Abstract
Study design:
Experimental, controlled, animal study.
Objectives:
To evaluate the functional effect of hyperbaric oxygen therapy administered shortly, one day after, and no intervention (control) in standardized experimental spinal cord lesions in Wistar rats.
Setting:
São Paulo, Brazil.
Methods:
In all, 30 Wistar rats with spinal cord lesions were divided into three groups: one group was submitted to hyperbaric oxygen therapy beginning half an hour after the lesion and with a total of 10 one-hour sessions, one session per day, at 2 atm; the second received the same treatment, but beginning on the day after the lesion; and the third received no treatment (control). The Basso, Beattie and Bresnahan scales were used for functional evaluation on the second day after the lesion and then weekly, until being killed 1 month later.
Results:
There were no significant differences between the groups in the functional analysis on the second day after the lesion. There was no functional difference comparing Groups 1 and 2 (treated shortly after or one day after) in any evaluation moment. On the 7th day, as well as on the 21st and 28th postoperative days, the evaluation showed that Groups 1 and 2 performed significantly better than the control group (receiving no therapy).
Conclusion:
Hyperbaric chamber therapy is beneficial in the functional recovery of spinal cord lesions in rats, if it is first administered just after spinal cord injury or within 24 h.
Similar content being viewed by others

Introduction
Clinical and experimental researches on spinal cord trauma have raised several hypotheses with regard to the pathophysiology of secondary injury that occurs immediately after the initial injury (primary). Most current efforts are directed to minimizing this type of injury, by acting directly on its causes. Recent studies1, 2 indicate that the process is characterized by an initial ischemia (affecting mainly the gray matter), extending rostrally and caudally to the lesion. At this point, the decrease in oxygen and nutrients supply to the cells reduces the amount of available ATP, causing a malfunction of the electrolyte pumps in the cell membrane, resulting in changes in the intra- and extracellular ionic concentrations.3, 4 This process is responsible for edema and cell death and for the secretion of aminoacidic neurotransmitters, for example, the glutamate.5 The decrease in ATP also stimulates the glycolytic pathway, increasing lactate and decreasing the local pH, which results later in vasodilation and increased blood flow, contributing to the formation of free radicals,6 and causing cell death. Although these processes occur mainly in the gray matter, the release of lytic enzymes and free radicals eventually damages the surrounding white matter. These metabolic products also cause inflammation and demyelination.1
In the search of potential of glucocorticoids to reduce this injury, methylprednisolone has been brought to the clinical use. This drug has beneficial effects when administered in a short period of time after the lesion,7, 8 but can also be accompanied by some side effects, as a deleterious process to neuronal regeneration (by inhibiting the activity of immune cells and antigen processing by macrophages,9 mild neutropenia, exacerbation of post-ischemic necrosis and inhibition of budding of axons.8 This study aims to find an alternative way to reduce the secondary spinal cord lesion while avoiding those side effects, or one adjuvant therapy to existing treatments. One way to conquer this challenge could be the investigation of the role of oxygen in lesion repair.
Much of the secondary injury process is triggered mainly by the depletion of oxygen, and experiments have tried to correct some of this deficit by using the hyperbaric oxygen therapy. This therapy is based on the obtainment of high tissue oxygen partial pressures, when breathing pure oxygen inside a hyperbaric chamber, and a higher-than-atmospheric pressure. This therapeutic approach had positive results in animals10, 11 and humans.12, 13, 14 Some of these studies were performed in the supra-segmental nervous system.15 However, risks were also appointed for such approaches,16, 17 potentially worsening neurological recovery. Our efforts focus on defining the real influence of hyperbaric oxygen therapy in the recovery of the injured spinal cord, making a standardized evaluation of the function, and on investigating if time would play a role in the hyperbaric therapy results.
The objective of this study was to evaluate the functional effect of hyperbaric oxygen therapy administered shortly, compared with that administered one day after and no intervention (control) in standardized experimental spinal cord lesions in Wistar rats.
Materials and methods
In this experimental, controlled trial, the functional results of the use of hyperbaric oxygen therapy in rats with induced spinal cord lesions are evaluated. All applicable institutional and governmental regulations on the ethical use of animals were followed during the course of this research. The institution's Ethical Committee approved the research protocol.
Design, animals and hyperbaric therapy settings
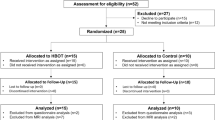
Healthy Wistar rats, aged 12 weeks old, and weighing 260–340 g, all from the same vivarium, were used. Rats not familiarized with each other were kept in separate cages to prevent aggressive behavior. Rats that died at any time after spinal cord lesion, and any rat exhibiting uncontrolled autophagic or mutilating behavior were excluded. Animals would also be excluded if they presented macroscopic spinal cord anomalies (malformations) previously detected on surgery, or those that still presented normal movement after the lesion (21 points on the Basso Beattie and Bresnahan scale).18 Rats with urinary infection refractory to antibiotic therapy were excluded.
All rats were submitted to laminectomy and spinal cord lesions using the NYU Impactor device, as described in detail below. They were anesthetized before the laminectomy and spinal cord lesion procedures, with a dose of 55–75 mg/kg body weight of sodium pentobarbital intraperitoneally. At the end of the 30-day experimental period, all the rats were weighed and were euthanized with a lethal dose of pentobarbital (140 mg/kg), also administered intraperitoneally.
The animals were divided into three groups: Groups 1 and 2 received hyperbaric therapy (HBO) (10 sessions) and Group 3 received no therapy (control). In all, 30 rats were used, 10 in each group. The only difference between Groups 1 and 2 is the moment of hyperbaric therapy initiation: Group 1 animals were taken to the hyperbaric chamber 1 after the spinal cord lesion was produced. Group 2 started to receive this therapy only 24 h after the lesion.
Hyperbaric therapy setting
Pressure was set always at 2 atms as set by Shiokawa et al.,19 and, apart from the first one, the rats received nine further 1-hour sessions, one per day,19 always in the same time of the day. The animals received therapy in a tubular, transparent, hyperbaric chamber, measuring 770 mm in length and 180 mm in internal diameter, with a useful height of 150 mm (between the platform and the upper wall; Figure 1). The chamber could hold 10 rats simultaneously, and it was regulated to provide 14 l of oxygen per minute.
Laminectomy and spinal cord lesion procedure
The anesthetic dose varied a little between the animals, but it was expected to take effect after 5 min and to last for at least 2 h. If any rat were found to be active or wake up during the procedures, the experiment would be interrupted.
The laminectomy method was already described by our team in this same journal.20 Briefly, a long, dorsal, medial incision was made to expose the posterior vertebral arches, from T8 to T12. The spinous process and laminae of vertebrae T9 and T10 were removed, to expose the spinal cord and enable positioning (puncture) of the tip of the NYU Impactor device, to perform the spinal cord lesion.
The protocol for spinal cord lesion, described elsewhere,20 consists of producing a spinal cord lesion with the computerized device NYU Impactor (New York University Spinal Cord Contusion System), using a falling weight. The falling of an impact rod weighing 10 g, compressing the spinal cord for 15 s, produced the impact on the spinal cord. However, different from previous studies,20, 21 the height was standardized to be of 25 mm (instead of the moderate lesions caused by the fall from 12.5 mm). The lesions were homogeneous and reproducible.
The device was adjusted to produce the impact between the superior margin of T9 and the inferior margin of T10. Immediately after the impact, the shaft was raised, the animal was placed in a warm surface and the site of the contusion was inspected in search for bleeding. Where hemorrhaging was present, hemostasia was performed. The contusion site was washed with physiological sodium chloride solution at room temperature. The paravertebral muscles were sutured using 5.0-monofilament nylon and the skin with 3-0 nylon suture stitches.
Animal care after the lesion
The animals received prophylactic cephalothin subcutaneously (25 mg/kg body weight) immediately after the lesion, and once a day for the next 7 days, to prevent urinary tract or wound infection. The rats' bladders were pressed, to empty them, periodically. Those that presented infection received levofloxacin (2.5 mg/kg, for 10 days). If after 10 days of therapy blood in the urine or clinical signs of infection were found, the rat was killed and excluded from the statistical analysis.
Once they had recovered from the anesthesia, the animals were allowed food and water. Weight was evaluated on the 2nd, 7th, 14th, 21st and 28th days after operation. On the 28th day, the rats were killed and histopathological analysis was performed.
Functional analysis
After the spinal cord lesion, the Basso Beattie and Bresnahan scale was used to evaluate the recovery of locomotor capacity,18 simultaneously by two trained observes who had no knowledge of the intervention to which each rat had been submitted (blind to the procedure). The final report of the evaluation, carried out on days 2, 7, 14, 21 and 28 after surgery, was made by consensus or, in the case of a disagreement, the lowest value was recorded. For this analysis, the MASCIS (Multicenter Animal Spinal Cord Injury Study),20, 22 standardized for Wistar rats, was adopted.
Pathological analysis
The segment of spine from T8 to T12 was removed and a visual macroscopic evaluation of the spinal cord at the contusion site was carried out, to check for any anomaly (exclusion criteria). The spinal cord, preserved in 10% formaldehyde solution, was sent for microscopic analysis. Histological cross-sections were made on the axial plane of the spinal cord segment, at 2 mm intervals, representing the entire lesioned area, to a length of 1 cm from the center of the lesion, and adjacent areas. This material was processed and dehydrated in a series of alcohols, then diaphanized in xylol and embedded in paraffin. In all, 5-μm-thick histological sections were produced in a microtome, 0.5 cm above and 0.5 cm below the central area of the lesion. The material was then fixed on glass slides stained with hematoxylin–eosin. Necrosis, hemorrhage, hypermia, degeneration of nervous substances (cystic degeneration) and cell infiltration were recorded as absent (0), slight (1), moderate (2) and accentuated (3).6, 23
The variables in the pathological analysis were necrosis, hyperemia, hemorrhage, degeneration of the nervous substance and cellular infiltration.6, 23 The presence of each variable was registered three times for each rat: one corresponding to the lesion itself, one to the cranial region of the lesion and the last to the caudal area of the lesion. Therefore, pathological analysis yielded a score between 0 and 15.
Statistical analysis
The non-parametric Mann–Whitney test was used in functional and histological analysis. In functional analysis, each limb was considered as one individual case. P-values of <0.05 were considered significant.
Results
Exclusion of animals
On the 6th day after the procedure, one rat of Group 2 (no. 12) was found dead in the cage for urinary infection. On the 7th day, one rat of Group 1 (no. 3) had hematuria and started to receive levofloxacin. Still, this animal died on the 10th day. Therefore, one rat was excluded from Group 1 and one from Group 2 from the analysis. No rat in the control group was excluded. From the 7th day on, all rats homogeneously gained weight.
Functional analyses
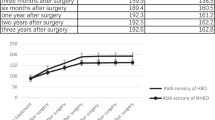
There were no significant differences between the groups in the functional analysis on the second day after the lesion (P>0.05). There was no functional difference comparing Groups 1 and 2 (treated shortly after or one day after) in any evaluation moment. On the 7th day, as well as on the 21st and 28th postoperative days, the evaluation showed that Groups 1 and 2 performed significantly better than the control group (receiving no therapy) (P<0.05). Only on the 14th day the difference between Groups 1 and 3 did not show significance (P=0.001). Table 1 shows Basso Beattie and Bresnahan results, Table 2 details statistical results (Mann–Whitney test) and Figure 2 demonstrates evolution of mean functional scores.
Histological analysis
There was no significant difference in the tissue analysis comparing groups and samples in any time (that is, hyperbaric oxygen therapy did not interfere in histological results). Table 3 shows P-values.
Discussion
Hyperbaric oxygen therapy is considered an interesting therapeutic modality, which is known to reduce oxidative stress itself. During and shortly after treatment, the therapy leads to a hypersaturating circulating plasma with dissolved oxygen, resulting in a transiently increased diffusion gradient between both the circulation and the surrounding tissues and driving transport of oxygen into the interstitium and tissues.10
In this study, there were no significant differences between the groups of rats on the 2nd postoperative day, which indicates homogeneity in the experimental production of the lesions. Indeed, the method of production of the spinal cord lesions had already been proved reproducible before.20, 21
The functional analysis reflects the ability of the individual to perform daily activities—and this is very important for humans. In our study, rats that were treated in the hyperbaric chamber had better functional results, compared with controls, in all evaluations—except for the 14th postoperative day, when Group 1 had the same performance as Group 3. In Figure 2, it is possible to see that Group 3 had a better performance than the other two groups between 7th and 14th days, when the groups got closer to each other. In the next periods, 21st and 28th days, Groups 1 and 2 again distanced themselves from Group 3.
The comparison between Groups 1 and 2 (both treated, but in different moments) has shown that they were not significantly different. This finding indicates that the time between the lesion and the administration of hyperbaric therapy does not interfere in the efficacy of the treatment. A delay would not hamper clinical results, therefore.
With regard to the histological findings, there was no significant difference in the tissue analysis comparing groups and samples in any time. This does not mean that the tissues are equal: the method of histological evaluation with hematoxylin–eosin can show necrosis, hemorrhage, hypermia, degeneration of nervous substances (cystic degeneration) and cell infiltration that had not changed with hyperbaric oxygen therapy, but the result could be different if we had used other techniques of neurochemical assays to access activities of antioxidant enzymes, like Mn-superoxide dismutase and catalase dosage and expression of antiapoptotic protein in the mitochondria, which are more sensitive methods to differ tissues with ischemic degeneration.6, 24
Supplementation with biological and cell resources should constitute the next steps to be taken, and may explain the difference in performance of the experimental groups that we have seen here. Maybe a study with antioxidant enzymes in different postoperative moments (days 7, 14, 21 and 28) could help to explain the absence of a significant difference in the functional analysis on day 7. Maybe it could also help to explain the hyperoxygen mechanism in the spinal cord lesion metabolism.
The finding of a beneficial functional effect of hyperbaric therapy in experimental spinal cord lesions suggests applicability in humans. Variations in the intensity, dosage, duration and periodicity of the therapy should be tested in other studies.
Conclusion
Hyperbaric chamber therapy proved to be beneficial in the functional recovery of spinal cord lesions in rats if it is first administered just after spinal cord injury or within 24 h post-spinal cord injury. The effect is comparable and better than that in the control group.
Data Archiving
There were no data to deposit.
References
Aslan A, Cemek M, Eser O, Altunbas K, Buyukokuroglu ME, Cosar M et al. Does dexmedetomidine reduce secondary damage after spinal cord injury? An experimental study. Eur Spine J 2009; 18: 336–344.
Cristante AF, Barros-Filho TE, Tatsui N, Mendrone A, Caldas JG, Camargo A et al. Stem cells in the treatment of chronic spinal cord injury: evaluation of somatosensitive evoked potentials in 39 patients. Spinal Cord 2009; 47: 733–738.
Fouad K, Ghosh M, Vavrek R, Tse AD, Pearse DD . Dose and chemical modification considerations for continuous cyclic AMP analog delivery to the injured CNS. J Neurotrauma 2009; 26: 733–740.
Ahn YH, Lee G, Kang SK . Molecular insights of the injured lesions of rat spinal cords: inflammation, apoptosis, and cell survival. Biochem Biophys Res Commun 2006; 348: 560–570.
Guimaraes PE, Fridman C, Gregorio SP, Kalil EM, Cristante AF, Teixeira WG et al. DNA polymorphisms as tools for spinal cord injury research. Spinal Cord 2009; 47: 171–175.
Cristante AF, Barros Filho TE, Oliveira RP, Marcon RM, Rocha ID, Hanania FR et al. Antioxidative therapy in contusion spinal cord injury. Spinal Cord 2009; 47: 458–463.
Xu WB, Lv G, Wang YF, Lu XH, Huang T, Zhu Y et al. Combination of dexamethasone and aminoguanidine reduces secondary damage in compression spinal cord injury. Cell Mol Neurobiol 2009; 29: 683–689.
Bracken MB, Shepard MJ, Holford TR, Leo-Summers L, Aldrich EF, Fazl M et al. Administration of methylprednisolone for 24 or 48 h or tirilazad mesylate for 48 h in the treatment of acute spinal cord injury. Results of the Third National Acute Spinal Cord Injury Randomized Controlled Trial. National Acute Spinal Cord Injury Study. JAMA 1997; 277: 1597–1604.
Genovese T, Mazzon E, Crisafulli C, Esposito E, Di Paola R, Muia C et al. Combination of dexamethasone and etanercept reduces secondary damage in experimental spinal cord trauma. Neuroscience 2007; 150: 168–181.
Topuz K, Colak A, Cemil B, Kutlay M, Demircan MN, Simsek H et al. Combined hyperbaric oxygen and hypothermia treatment on oxidative stress parameters after spinal cord injury: an experimental study. Arch Med Res 2010; 41: 506–512.
Tai PA, Chang CK, Niu KC, Lin MT, Chiu WT, Lin CM . Attenuating experimental spinal cord injury by hyperbaric oxygen: stimulating production of vasculoendothelial and glial cell line-derived neurotrophic growth factors and interleukin-10. J Neurotrauma 2010; 27: 1121–1127.
Al-Waili NS, Butler GJ, Beale J, Abdullah MS, Hamilton RW, Lee BY et al. Hyperbaric oxygen in the treatment of patients with cerebral stroke, brain trauma, and neurologic disease. Adv Ther 2005; 22: 659–678.
Rockswold SB, Rockswold GL, Defillo A . Hyperbaric oxygen in traumatic brain injury. Neurol Res 2007; 29: 162–172.
Asamoto S, Sugiyama H, Doi H, Iida M, Nagao T, Matsumoto K . Hyperbaric oxygen (HBO) therapy for acute traumatic cervical spinal cord injury. Spinal Cord 2000; 38: 538–540.
Kohshi K . Hyperbaric oxygen therapy for neurologic emergency and neurosurgical diseases: a systematic review of the literature. J UOEH 2003; 25: 419–433.
Huang KC, Hsu WH, Peng KT, Huang TJ, Hsu RW . Hyperbaric oxygen therapy in orthopedic conditions: an evaluation of safety. J Trauma 2006; 61: 913–917.
Ors F, Sonmez G, Yildiz S, Uzun G, Senol MG, Mutlu H et al. Incidence of ischemic brain lesions in hyperbaric chamber inside attendants. Adv Ther 2006; 23: 1009–1015.
Basso DM, Beattie MS, Bresnahan JC . A sensitive and reliable locomotor rating scale for open field testing in rats. J Neurotrauma 1995; 12: 1–21.
Shiokawa O, Fujishima M, Yanai T, Ibayashi S, Ueda K, Yagi H . Hyperbaric oxygen therapy in experimentally induced acute cerebral ischemia. Undersea Biomed Res 1986; 13: 337–344.
Marcon RM, Cristante AF, de Barros Filho TE, de Oliveira RP, dos Santos GB . Potentializing the effects of GM1 by hyperbaric oxygen therapy in acute experimental spinal cord lesion in rats. Spinal Cord 2010; 48: 808–813.
Narazaki DK, Barros Filho TE, Oliveira CR, Cristante AF, Iutaka AS, Marcon RM et al. Spinal cord regeneration: the action of neurotrophin-3 in spinal cord injury in rats. Clinics (Sao Paulo) 2006; 61: 453–460.
Basso DM, Beattie MS, Bresnahan JC, Anderson DK, Faden AI, Gruner JA et al. MASCIS evaluation of open field locomotor scores: effects of experience and teamwork on reliability. Multicenter Animal Spinal Cord Injury Study. J Neurotrauma 1996; 13: 343–359.
Galvão PEC, Cristante AF, Jorge HMH, Damasceno ML, Marcon RM, Oliveira RP et al. Avaliação funcional e histológica da oxigenoterapia hiperbárica em ratos com lesão medular [Functional and histologic evaluation of hyperbaric oxygen therapy in rats with spinal cord injury]. Acta Ortop Bras 2011; 19: 10–16.
Wang L, Li W, Kang Z, Liu Y, Deng X, Tao H et al. Hyperbaric oxygen preconditioning attenuates early apoptosis after spinal cord ischemia in rats. J Neurotrauma 2009; 26: 55–66.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Cristante, A., Damasceno, M., Barros Filho, T. et al. Evaluation of the effects of hyperbaric oxygen therapy for spinal cord lesion in correlation with the moment of intervention. Spinal Cord 50, 502–506 (2012). https://doi.org/10.1038/sc.2012.16
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2012.16
Keywords
This article is cited by
-
Effects of hyperbaric oxygen therapy on postoperative recovery after incomplete cervical spinal cord injury
Spinal Cord (2022)
-
Effects of tacrolimus and erythropoietin in experimental spinal cord lesion in rats: functional and histological evaluation
Spinal Cord (2016)
-
Effects of antidepressant and treadmill gait training on recovery from spinal cord injury in rats
Spinal Cord (2013)