Abstract
Study design:
Cross-sectional survey.
Objective:
To examine the association between psychological characteristics in self-management and probable depression status in individuals with a traumatic spinal cord injury (SCI).
Setting:
Community-dwelling individuals with traumatic SCI living across Canada.
Methods:
Individuals with SCI were recruited by email via the Rick Hansen Institute as well as an outpatient hospital spinal clinic. Data were collected by self-report using an online survey. Standardized questionnaires were embedded within a larger survey and included the Hospital Anxiety and Depression Scale (HADS), the short version of the Patient Activation Measure (PAM), the Moorong Self-Efficacy Scale (MSES) and the Pearlin-Schooler Mastery Scale (PMS).
Results:
Individuals with probable depression (n=25) had lower self-efficacy (67.9 vs 94.2, P<0.0001), mastery (18.9 vs 22.9, P<0.0001) and patient activation (60.4 vs 71.6, P<0.0001) as well as higher anxiety (9.0 vs 5.5, P<0.0001), compared with their non-depressed counterparts (n=75). A logistic regression determined that lower self-efficacy and mastery scores as well as less time since injury were associated with depression status (P=0.002; P=0.02 and P=0.02, respectively). Individuals with higher anxiety scores were almost 1.5 times more likely to be depressed, while older age was positively associated with depression status (P=0.016 and P=0.024, respectively).
Conclusion:
Interventions for depression in SCI, including a self-management program, should target factors such as self-efficacy and mastery, which could improve secondary medical complications and overall quality of life.
Similar content being viewed by others
Introduction
Individuals with spinal cord injury (SCI) are predisposed to a range of secondary medical complications including urinary tract infections, pressure ulcers, spasticity and pain.1, 2, 3, 4 Many individuals with SCI will also experience significant psychological, social and neurobehavioural issues, and are at increased risk of developing substance abuse problems, low self-esteem and depression.5 Major depression is the most common psychological condition associated with SCI, affecting approximately 25–30% of individuals with SCI living in the community.5 The presence of depression in SCI is associated, in turn, with a variety of poorer outcomes including increased hospitalization periods and secondary medical conditions, as well as decreased social integration, quality of life, and self-care dependency.6 Indeed, our recent qualitative research determined that positive mood was an important facilitator to self-management, and conversely, that negative mood was an important barrier to self-management among individuals with traumatic SCI.7 At the same time, the first part of our results from this national survey on self-management in traumatic SCI revealed that 62.6% were in the ‘maintaining behaviors' segment of self-management/activation (that is, the highest level of self-management/activation), despite the fact that 13% of those individuals in this activation group had a depression score consistent with probable depression.8 Therefore, the current study aims to explore this complexity and examine the association between relevant psychological characteristics in self-management (that is, self-efficacy, mastery and patient activation) and probable depression status in individuals with a traumatic SCI.
Materials and Methods
Study design
A national, cross-sectional study was conducted including individuals with traumatic SCI living in the community in Canada. Research ethics approval was obtained from the University of Toronto (Protocol Reference #26429).
Participants and recruitment
Eligible respondents included individuals who (1) had experienced a traumatic SCI (for example, a fall, motor vehicle accident and sporting accidents); (2) were 18 years of age or older; and (3) were fluent in English. Respondents were recruited by email via the Rick Hansen Institute (RHI) and included individuals who had agreed to be contacted for research purposes. Additional respondents were recruited in-person via the outpatient spinal clinic at Toronto Western Hospital. All respondents were recruited between January and June 2013.
Data collection and survey items
All data were collected by self-report surveys using online software, FluidSurveys (Ottawa, ON, Canada). All respondents were required to provide informed consent before completing the survey (that is, informed consent was not assumed simply by the completion/submission of the online survey).
The specific content of the survey itself was based on the themes that emerged from the first phase of this study on the facilitators and barriers to self-management in traumatic SCI (that is, influence of positive/negative mood and self-efficacy)7 as well as the important psychological elements (that is, module on depression)/underlying theory of the Stanford CDSMP (Chronic Disease Self-Management Program) (that is, social cognitive theory and self-efficacy).9, 10, 11
Standardized questionnaires were used to capture these qualitative themes generated from the first phase of the study as well as the important elements of the CDSMP. These standardized questionnaires were embedded within the larger survey. These questionnaires included the Hospital Anxiety and Depression Scale (HADS),12 the short version of the Patient Activation Measure (PAM),13, 14 the Moorong Self-Efficacy Scale (MSES)15 and the Pearlin-Schooler Mastery Scale (PMS).16
The Hospital Anxiety and Depression Scale
The HADS is a brief, self-report measure that was designed to detect the presence and severity of relatively mild degrees of mood disorder in non-psychiatric, hospital outpatients. It provides separate scores for anxiety and depression. The HADS has 14 items (seven for anxiety and seven for depression) and has established validity and reliability (the Cronbach’s alpha for the HADS-Anxiety has a reported mean of 0.83; the HADS-Depression has a reported mean of 0.82).17 Scores range from 0 to 21, with higher scores indicating greater symptoms of anxiety and depression.12 Cutoff scores of ⩾8 have been used previously to denote probable anxiety or depression.18
The Patient Activation Measure
The PAM is designed to assess an individual’s knowledge, skill and confidence in managing his or her own health care.13, 14 The short version consists of 13 items and uses a Likert-type agreement scale with four response options (1=strongly disagree, 4=strongly agree). The raw score is calculated by adding all of the responses to the 13 questions and range from 13 to 52. These raw scores are converted into activation scores. The converted activation scores range from 0 to 100. Based on these activation scores, individuals are placed into one of four stages of progressive activation: believes active role is important (PAM score of ⩽47.0), has the confidence and knowledge to take action (PAM score of 47.1–55.1), is taking action (PAM score of 55.2–67.0) and is able to stay the course under stress (PAM score of ⩾67.1).13, 14, 19 The previous research has demonstrated that higher PAM scores are associated with healthy behaviors, a higher likelihood of performing self-management and higher medication adherence.20 Individuals scoring at the lower end of the activation may believe that the physician is the one to ‘fix‘ them; mid-range scores may indicate that individuals recognize that they may be involved in their care, but lack the knowledge to do so effectively. Individuals with high PAM scores have gained confidence in their ability to self-manage and make lifestyle changes. The PAM was developed and validated in insured community-based samples in the United States.14, 19
Moorong Self-Efficacy Scale
The MSES was developed to measure an individual’s confidence in performing functional, social, leisure and vocational activities post-SCI. Individuals rate their confidence in their ability to complete the 16 tasks on a seven-point Likert scale (1=very uncertain, 7=very certain). The total scale score is obtained by summing the individual item responses and range from 16 to 112. Higher scores indicate higher perceived self-efficacy. Results have confirmed that the MSES is a valid instrument that is sensitive to real-life changes post-SCI.15
Pearlin-Schooler Mastery Scale
The PMS measures global sense of personal control. It consists of seven items and individuals respond to a five-point Likert scale about the extent to which they agree (5=strongly agree) or disagree (1=strongly disagree) with the various statements. A PMS score ranges from 7 to 35, with a higher score reflecting greater mastery.16
In addition, socio-demographic and injury-related variables were documented including age, sex, marital status, level of education, level of injury and time since injury. Multiple iterations of the survey instrument were produced and reviewed by the research team for flow and content.
Statistical analysis
Respondents’ sociodemographic and psychological characteristics were compared by probable depression status using independent t-test or Mann–Whitney U-test and Chi-Square test. The respondents who completed the survey and the individuals who failed to complete the survey were compared according to age, sex and level of injury using independent t-test and Chi-Square test, or Mann–Whitney U-test. This was to determine whether the ‘completion‘ group was representative of the larger group of eligible individuals identified for the study. For comparison between depressed and non-depressed groups, Fisher’s exact test or Chi-Square test was used for categorical variables (sex, marital status and education) and t-test for continuous variables, including age, anxiety (HADS-Anxiety) and mastery (PMS). Mann–Whitney U-test was used to compare differences in time since injury, self-efficacy (MSES) and patient activation (PAM).
To test for interdependence of the variables, the primary outcome measure of probable depression (HADS-Depression) and the secondary outcome measures of self-efficacy, mastery, patient activation, probable anxiety, time since injury and age were then determined with Spearman’s correlation coefficient. A logistic regression was performed to examine the individual contribution of the above-mentioned independent variables as well as sex, marital status (single vs married/co-habitating) and education (trade/high school or less vs /college/bachelor’s/ post-graduate degree) to the dependent variable, probable depression. All independent variables were entered into the equation at the same time (that is, using the Enter method). Since no predictions had been made regarding the importance or ordering of variables in association with probable depression, this method was considered appropriate. Statistics were calculated using the Statistical Package for the Social Sciences software.
Response characteristics and sample comparability
The current sample of respondents was drawn from the RHISCI Community database. There were a total of 1417 respondents. Of the 1417 individuals, 71 did not wish to be contacted for future studies, leaving 1346 individuals who did want to be contacted for future studies. A random sample of 300 individuals was drawn from this sample of 1346 individuals.
Survey invitations were sent to 300 individuals with SCI including individuals with both traumatic and non-traumatic SCI from the RHI database; four additional individuals were approached about study participation at the Toronto Western Hospital outpatient spinal clinic. The number of individuals with non-traumatic SCI (that is, and therefore ineligible to participate in the study) was unknown. From this, 145 individuals responded to the survey invitation; with 114 respondents completing the entire survey (including the four respondents from the Toronto Western Hospital).
Five individuals had injuries of non-traumatic origin and were therefore excluded (109 individuals with traumatic SCI). A further 10 outliers were excluded due to perfect patient activation scores (a measure of self-management behavior), yielding a final sample size of 99 individuals.
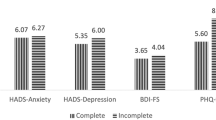
There were no significant differences between individuals who completed the survey (n=114) and individuals who did not complete the survey (n=31) in relation to age and gender (P>0.05). However, there was a significant difference between group membership (that is, individuals who completed the survey and individuals who did not complete the survey) and level of injury (Chi Square (2)=7.915, P<0.05). Individuals were considered in the ‘non-completion‘ group if they only completed basic demographic/clinical information on the online survey and did not complete any of the measures (for example, HADS and PAM).
Results
Sample characteristics and sample characteristics by depression status
The overall respondent characteristics have been previously reported.8 Almost one-quarter (n=24; 24.2%) of the respondents had a depression score consistent with probable depression, while 32.3% (n=32) had a score consistent with probable anxiety. In terms of the patient activation levels, 7.1% (n=7) of the respondents were in the ‘starting to take a role', 9.1% (n=9) were in the ‘building knowledge and confidence', 21.2% (n=21) were in the ‘taking action' and 62.6% (n=62) were in the ‘maintaining behaviors' segments. Thirteen percent of respondents in the highest activation group had a depression score consistent with probable depression (results not tabulated).
The respondent characteristics by probable depression status have been summarized in Table 1. Individuals with scores consistent with probable depression had significantly poorer outcomes across all of the psychological variables. For example, individuals with probable depression had lower self-efficacy (67.9 vs 94.2, P<0.0001), mastery (18.9 vs 22.9, P<0.0001) and patient activation (60.4 vs 71.6, P<0.0001) as well as higher anxiety (9.0 vs 5.5, P<0.0001), compared with their non-depressed counterparts. In addition, there was a significant difference with respect to time since injury in the depressed group vs the non-depressed group, with individuals with probable depression having a mean time since injury of 10.9 vs 19.8 years in the non-depressed group (P=0.001).
Associations between psychological characteristics
As demonstrated in Table 2, there was a significant positive correlation between probable depression and anxiety (r=0.545, P<0.01), indicating that individuals with higher depression scores had higher anxiety scores. There was a significant negative correlation between probable depression and self-efficacy (r=-0.560, P<0.01), indicating that individuals with higher depression scores had lower self-efficacy scores. Characteristics that were significantly (at P<0.01) associated with time since injury were probable depression (r=-0.296, P<0.01) and age (r=0.276, P<0.01), suggesting that increased levels of depression were associated with individuals in earlier stages of their injury and older age, respectively.
Characteristics contributing to depression
Multicollinearity statistics revealed no high intercorrelations (that is, r>0.70) between the psychological and other variables of interest. Thus, nine independent variables were included in the final logistic regression model: self-efficacy, mastery, patient activation, probable anxiety, time since injury and age as well sex, marital status and education. Results of the logistic regression are shown in Table 3. The combination of these nine independent variables accounted for 74% of the variance in this sample’s depression level (adjusted R2=0.742). Of the nine variables, self-efficacy, mastery, probable anxiety, time since injury and age were statistically significant. Lower self-efficacy and mastery scores, as well as less time since injury were associated with probable depression status (P=0.002, P=0.02 and P=0.02, respectively). Individuals with higher anxiety scores were almost 1.5 times more likely to have probable depression, while older age was positively associated with probable depression status (P=0.02 and P=0.02, respectively).
Discussion
The current study aimed to identify some of the psychological characteristics in self-management that are associated with probable depression status in individuals with a traumatic SCI. A main finding of this study was that both lower self-efficacy and mastery (that is, two key psychological characteristics in self-management) were associated with probable depression status in individuals with traumatic SCI. Lower self-efficacy, as measured by the Lorig Chronic Disease Self-Management Scale, has previously been associated with higher depression scores in SCI.21 In fact, individuals with SCI who have lower self-efficacy demonstrate poorer mental health in general and increased secondary complications (that is, poorer self-management).22 Indeed, self-efficacy is the foundational element of the Stanford CDSMP10 and self-efficacy is seen as an early step in causal pathways of behavior change in self-management programs, leading to improved health outcomes (for example, depression). Similarly, a lower mastery score was also associated with probable depression status, and to the best of our knowledge, this direct association has not been previously investigated in a SCI population. Future research should continue to explore the role of mastery in SCI and its impact on other mental health outcomes.
Almost one-third of the respondents had a score consistent with probable anxiety. In a review of psychosocial issues in SCI, Post and van Leeuwen23 indicated that six studies had examined anxiety in SCI. Clinically significant symptoms of anxiety in SCI have been previously reported as ranging from 13.2 to 40%. The current study also determined that a higher anxiety score was significantly associated with probable depression. More recently, Ullrich et al.24 demonstrated that among veterans with SCI and depression, 70% were diagnosed with another psychiatric illness, with post-traumatic stress disorder and other anxiety disorders being the most common. Thus, interventions for depression in SCI, including a self-management program, should consider and address the high likelihood of concurrent anxiety.
Patient activation was not significantly associated with probable depression status in the logistic regression. However, 62.6% (n=62) of the respondents were in the ‘maintaining behaviors' stage of patient activation/self-management, as previously reported.8 This proportion was inconsistent with the previous research on a national (US) sample of individuals 45 years and older, demonstrating 22% were in the ‘maintaining behaviors' stage of patient activation.19 However, similar to the current study, Rask et al.25 determined that 62% of their respondents were in the highest stage of activation in their study of underprivileged individuals with diabetes. As previously noted, future research is needed to confirm the findings related to patient activation and depression in the current study, and explore the use of adapted activation measures that might better discriminate levels of readiness for self-management among individuals with SCI. Nonetheless, patient activation and probable depression were moderately correlated (that is, r=-0.311, P<0.01), and the bivariate analysis demonstrated significantly lower activation scores among the depressed group vs the non-depressed group. Further large-scale research would allow more advanced analyses, such as structural equation modeling, to better estimate the relationships between self-efficacy, mastery, patient activation (that is, self-management behavior) and depression.
Finally, the current study demonstrated that a decreased time since injury and older age were significantly associated with probable depression status. The nature of these associations has been reported inconsistently in the literature. For example, Krause et al.26 reported that individuals with SCI were more likely to suffer from depression with increasing age (consistent with the current study) and a greater number of years post-injury (inconsistent with the current study). Tate et al.27 reported that younger age was associated with depression in SCI. The current findings do appear to mirror the findings of our previous, qualitative research whereby individuals with SCI reported low mood (and/or a lack of readiness for self-management) early in the course of their recovery.7 Relatedly, Pang et al.28 demonstrated that those individuals with increased time since injury have better self-efficacy, but the results did not reach statistical significance. They concluded that it may take time for the newly injured individual to accept his or her own disabilities and learn to cope with the consequences of the condition. It was further suggested that as time progresses, individuals with SCI may come to terms with their own disability and thus develop a better sense of control, and in turn, increased mood. In our previous research,7, 8 individuals with traumatic SCI and their caregivers and health-care professionals reported on the increasing complexities of SCI as individuals live longer, with chronic diseases. Thus, it is plausible that with increasing co-morbidities as individuals with SCI age, they are at an increased risk of depression.
The authors acknowledge some limitations associated with the study. It is likely that the respondents in the current study represented a more engaged and healthier group of individuals with traumatic SCI, and thus the findings may not be representative of the broader group of individuals with traumatic SCI (for example, 95% of the respondents reported having a family physician; 62.6% were in the ‘maintaining behaviors' segment of self-management/activation; all respondents wished to be contacted for research purposes). Furthermore, the design of this study is cross-sectional and therefore cannot draw causal links between probable depression status and the psychological characteristics of interest. Longitudinal research is needed to establish causality and understand changes in mood levels among individuals with SCI over time. Finally, self-report measures of psychological outcome are considered subjective (vs a structured diagnostic interview), and thus presented a testing bias. Future SCI research could therefore incorporate clinician-based ratings, consistent with recommendations for clinical trials.
The current study determined that low self-efficacy and low mastery were significantly associated with probable depression status. These findings are consistent with the foundational role that self-efficacy, in particular, plays in many self-management programs. A higher anxiety score, less time since injury and older age were also significantly associated with probable depression. Future, large-scale research is needed to better estimate the relationships between self-efficacy, mastery, patient activation (that is, self-management behavior), and depression and how these constructs evolve over time to plan rehabilitation and (long-term) community interventions that are targeted to the needs of the individual. However, the current study suggests that interventions for depression in SCI in clinical/rehabilitation and community practice, including a self-management program, should specifically target factors such as self-efficacy and mastery to improve depression in SCI. These efforts could subsequently improve other outcomes including secondary medical complications and overall quality of life.
Data Archiving
There were no data to deposit.
References
Johnson RL, Gerhart KA, McCray J, Menconi JC, Whiteneck GG . Secondary conditions following spinal cord injury in a population-based sample. Spinal Cord 1998; 36: 45–50.
McKinley WO, Seel RT, Hardman JT . Nontraumatic spinal cord injury: incidence, epidemiology, and functional outcome. Arch Phys Med Rehabil 1999; 80: 619–623.
Dryden DM, Saunders LD, Rowe BH, May LA, Yiannakoulias N, Svenson LW et al. Utilization of health services following spinal cord injury: a 6-year follow-up study. Spinal Cord 2004; 42: 513–525.
Jaglal SB, Munce SEP, Guilcher SJT, Couris CM, Fung K, Craven BC et al. Health system factors associated with rehosptialisations after traumatic spinal cord injury: a population-based study. Spinal Cord 2009; 47: 604–609.
Craig A, Tran Y, Middleton J . Psychological morbidity and spinal cord injury: a systematic review. Spinal Cord 2009; 47: 108–114.
Elliott TR, Kennedy P . Treatment of depression following spinal cord injury: an evidence-based review. Rehabil Psychol 2004; 49: 134–139.
Munce SE, Webster F, Fehlings MG, Straus SE, Jang E, Jaglal SB . Perceived facilitators and barriers to self-management in individuals with traumatic spinal cord injury: a qualitative descriptive study. BMC Neurol 2014; 14: 48.
Munce SE, Fehlings MG, Straus SE, Nugaeva N, Jang E, Jaglal SB . Views of people with traumatic spinal cord injury about the components of self-management programs and program delivery: a Canadian pilot study. BMC Neurol 2014; 14: 209.
Lorig KR, Sobel D, Stewart A, Brown B, Bandura A, Ritter P et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: a randomized trial. Med Care 1999; 37: 5–14.
Lorig KR, Ritter P, Stewart AL, Sobel DS, Brown BW Jr, Bandura A et al. Chronic disease self-management program: 2-year health status and health care utilization outcomes. Med Care 2001; 39: 1217–1223.
Bandura A . Health promotion by social cognitive means. Health Educ Behav 2004; 31: 143–164.
Zigmond AS, Snaith RP . The hospital anxiety and depression scale. Acta Psychiatr Scand 1983; 67: 361–370.
Hibbard JH, Stockard J, Mahoney ER, Tusler M . Development of the patient activation measure: conceptualizing and measuring activation in patient and consumers. Health Serv Res 2004; 39: 1005–1026.
Hibbard JH, Mahoney E, Stockard J, Tusler M . Development and testing of a short form of the patient activation measure (PAM). Health Serv Res 2005; 40: 1918–1930.
Middleton JW, Tate RL, Geraghty TJ . Self-efficacy and spinal cord injury: psychometric properties of a new scale. Rehabil Psychol 2003; 48: 281–288.
Pearlin LI, Schooler C . The structure of coping. J Health Soc Behav 1978; 19: 2–21.
Bjelland I, Dahl AA, Haug TT, Neckelmann D . The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 2002; 52: 69–77.
Barlow JH, Turner AP, Edwards R, Gilchrist M . A randomised controlled trial of lay-led self-management for people with multiple sclerosis. Patient Educ Couns 2009; 77: 81–89.
Hibbard JH, Tusler M . Accessing activation stage and employing a “next steps” approach to supporting patient self-management. J Ambul Care Manage 2007; 30: 2–8.
Mosen D, Schmittdiel J, Hibbard JH, Sobel D, Remmers C, Bellows J . Is patient activation associated with outcomes of care for adults with chronic conditions? J Ambul Care Manage 2007; 30: 21–29.
Bombardier CH, Fann JR, Tate DG, Richards JS, Wilson CS, Warren AM et al. An exploration of modifiable risk factors for depression after spinal cord injury: which factors should we target? Arch Phys Med Rehabil 2012; 93: 775–781.
Suzuki R, Krahn GL, McCarthy MJ, Adams EJ . Understanding health outcomes: physical secondary conditions in people with spinal cord injury. Rehabil Psychol 2007; 52: 338–350.
Post MW, van Leeuwen CM . Psychosocial issues in spinal cord injury: a review. Spinal Cord 2012; 50: 382–389.
Ullrich PM, Smith BM, Blow FC, Valenstein M, Weaver FM . Depression, healthcare utilization, and comorbid psychiatric disorders after spinal cord injury. J Spinal Cord Med 2014; 37: 40–45.
Rask KJ, Ziemer DC, Kohler SA, Hawley JN, Arinde FJ, Barnes CS . Patient activation is associated with healthy behaviors and ease in managing diabetes in an indigent population. Diabetes Educ 2009; 35: 622–630.
Krause JS, Coker J, Charlifue C, Whiteneck GG . Depression and subjective well-being among 97 American Indians with spinal cord injury: a descriptive study. Rehabil Psychol 1999; 44: 354–372.
Tate D, Forchheimer M, Maynard F, Dijkers M . Predicting depression and psychological distress in persons with spinal cord injury based on indicators of handicap. Am J Phys Med Rehabil 1994; 73: 175–183.
Pang MY, Eng JJ, Lin KH, Tang PF, Hung C, Wang YH . Association of depression and pain interference with disease-management self-efficacy in community-dwelling individuals with spinal cord injury. J Rehabil Med 2009; 41: 1068–1073.
Acknowledgements
SEP Munce was supported by a Frederick Banting and Charles Best Doctoral Research Award from the Canadian Institutes of Health Research and a Knowledge Translation Canada Fellowship Award. We are grateful to the Rick Hansen Institute and Toronto Western Hospital for assisting us in the recruitment of participants.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Munce, S., Straus, S., Fehlings, M. et al. Impact of psychological characteristics in self-management in individuals with traumatic spinal cord injury. Spinal Cord 54, 29–33 (2016). https://doi.org/10.1038/sc.2015.91
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2015.91
This article is cited by
-
Learning self-care skills after spinal cord injury: a qualitative study
BMC Psychology (2021)
-
Peer mentorship for adults with spinal cord injury: a static group comparison between mentees and non-mentees’ reported coping strategies
Spinal Cord (2018)
-
Associations between disability-management self-efficacy, participation and life satisfaction in people with long-standing spinal cord injury
Spinal Cord (2017)
-
Depressive mood in adults with spinal cord injury as they transition from an inpatient to a community setting: secondary analyses from a clinical trial
Spinal Cord (2017)