Abstract
Study design:
Longitudinal.
Objective:
To investigate the relative importance of personality traits, emotional distress and pain as predictors of functional health status in patients with spinal cord injury (SCI) or multiple traumas (MTs).
Setting:
Sunnaas Rehabilitation Hospital, Norway.
Methods:
Data were obtained from SCI and MT patients at admission (n=101) and at discharge (n=87) from rehabilitation, as well as 4 years post injury (n=75). The primary outcome measure was the sickness impact profile (SIP). Personality traits, that is, dispositional optimism and positive/negative affectivity, were measured using the Life Orientation Test-Revised and the Positive Affect and Negative Affect Schedule, respectively.
Results:
Using hierarchical regression analysis, dispositional optimism and pain emerged as the most robust predictors of functional health status. Generally, these two variables accounted for a substantial part of the variance (that is, 20–40%) in the SIP scales. Significant correlations between pain and anxiety/depression were found in all phases of the study, and at follow-up depression level appeared as an independent predictor of functional health.
Conclusion:
The substantial predictive power, in terms of explained variance, of dispositional optimism, pain and depression/anxiety, indicates that these variables may be of practical–clinical importance in a rehabilitation setting. Specifically, patients characterized by low optimism, combined with presence of pain and depression/anxiety, may constitute a high-risk group for disability and reduced quality of life. On the other hand, high optimism should be regarded as a resilience characteristic, protecting the individual against long-term sequelae of severe physical injury.
Similar content being viewed by others
Introduction
The ultimate goal of rehabilitation of patients who have acquired a severe physical injury, such as spinal cord injury (SCI) or multiple traumas (MTs), might be described as reducing disabilities to minimize handicaps.1 In practice, this amounts to improving the patients’ function in daily activities and generally to making them feel better. Measurements of how people are feeling and adapting in this context might be referred to as health-related quality of life or functional health status, depending on the type of measures used. In order to assess the influence of injury/disease and treatment on the daily life of patients, functional health and health-related quality of life as outcome measures have been increasingly used in addition to ordinary medical criteria.2
SCI and MT often cause severe disabilities and dramatic changes in the life of the afflicted person and are usually associated with reduced functional health levels.2, 3 The findings are not unequivocal, however. For example, several studies suggest that health-related quality of life after SCI or MT is not always influenced by the severity of either impairment or disability.3, 4 The causes of these findings are unclear, but it is assumed that psychological adaptive responses are involved.3 Previous research on SCI and MT populations has included a variety of functional health determinants, such as demographic factors and co-morbidity,2 physical fitness5 and social support.6 Yet, as emphasized by Post and Noreau,7 there is a lack of longitudinal studies, particularly of the effect of personal characteristics (for example, personality, coping strategies), in this research area.
In a recent study of adjustment patterns in SCI and MT patients in a rehabilitation setting,8 resilience was the most common trajectory. Resilience was defined as the ability of individuals who are facing a severe and potentially disabling physical injury to maintain a relatively stable and healthy level of psychological and social functioning, and to maintain positive emotions and positive perception of the self and the future.8 Importantly, compared with the other two trajectories (that is, recovery and distress) that were identified in this study, the resilient patients evidenced higher initial optimism levels, more positive affect (PA) (and less negative affect (NA)) and less pain.
In this study the utility of these resilience characteristics as predictors of functional health in the same unselected patient sample was explored. Thus, the main aim of this study was to investigate to what extent functional health status could be predicted by personality traits (that is, dispositional optimism and positive/negative affectivity), emotional distress and pain levels.
Materials and methods
Participants
This study was conducted at Sunnaas Rehabilitation Hospital (SRH), the most specialized rehabilitation hospital in Norway. The participants comprised inpatients with MTs, SCI or both, admitted to SRH during a 2-year period from February 2003 to January 2005. Exclusion criteria were severe cognitive deficits or practical problems with carrying out the interview because of severe medical complications, psychosis or other psychiatric illness, or insufficient understanding of the Norwegian language. Procedures for data collection as well as demographic and medical characteristics of the sample at admission (T1) and discharge (T2) have been described in detail in previous publications.4, 8 The follow-up study was conducted 4 years after discharge (T3) from SRH, from February 2007 through February 2009. Of the 101 patients who were included at T1, 85 were contacted at follow-up and asked to participate (9 patients were deceased, 6 could not be located and 1 was excluded because the diagnosis had been changed to multiple sclerosis). Of these, 10 refused to participate, leaving us with a net sample of 75 individuals.
All traumatic injuries were classified by the Abbreviated Injury Scale and the New Injury Severity Score (NISS),9 with a NISS score above 15 considered a serious injury. A MT was defined as having a NISS score above 15 and with at least two injuries classified in the Abbreviated Injury Scale.9 Both patients with traumatically acquired SCI (that is, caused by accidents) and nontraumatic SCI (that is, caused by infections and vascular lesions) were included. A total of 19 patients had MT in addition to SCI. The project was approved by the Regional Committee for Medical Ethics, South-East Norway.
Sickness impact profile (SIP)
The SIP is a well-established generic measure of functional health status,10, 11 yielding scores for all essential facets of this construct.1 It consists of 136 statements about functional status in 12 categories. Two dimension scores and the overall SIP score were calculated, with higher scores indicating more dysfunction. The physical dimension comprises the categories ambulation, mobility, body care and movement. The psychosocial dimension encompasses the alertness behavior, social interaction, emotional behavior and communication categories. The remaining independent categories are sleep and rest, eating, work, home management and recreation and pastimes. Psychometric properties of the SIP are generally very good,12 and the instrument has been used in a broad range of studies, including studies of consecutive trauma patients or groups with single diagnoses such as SCI.2
Psychological measures
Symptoms of posttraumatic stress were measured with the Impact of Event Scale-Revised (IES-R).13 The IES-R is a 22-item scale that measures all three core characteristics of post traumatic stress disorder (PTSD), that is, intrusion, avoidance and hyperarousal. The Hospital Anxiety and Depression Scale (HADS)14 was used to identify symptoms of anxiety (HADS-A) and depression (HADS-D). A score of 0–7 for either subscale is regarded as being in the normal range, and a score of 8 or higher indicates probable presence (‘caseness’) of depression or anxiety disorder. Pain was assessed with a yes/no question and a visual analogue scale indicating the maximal experience of pain during the last week on a scale ranging from 0 to 10.
PA and NA were measured using the Positive Affect and Negative Affect Schedule (PANAS).15 The PANAS consists of 10 adjectives in two subscales: PA and NA. In this study, results based on the trait version of the instrument are reported. Finally, to measure the personality trait dispositional optimism, a revised version of the Life Orientation Test (LOT-R) was used.16, 17 The personality instruments were administered in the initial phase of the study (see Table 1).
All the measures are well established, and we used Norwegian language versions. Internal consistency for the scales was acceptable in our sample, with Cronbach's α ranging from 0.92 (IES-R) to 0.80 (HADS-D).
Statistical analyses
Multivariate analysis of variance and paired samples t-tests were conducted to analyze within-subject changes in distress and pain over time. Correlation analysis was performed to explore associations among the study variables. In order to examine the effects of sets of independent variables on SIP scores, hierarchical regression analysis was used. Because of the large number of study variables relative to the number of subjects, a careful selection of independent variables to be included in the regression analyses was performed. Initial correlation and regression analyses revealed no consistent effects of NISS (that is, injury severity) or age, sex and education on the dependent variables. Consequently, these variables were not included in further analyses. Furthermore, when the three personality measures were entered simultaneously as independent variables in regression analyses, only the LOT-R was found to have significant effects on the SIP scales. In a next step, a series of hierarchical linear regressions were conducted, entering, first, the LOT-R, then maximum pain rating and in the third block of variables HADS-A, HADS-D and IES-R. In these analyses, consistent effects of the pain variables, in addition to the LOT-R, were found. No significant parameters or further increases in R2 occurred when the emotional distress indices obtained at admission or discharge were entered in the third block, but significant effects of HADS-D at follow-up were demonstrated (Table 3, model 3). All significant predictors that emerged from these analyses were then included in a final set of regression models (that is, model 1–3 reported in Table 3), in which the LOT-R (T1) was entered in the first step, maximum pain ratings (T1–T3) in the second and, in model 3, HADS-D in the third. Changes in explained variance (R2 change) across blocks were determined using the F-test.
Results
Mean age for the 75 patients (67% men) who participated at follow-up was 45 years (s.d. 14.5) and mean years of education was 13 (s.d. 3.1). Since some of the respondents from T1 did not participate at T3 (n=26) because of the reasons explained above, analyses were conducted to compare the respondents with the nonrespondents at T3. Briefly, these results showed that the nonresponders had a significantly shorter stay at the rehabilitation hospital, were less optimistic and had lower trait PA.
As shown in Table 1, there were no significant changes in anxiety or post-traumatic stress symptoms across the time points. However, an increase in depression at follow-up as compared with depression level at discharge was observed (P<0.05). Although the mean levels of anxiety and depression are within the normal range (0–7), frequency analyses revealed that in each phase of the study 20–25% of the participants exhibited elevated (⩾8) HADS-A scores. The proportion of participants with elevated HADS-D scores was about 10% at admission and discharge, and about 20% at follow-up. There was also an increase in maximum pain ratings at follow-up compared with pain levels both at admission (P<0.05) and discharge (P<0.001). A large proportion of the patients (68%) reported having pain at follow-up. Several of the mean scores on the SIP subscales (categories) were >20, indicating severe functional impairment. These were work (42.7, s.d. 30.6), recreation and pastimes (26.3, s.d. 20), home management (21.2, s.d. 20.9) and sleep and rest (22.1, s.d. 21.4).
Correlation analyses
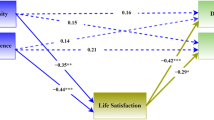
With one exception, all correlations between personality measures (that is, LOT-R, PANAS-PA and PANAS-NA) obtained at admission and the SIP scales were significant (Table 2). Furthermore, pain ratings obtained in the three phases of the study were consistently related to both psychosocial and physical aspects of functional health. Generally, measures of emotional distress (that is, HADS-A, HADS-D and IES-R) were positively correlated with the SIP scales. Further analyses showed significant correlations between pain and HADS-A at admission (r=0.35, P<0.01). At discharge and follow-up both HADS-A and HADS-D were significantly associated with pain ratings (coefficients in the 0.24–0.39 range, P<0.05). These coefficients were still significant after controlling for personality variables (that is, LOT-R, PANAS-PA and PANAS-NA) in partial correlation analyses (data not shown).
Regression analyses
As is evident from Table 3, all the SIP scales were significantly predicted by the LOT-R.
Nearly one-fifth of the variance in the SIP total score could be accounted for by this independent variable. Moreover, inclusion of the pain variable, and in model 3 the HADS-D, resulted in an additional increase in R2, and together these independent variables accounted for 25–39% of the variance in the SIP total score. Generally, rather similar effects of the LOT-R and the pain variables on the individual SIP scales were found.
Discussion
The primary purpose of the study was to investigate predictors of long-term functional health status in a group of MT and/or SCI patients. The impact of major trauma was reflected in the elevated mean scores on several of the SIP scales, indicating that a high proportion of the patients experienced persistent consequences of their injuries. Moreover, several of the patients evidenced symptoms of anxiety and/or depression, particularly at follow-up. Although most of the psychological measures correlated significantly with the SIP scales, dispositional optimism turned out to be the most robust predictor variable. With the exception of HADS depression scores at follow-up, inclusion of emotional distress indices did not result in significant increases in R2 when these variables were entered after dispositional optimism and pain ratings in hierarchical regressions. It should be mentioned, however, that part of the associations found might be attributed to overlap between measurements. Of particular note, anxiety and mood problems are addressed not only in the HADS but also in the SIP psychosocial and total scores. Consequently, empirical associations between these two measures should be expected.
Dispositional optimism is a widely studied trait in psychology and medicine associated with a variety of important outcomes.17, 18 For example, low optimism scores have been shown to predict progression of carotid atherosclerosis, and delay in returning to normal activities following hernia operations. Moreover, evidence supports better adjustment following surgery and radiation therapy for cancer among optimists.17, 18 The originators of the LOT scales suggest that the better emotional and behavioral outcomes of optimists may be fostered partly by their use of well-functioning coping styles, such as their ability to recruit social support networks and their use of problem-focused and preventive coping strategies.18 Generally, dispositional optimism appears as a crucial personality trait for the understanding of coping and self-regulation processes in individuals who have suffered serious trauma, or stress experiences generally. Interestingly, research has suggested that the trait may be based on previously learned experiences and is therefore, to a certain extent, amenable to change.17, 18
Another contribution of this study was to provide comprehensive analyses of the association between pain experiences, functional health and emotional distress. Importantly, maximum pain ratings emerged as significant predictors of both physical and psychosocial aspects of functional health. The results also showed that pain was related to depression and/or anxiety in all phases of this study. Accumulated research has shown that chronic pain is strongly associated with risk of depression and anxiety, with relative risks ranging from 2 to 4 in most studies.19 Evidence that pain causes emotional distress, rather than vice versa, comes from treatment studies indicating that levels of depression and anxiety normalize after successful pain treatment.20 On the other hand, psychological factors are predictive of the development of chronic pain after injury/disease, and there is evidence that anxiety and depression increase pain sensitivity and may therefore exacerbate pain conditions.19, 20
A potential limitation of this study is the relatively small sample size, combined with what seems to be nonrandom attrition from admission to follow-up (that is, the nonresponders having shorter stay in the rehabilitation hospital, being less optimistic and having lower trait PA). Thus, caution must be taken in generalizing the results. Still, the main findings, in terms of relationships between the SIP scales and the independent variables, some of which are measured at several time points, appear quite consistent.
Conclusion
Despite their limitations, our results may have important implications. Notably, we found that both dispositional optimism and pain predicted functional health status assessed several years after severe physical injury. Furthermore, in each phase of this study significant associations between pain and emotional distress indices were found, indicating that these variables may be causally related, independent of personality influences. In the follow-up phase, depression emerged as an independent predictor of functional health status. Taken together, these findings suggest that the combination of pain with depression/anxiety and low optimism could represent a high-risk group for disability and reduced quality of life, in which case this may be a patient group of particular importance for targeted interventions.
References
Gyatt GH, Naylor CD, Juniper E, Heyland DK, Jaeschke R, Cook DJ . User's guides to the medical literature. XII. How to use articles about health-related quality of life. JAMA 1997; 277: 1232–1237.
Holtslag HR, Post MW, Lindeman E, Van der Werken C . Long-term functional health status of severely injured patients. Injury 2007; 38: 280–289.
Abrantes-Pais FN, Friedman JK, Lovallo WR, Ross ED . Psychological or physiological: why are tetraplegic patients content? Neurology 2007; 69: 261–267.
Quale AJ, Schanke AK, Froslie KF, Roise O . Severity of injury does not have any impact on posttraumatic stress symptoms in severely injured patients. Injury 2009; 40: 498–505.
Noreau L, Shephard R . Spinal cord injury, exercise and quality of life. Spinal Cord 1998; 36: 716–723.
Post M, Ros W, Schrijvers A . Impact of social support on health status and life satisfaction in people with a spinal cord injury. Psychol Health 1999; 14: 679–695.
Post M, Noreau L . Quality of life after spinal cord injury. J Neurol Phys Ther 2005; 29: 139–146.
Quale AJ, Schanke AK . Resilience in the face of coping with a severe physical injury: a study of trajectories of adjustment in a rehabilitation setting. Rehabil Psychol 2010; 55: 12–22.
Association for the Advancement of Automotive Medicine. The Abbreviated Injury Scale 1990 Revision Update 98. Association for the Advancement of Automotive Medicine: Des Plaines, IL, 1998.
Bergner M, Bobbitt RA, Pollard WE, Martin DP, Gilson BS . The sickness impact profile: validation of a health status measure. Med Care 1976; 14: 57–67.
Gjertsen E . Sickness impact profile (Norwegian version). Tidsskr Nor Laegeforen (Journal of the Norwegian Medical Association) 1985; 105: 2152–2157.
de Bruin AF, de Witte LP, Stevens F, Diederiks JP . Sickness impact profile: the state of the art of a generic functional status measure. Soc Sci Med 1992; 35: 1003–1014.
Weiss DS, Marmar CR . The impact of event scale - revised. In: Wilson JP, Keane TM (eds). Assessing Psychological Trauma and PTSD: A Handbook for Practitioners. Guilford Press: New York, 1997, pp 399–411.
Zigmond AS, Snaith RP . The hospital anxiety and depression scale. Acta Psychiatr Scand 1983; 67: 361–370.
Watson D, Clark LA, Tellegen A . Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol 1988; 54: 1063–1070.
Scheier MF, Carver CS, Bridges MW . Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. J Pers Soc Psychol 1994; 67: 1063–1078.
Vassar M, Bradley G . A reliability generalization of coefficient Alpha for the Life Orientation Test. J Pers Assess 2010; 92: 362–370.
Carver CS, Scheier MF, Miller CJ, Fulford D . Optimism. In: Lopez SJ, Snyder CR (eds). Oxford Handbook of Positive Psychology, 2nd edn. Oxford University Press: New York, 2009, pp 303–312.
Kroenke K, Shen J, Oxman TE, Williams JW, Dietrich AJ . Impact of pain on the outcomes of depression treatment: results from the RESPECT trial. Pain 2008; 134: 209–215.
Von Korff M, Simon G . The relationship between pain and depression. Br J Psychiat 1996; 168(Suppl): 101–108.
Acknowledgements
This research was supported by grants from the Norwegian Foundation for Health and Rehabilitation through the Norwegian Association of Disabled.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Vassend, O., Quale, A., Røise, O. et al. Predicting the long-term impact of acquired severe injuries on functional health status: the role of optimism, emotional distress and pain. Spinal Cord 49, 1193–1197 (2011). https://doi.org/10.1038/sc.2011.70
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2011.70
Keywords
This article is cited by
-
Discharge from the trauma centre: exposure to opioids, unmet information needs and lack of follow up—a qualitative study among physical trauma survivors
Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine (2021)
-
Psychosocial resources and chronic pain in individuals with spinal cord injury: evidence from the second Swiss national community survey
Spinal Cord (2021)
-
The relationship between traits optimism and anxiety and health-related quality of life in patients hospitalized for chronic diseases: data from the SATISQOL study
Health and Quality of Life Outcomes (2013)
-
Disposition and Adjustment to Chronic Pain
Current Pain and Headache Reports (2013)