final follow-up was E), partially improved (AIS grade changed to B, C, D but not E) and no improvement (AIS grading at presentation and final follow-up remained same). Bladder and bowel involvement at initial presentation documented as a loss of perianal sensation and voluntary anal contraction and its further confirmation by urodynamic studies were also analyzed from available records.
All continuous variables were compared across groups by one-way ANOVA. For finding pairwise differences, post hoc analyses were performed using Turkey–Kramer tests. All categorical variables were compared across groups (partial, complete and no recovery) by Chi-square tests. P-value of <0.05 was considered as significant for all tests.
Results
The mean age of patients was 46.63 years with a standard deviation of 18.21. There was no statistical difference between the median ages of patients in years across the groups (completely improved (50.24), partially improved (48.6) and no improvement (52.20)). A total of 165 (52.88%) patients were male. Gender distribution was not different across three groups (P=0.21). The most common co-morbidity was diabetes in 70 (22.43%) patients followed by hypertension in 60 (19.23%). Incidence of diabetes and hypertension was not different across groups (P=0.69 and 0.62). A total of 209 (66.99%) patients presented with typical clinical presentation as discussed in Introduction, whereas 264 (84.62%) had typical MRI picture. Clinical and radiological presentation was not different across the three groups (P=0.37 and 0.52).
Evidence of pulmonary tuberculosis was found in 59 (18.91%) patients. On Chi-square test, incidence of pulmonary tuberculosis was not different across the groups (P=0.40). Delay in treatment was calculated by reviewing the time between the start of symptoms and start of anti-tubercular drugs in the available records. The mean delay in treatment was 79.74 days and median was 30 days. The mean delay between onset of symptoms and surgery was 172.3 days and median was 90 days. On analysis, the delay in treatment and surgery was similar across the groups (P=0.42 and 0.38).
One level of spinal involvement was found in 250 patients (80.44%). Two level involvements were seen in 32 (10.26%), whereas three or more than three levels were seen in only 30 (9.29%). One level was taken as an involvement of one functional unit—two adjacent vertebrae with intervening disc.19 In our study, of the 356 involved vertebrae from C1 to S2, thoracic vertebrae (T1-T10) were most commonly involved (n=163 or 45.78%) followed by thoracolumbar (T11-L2) (n=98 or 27.52%), lumbosacral (L3-S2) (n=70 or 19.66%), sub-axial (C3-C7) (n=21 or 5.80%) and upper cervical (C1-C2) (n=4 or 1.12%) vertebrae (Figure 3). On comparing the groups having one level of vertebral involvement with those having two or more level involvement, complete improvement in AIS grade was significantly higher in the group with only one level of vertebral involvement (P=0.021).
AIS grading was analyzed from the available data (n=312). AIS grading at presentation, at discharge and at final follow-up was analyzed. Although 112 cases (35.89%) presented with intact neurology, 97 (31.0%) were AIS D, 65 (20.83%) were AIS C, 8 (2.50%) were AIS B and 30 (9.61%) were AIS A. At final follow-up, although 128 (64%) were AIS grade E, 39 (19.5%) were grade D, 18 (9.0%) were grade C, 7 (3.50%) were AIS B and 8 (4.00%) were AIS A (Figure 4).
Out of the cases who presented with neurological deficit (n=200), 128 (64%) completely recovered in terms of AIS grading, 46 (23%) had partial recovery, no improvement in AIS grading was seen in 19 (9.5%) and neurological deterioration was documented in 7(3.5%) cases at final follow-up (Figure 5). Although complete recovery was seen only in 4 cases (10.52%) of AIS A and AIS B at presentation, 127 (78.4%) cases presenting with AIS C or AIS D improved completely. This difference was statistically significantly higher as a measure on the Chi-square test with P=0.001.
On analysis of patients (n=200) who presented with neurological deficit, 84 had confirmed bladder and bowel involvement at presentation. For patients with bladder and bowel involvement, mean duration was 39 days and median was 15 days. Only 27 out of 84 patients (32.14%) with bladder and bowel involvement improved completely (AIS E at final follow-up) compared with 97 out of 116 patients (83.62%) without bladder and bowel involvement (Figure 6). On further analysis, of the patients with bladder and bowel involvement for more than 15 days, only 7 patients showed complete recovery. All the cases presenting with AIS A, B or C with bladder and bowel involvement more than 15 days did not improve completely. The duration of involvement of bowel/bladder function in the subgroup that did not improve neurologically was significantly higher (103 days) than the subgroups that either showed partial improvement (19 days) or complete recovery (11 days) (P=0.0001). On Chi-square test to analyze the difference in patients with bladder and bowel involvement compared with those without bowel bladder involvement, the proportion of patients with no bowel bladder involvement was significantly higher in the group with complete recovery (P=0.00).
Of the total (n=312) cases, 190 were surgically treated. Most common procedure (n=160) was all-posterior decompression and pedicle screw fixation two levels above and below the diseased vertebra with decompression through corpectomy of the diseased vertebra and inter-body fusion with cage and bone graft (Figure 7). The most common approach in cervical spine was all-anterior approach. Both anterior and posterior approaches were used only in 18 cases. On analysis, there was no statistically significant difference in neurological improvement regardless of surgical approach and instrumentation (Anterior/Posterior) across the different groups. However, 79% of the initial AIS A/B levels were treated surgically as compared with only 59% of the C/D/E subgroup, with a statistically significant difference between the two groups (Chi-square=5.6, df=1, P=0.017).
Discussion
More than seven decades have passed since the start of modern anti-tubercular drugs, but still there is a lack of clarity regarding presentation, diagnosis and factors affecting the neurological recovery in patients suffering from tuberculosis of spine. In our analysis of 312 bacteriologically/histopathologically confirmed cases of tuberculosis of spine, 209 (66.99%) patients presented with typical clinical presentation, whereas 284 (84.62%) had a typical MRI picture. Although clinical presentation in tuberculosis of spine can be deceptive, MRI remains a good tool in screening of spinal tuberculosis.
The most common co-morbidity was diabetes and hypertension (22.43 and 19.23%, respectively). Others have reported incidence of diabetes as high as 30% in cases of tuberculosis of spine.20 Incidence of pulmonary tuberculosis was 18.91% (59 patients) in our series. Although pulmonary tuberculosis is a known risk factor for tuberculosis of spine, there is no recent literature regarding its incidence in Pott’s spine. One level of vertebral spinal involvement (one functional unit) was documented in a majority of patients (n=250 or 80.44%), whereas two functional units were involved in 32 (10.27%), and three or more than three levels in 30 (9.29%) patients. Although most of the previous studies have documented vertebral level, we have documented functional unit as one level considering paradiscal involvement of disease.19 In a study of 284 cases by Wang,21 13.7% had involvement of one vertebra, two vertebrae were involved in 59.5% and more than three vertebrae involvement was documented in 26.8% of cases.
However, in our study, thoracic levels (T1-10) were most commonly affected (45.78%) followed by thoracolumbar vertebrae (T11-L2) (27.52%). Some of the studies have reported thoracolumbar level as most commonly involved,7 whereas others have found thoracic vertebrae as the most commonly affected.22, 23
In our study, more than one-third of cases (n=112 or 35.89%) presented with intact neurology, whereas 97 (31.0%) were AIS D, 65 (20.83%) AIS C, 8 (2.50%) AIS B and 30 (9.61%) AIS A. There are only few studies documenting the neurological grading in spinal tuberculosis. In a limited study of 60 cases, Gupta23 found that 1 patient (2.08%) was AIS A, 2 (4.16%) were AIS B, 9 (18.75%) were AIS C, 36 (60%) were AIS D and 12 (20%) were AIS E, with complete recovery at final follow-up in 33 patients. In our study, most of the patients (n=162 or 51.83%) presented with AIS C or D. A total of 128 patients (64%) presenting with neurological deficit completely improved following the treatment at final follow-up. Eighty-four patients presented with bladder and bowel involvement and in most involvement was less than 16 days. None of the previous studies have documented the duration of bladder and bowel involvement and its significance in neurological recovery.
A total of 160 (85.21%) patients were treated by all-posterior approach, and posterior instrumentation was used in 148 (93%). Recently published meta-analysis suggested no significant difference between the anterior and posterior approaches in terms of final outcome of the patients as long as anterior decompression is performed. Even all-posterior instrumentation appears to have same clinical outcome as anterior in patients with spinal tuberculosis.24, 25 Significantly higher number of patients with AIS scores A and B were treated surgically (79%) compared with patients who were neurologically intact or AIS C and D at presentation (df=1, P=0.07).
On analyzing the factors that might affect the neurological improvement (partial, complete and no recovery) when different groups were compared, no significant difference was found between the groups in age or sex distribution, delay in initiating treatment, and in the approach to surgery and instrumentation. Although Park16 study supports our finding that gender does not influence the outcome in tuberculosis of spine, but unlike our study he states young age as a favorable prognostic factor. There are no major studies on the effect of delay in treatment on neurological outcome.
The three groups were significantly different in terms of the number of vertebral involvement, AIS grade at presentation and bladder and bowel involvement. In cases with involvement of one functional unit, the chances of complete neurological recovery were significantly higher. Statistically significant number of patients (78.4%) with AIS C and D improved completely compared with those with AIS A and B (P=0.001). Although 83.62% of patients without bladder and bowel involvement improved completely, significantly lesser percentage (32.14%) of patients with bladder and bowel involvement improved completely on final follow-up. None of the patients with AIS A, B or C presentation with bladder and bowel involvement more than 15 days improved completely. In a limited study of 70 medically treated cases of tuberculosis of spine, Garg15 found bladder involvement and involvement of more than 2 vertebrae to be predictors of poor outcome. There is no study on the influence of AIS grading at presentation on the final neurological recovery in cases of spinal tuberculosis. Our study is first of its kind with a large sample size to document demographics of tuberculosis in bacteriologically-confirmed cases. Although AIS grading alone could be an incomplete tool to grade neurological deficit in spinal tuberculosis, AIS grading along with duration of bladder and bowel and levels of vertebral involvements has good prognostic value.
Limitations of study
This was a retrospective study. Also, AIS grading is an incomplete tool to judge neurological deficit in some cases of spinal tuberculosis as it is difficult to grade patients presenting with spasticity.
Conclusions
On the basis of our analysis of 312 bacteriologically-confirmed cases of tuberculosis of spine, we conclude that clinical presentation of tuberculosis can be atypical in up to one-third of cases (33.01% in our series), but majority of them have a typical MRI presentation (84.62%). Thoracic spine is the most commonly affected level (45.78%) followed by thoracolumbar vertebrae (27.52%). In majority of cases (80.44%), disease is restricted to one or two adjoining vertebrae. Almost one-fourth of patients (26.92% in our series) present with bladder and bowel involvement. Most of the cases with neurological deficit presented with AIS C or D (51.83%). Complete neurological improvement was possible in more than half of these cases (64.00% in our series) following conservative or surgical treatment.
Our study seems to suggest that, although age, sex, radiological presentation, co–morbidities, presence of pulmonary tuberculosis, delay in initiating treatment and approach to surgery and instrumentation had no significant effect on final neurological improvement, levels of vertebral involvement, AIS grading at presentation, bladder and bowel involvement and its duration significantly affect the neurological improvement.
References
Dye C, Watt CJ, Bleed DM . Evolution of tuberculosis control and prospects for reducing tuberculosis incidence, prevalence, and deaths globally. JAMA 2005; 293: 2767–2775.
Global Tuberculosis Control. WHO: Geneva, 2012. Available at www.who.int/tb/publications/global_report.
Chhabra HS ISCoS Textbook on Comprehensive Management of Spinal Cord Injuries. ISBN-13: 978-93-5129-440-5 2015.
Bickenbach J; Officer A, Shakespeare T, von Groote P. International Perspectives on Spinal Cord Injury. WHO: Geneva, Switzerland. 2013.
New PW, Reeves RK, Smith É, Eriks-Hoogland I, Gupta A, Scivoletto G et al. International retrospective comparison of inpatient rehabilitation for patients with spinal cord dysfunction: differences according to etiology. Arch Phys Med Rehabil 2016; 97: 380–385.
Tuli SM . Tuberculosis of the Skeletal System, 4th edn. Jaypee Brothers Medical Publishers: New Delhi, India. 2010.
Jain AK, Sreenivasan R, Saini NS, Kumar S, Jain S, Dhammi IK . Magnetic resonance evaluation of tubercular lesion in spine. Int Orthop 2012; 36: 261–269.
Danchaivijitr N, Temram S, Thepmongkhol K, Chiewvit P . Diagnostic accuracy of MR imaging in tuberculous spondylitis. J Med Assoc Thai 2007; 90: 1581–1589.
Alvi AA, Raees A, Khan Rehmani MA, Aslam HM, Saleem S, Ashraf J . Magnetic resonance image findings of spinal tuberclosis at first presentation. J Int Arch Med 2014; 7: 12.
Gupta AK, Kumar C, Kumar P, Verma AK, Nath R . Correlation between neurological recovery and magnetic resonance imaging in Pott's paraplegia CD. Indian J Orthop 2014; 48: 366–373.
Dunn R, Zondagh I, Candy S . Spinal tuberculosis: magnetic resonance imaging and neurological impairment. Spine (Phila Pa 1976) 2011; 36: 469–473.
Patil SS, Mohite S, Varma R, Bhojraj SY, Nene AM . Non-surgical management of cord compression in tuberculosis: a series of surprises. Asian Spine J 2014; 8: 315–321.
Djientcheu VP, Mouafo Tambo FF, Ndougsa IS, Eloundou NJ, Kouna Tsala IN, Ngowe Ngowe M et al. The role of surgery in the management of Pott's disease in Yaoundé. A review of 43 cases. Orthop Traumatol Surg Res 2013; 99: 419–423.
Jain AK . Tuberculosis of the spine: a fresh look at an old disease. J Bone Joint Surg Br 2010; 92: 905–913.
Garg RK, Raut T, Malhotra HS, Parihar A, Goel M, Jain et al. Evaluation of prognostic factors in medically treated patients of spinal tuberculosis. Rheumatol Int 2013; 33: 3009–3015.
Park DW, Sohn JW, Kim EH, Cho DI, Lee JH, Kim KT et al. Outcome and management of spinal tuberculosis according to the severity of disease: a retrospective study of 137 adult patients at Korean teaching hospitals. Spine (Phila Pa 1976) 2007; 32: E130–E135.
Su SH, Tsai WC, Lin CY, Lin WR, Chen TC, Lu PL et al. Clinical features and outcomes of spinal tuberculosis in southern Taiwan. J Microbiol Immunol Infect 2010; 43: 291–300.
Frederick M Maynard Jra, Michael B Bracken, Graham Creasey, John F Ditunno Jr, William H Donovan, Thomas B Ducker, International Standards for Neurological and Functional Classification of Spinal Cord Injury; May 1997, Volume 35, Number 5; American Spinal Injury Association: Atlanta, GA, USA. 266–274.
White AA, Panjabi MM. Clinical Biomechanics of the Spine. Lippincott: Philadelphia, PA, USA, 1990, ISBN 0397507208.
Alavi SM, Sharifi M . Tuberculous spondylitis: risk factors and clinical/paraclinical aspects in the south west of Iran. J Infect Public Health 2010; 3: 196–200.
Wang H, Li C, Wang J, Zhang Z, Zhou Y . Characteristics of patients with spinal tuberculosis: seven-year experience of a teaching hospital in Southwest China. Int Orthop. 2012; 36: 1429–1434.
DOBSON J . Tuberculosis of the spine; an analysis of the results of conservative treatment and of the factors influencing the prognosis. J Bone Joint Surg Br 1951; 33-B: 517–531.
Gupta AK, Kumar C, Kumar P, Verma AK, Nath R, Kulkarni CD . Correlation between neurological recovery and magnetic resonance imaging in Pott's paraplegia. Indian J Orthop 2014; 48: 366–373.
Muheremu A, Niu X, Wu Z, Tian W . Study on anterior and posterior approaches for spinal tuberculosis: a meta-analysis. Eur J Orthop Surg Traumatol 2014; 25 (Suppl 1): S69–S76.
Yang P, He X, Li H, Zang Q, Yang B . Clinical efficacy of posterior versus anterior instrumentation for the treatment of spinal tuberculosis in adults: a meta-analysis. J Orthop Surg Res 2014; 9: 10.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This is an original research, has not been previously published and has not been submitted for publication elsewhere while under consideration. The study was conducted at Indian spine injuries center, New Delhi.
Rights and permissions
About this article
Cite this article
Sharma, A., Chhabra, H., Chabra, T. et al. Demographics of tuberculosis of spine and factors affecting neurological improvement in patients suffering from tuberculosis of spine: a retrospective analysis of 312 cases. Spinal Cord 55, 59–63 (2017). https://doi.org/10.1038/sc.2016.85
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2016.85
This article is cited by
-
Comparative efficacy of traditional conservative treatment and CT-guided local chemotherapy for mild spinal tuberculosis
BMC Musculoskeletal Disorders (2022)
-
Treatment for tuberculosis of the subaxial cervical spine: a systematic review
Archives of Orthopaedic and Trauma Surgery (2021)
-
Midterm surgical results of the lamina with spinous process in treating one-level thoracic or lumbar tuberculosis: a retrospective study
Scientific Reports (2020)
-
MRI and clinical features of acute fungal discitis/osteomyelitis
European Radiology (2020)
-
CT-guided discitis-osteomyelitis biopsies with negative microbiology: how many days should we wait before repeating the biopsy?
Skeletal Radiology (2020)