Abstract
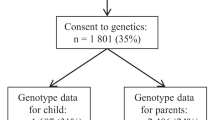
Early childhood obesity is a growing global concern; however, the role of common genetic variation on infant and child weight development is unclear. Here, we identify 46 loci associated with early childhood body mass index at specific ages, matching different child growth phases, and representing four major trajectory patterns. We perform genome-wide association studies across 12 time points from birth to 8 years in 28,681 children and their parents (27,088 mothers and 26,239 fathers) in the Norwegian Mother, Father and Child Cohort Study. Monogenic obesity genes are overrepresented near identified loci, and several complex association signals near LEPR, GLP1R, PCSK1 and KLF14 point towards a major influence for common variation affecting the leptin–melanocortin system in early life, providing a link to putative treatment strategies. We also demonstrate how different polygenic risk scores transition from birth to adult profiles through early child growth. In conclusion, our results offer a fine-grained characterization of a changing genetic landscape sustaining early childhood growth.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The full GWAS summary statistics for all time points are available at https://www.fhi.no/en/studies/moba/for-forskere-artikler/gwas-data-from-moba/. Access to genotypes and phenotypes from MoBa is subject to controlled access by the Norwegian Institute of Public Health in accordance with national and international regulations. Conditions of access including contact details for requests can be found at the Norwegian Institute of Public Health website (https://www.fhi.no/en/studies/moba/).
HRC or 1000G Imputation preparation and checking: https://www.well.ox.ac.uk/~wrayner/tools/.
Sanger imputation service: https://imputation.sanger.ac.uk/.
LD score repository: https://alkesgroup.broadinstitute.org/LDSCORE/.
Genotype-Tissue Expression: https://www.gtexportal.org/.
Birth weight reference data29: http://egg-consortium.org/BW5/Fetal_BW_European_meta.NG2019.txt.gz.
Adult BMI reference data15: http://portals.broadinstitute.org/collaboration/giant/images/c/c8/Meta-analysis_Locke_et_al%2BUKBiobank_2018_UPDATED.txt.gz.
T2D67: https://www.diagram-consortium.org/downloads.html.
• T2D GWAS meta-analysis–unadjusted for BMI67.
• T2D GWAS meta-analysis–adjusted for BMI67.
Childhood obesity18: http://egg-consortium.org/Childhood_Obesity_2019/CHILDHOOD_OBESITY.TRANS_ANCESTRAL.RESULTS.txt.gz.
Childhood BMI16: http://egg-consortium.org/Childhood_BMI/EGG_BMI_HapMap_DISCOVERY.txt.gz.
ALSPAC data dictionary and variable search tool: http://www.bristol.ac.uk/alspac/researchers/our-data/.
Change history
09 February 2024
A Correction to this paper has been published: https://doi.org/10.1038/s42255-024-01004-z
References
Fraser, A. et al. Cohort Profile: the Avon Longitudinal Study of Parents and Children: ALSPAC mothers cohort. Int. J. Epidemiol. 42, 97–110 (2013).
Rolland-Cachera, M. F., Deheeger, M., Maillot, M. & Bellisle, F. Early adiposity rebound: causes and consequences for obesity in children and adults. Int. J. Obes. 30, S11–S17 (2006).
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2,416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 390, 2627–2642 (2017).
World Health Organization. Consideration of the evidence on childhood obesity for the Commission on Ending Childhood Obesity: report of the ad hoc working group on science and evidence for ending childhood obesity (WHO, Geneva, 2016) http://apps.who.int/iris/bitstream/10665/206549/1/9789241565332_eng.pdf?ua=1
Singh, A. S., Mulder, C., Twisk, J. W. R., van Mechelen, W. & Chinapaw, M. J. M. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes. Rev. 9, 474–488 (2008).
Woo, J. G. et al. Prediction of adult class II/III obesity from childhood BMI: the i3C consortium. Int. J. Obes. 44, 1164–1172 (2020).
Geserick, M. et al. Acceleration of BMI in early childhood and risk of sustained obesity. N. Engl. J. Med. 379, 1303–1312 (2018).
MacLean, P. S., Higgins, J. A., Giles, E. D., Sherk, V. D. & Jackman, M. R. The role for adipose tissue in weight regain after weight loss. Obes. Rev. 16, 45–54 (2015).
Silventoinen, K. et al. Genetic and environmental effects on body mass index from infancy to the onset of adulthood: an individual-based pooled analysis of 45 twin cohorts participating in the COllaborative project of Development of Anthropometrical measures in Twins (CODATwins) study. Am. J. Clin. Nutr. 104, 371–379 (2016).
Silventoinen, K. et al. Differences in genetic and environmental variation in adult BMI by sex, age, time period, and region: an individual-based pooled analysis of 40 twin cohorts. Am. J. Clin. Nutr. 106, 457–466 (2017).
Kilpeläinen, T. O. et al. Physical activity attenuates the influence of FTO variants on obesity risk: a meta-analysis of 218,166 adults and 19,268 children. PLoS Med. 8, e1001116 (2011).
Khera, A. V. et al. Polygenic prediction of weight and obesity trajectories from birth to adulthood. Cell 177, 587–596 (2019).
Yang, J. et al. Genetic variance estimation with imputed variants finds negligible missing heritability for human height and body mass index. Nat. Genet. 47, 1114–1120 (2015).
Yang, J. et al. Genome partitioning of genetic variation for complex traits using common SNPs. Nat. Genet. 43, 519–525 (2011).
Yengo, L. et al. Meta-analysis of genome-wide association studies for height and body mass index in ∼700,000 individuals of European ancestry. Hum. Mol. Genet. 27, 3641–3649 (2018).
Felix, J. F. et al. Genome-wide association analysis identifies three new susceptibility loci for childhood body mass index. Hum. Mol. Genet. 25, 389–403 (2016).
Vogelezang, S. et al. Novel loci for childhood body mass index and shared heritability with adult cardiometabolic traits. PLoS Genet. 16, e1008718 (2020).
Bradfield, J. P. et al. A trans-ancestral meta-analysis of genome-wide association studies reveals loci associated with childhood obesity. Hum. Mol. Genet. 28, 3327–3338 (2019).
Helgeland, Ø. et al. Genome-wide association study reveals dynamic role of genetic variation in infant and early childhood growth. Nat. Commun. 10, 4448 (2019).
Alves, A. C. et al. GWAS on longitudinal growth traits reveals different genetic factors influencing infant, child, and adult BMI. Sci. Adv. 5, eaaw3095 (2019).
Farooqi, I. S. et al. Effects of recombinant leptin therapy in a child with congenital leptin deficiency. N. Engl. J. Med. 341, 879–884 (1999).
Licinio, J. et al. Phenotypic effects of leptin replacement on morbid obesity, diabetes mellitus, hypogonadism, and behavior in leptin-deficient adults. Proc. Natl Acad. Sci. USA 101, 4531–4536 (2004).
Turcot, V. et al. Protein-altering variants associated with body mass index implicate pathways that control energy intake and expenditure in obesity. Nat. Genet. 50, 26–41 (2018).
Loos, R. J. F. & Yeo, G. S. H. The genetics of obesity: from discovery to biology. Nat. Rev. Genet. https://doi.org/10.1038/s41576-021-00414-z (2021).
Flannick, J., Johansson, S. & Njølstad, P. R. Common and rare forms of diabetes mellitus: towards a continuum of diabetes subtypes. Nat. Rev. Endocrinol. 12, 394–406 (2016).
Marenne, G. et al. Exome sequencing identifies genes and gene sets contributing to severe childhood obesity, linking PHIP variants to repressed POMC transcription. Cell Metab. 31, 1107–1119 (2020).
Magnus, P. et al. Cohort Profile Update: The Norwegian Mother and Child Cohort Study (MoBa). Int. J. Epidemiol. 45, 382–388 (2016).
Yang, J. et al. Conditional and joint multiple-SNP analysis of GWAS summary statistics identifies additional variants influencing complex traits. Nat. Genet. 44, 369–375 (2012).
Warrington, N. M. et al. Maternal and fetal genetic effects on birth weight and their relevance to cardio-metabolic risk factors. Nat. Genet. https://doi.org/10.1038/s41588-019-0403-1 (2019).
Boyd, A. et al. Cohort Profile: the ‘children of the 90s’—the index offspring of the Avon Longitudinal Study of Parents and Children. Int. J. Epidemiol. 42, 111–127 (2013).
Sun, Q. et al. Genome-wide association study identifies polymorphisms in LEPR as determinants of plasma soluble leptin receptor levels. Hum. Mol. Genet. 19, 1846–1855 (2010).
Saeed, S. et al. Loss-of-function mutations in ADCY3 cause monogenic severe obesity. Nat. Genet. 50, 175–179 (2018).
Stergiakouli, E. et al. Genome-wide association study of height-adjusted BMI in childhood identifies functional variant in ADCY3. Obesity 22, 2252–2259 (2014).
Krashes, M. J., Lowell, B. B. & Garfield, A. S. Melanocortin-4 receptor-regulated energy homeostasis. Nat. Neurosci. 19, 206–219 (2016).
Jackson, R. S. et al. Obesity and impaired prohormone processing associated with mutations in the human prohormone convertase 1 gene. Nat. Genet. 16, 303–306 (1997).
Martín, M. G. et al. Congenital proprotein convertase 1/3 deficiency causes malabsorptive diarrhea and other endocrinopathies in a pediatric cohort. Gastroenterology 145, 138–148 (2013).
Ramos-Molina, B., Martin, M. G. & Lindberg, I. PCSK1 variants and human obesity. Prog. Mol. Biol. Transl. Sci. 140, 47–74 (2016).
Sun, B. B. et al. Genomic atlas of the human plasma proteome. Nature 558, 73–79 (2018).
Alvarez, E. et al. The expression of GLP-1 receptor mRNA and protein allows the effect of GLP-1 on glucose metabolism in the human hypothalamus and brainstem. J. Neurochem. 92, 798–806 (2005).
Yau, A. M. W. et al. A pilot study investigating the influence of glucagon-like peptide-1 receptor single-nucleotide polymorphisms on gastric emptying rate in Caucasian men. Front. Physiol. 9, 1331 (2018).
Small, K. S. et al. Regulatory variants at KLF14 influence type 2 diabetes risk via a female-specific effect on adipocyte size and body composition. Nat. Genet. 50, 572–580 (2018).
Kong, A. et al. Parental origin of sequence variants associated with complex diseases. Nature 462, 868–874 (2009).
Yang, Q. & Civelek, M. Transcription factor KLF14 and metabolic syndrome. Front. Cardiovasc. Med. 7, 91 (2020).
Yaghootkar, H. et al. Genetic studies of leptin concentrations implicate leptin in the regulation of early adiposity. Diabetes https://doi.org/10.2337/db20-0070 (2020).
Murray, P. G. & Clayton, P. E. Endocrine control of growth. Am. J. Med. Genet. C Semin. Med. Genet. 163C, 76–85 (2013).
Yeo, G. S. H. et al. The melanocortin pathway and energy homeostasis: from discovery to obesity therapy. Mol. Metab. 48, 101206 (2021).
Clément, K. et al. Efficacy and safety of setmelanotide, an MC4R agonist, in individuals with severe obesity due to LEPR or POMC deficiency: single-arm, open-label, multicentre, phase 3 trials. Lancet. Diabetes Endocrinol. 8, 960–970 (2020).
Clément, K. et al. MC4R agonism promotes durable weight loss in patients with leptin receptor deficiency. Nat. Med. 24, 551–555 (2018).
González-García, I., Milbank, E., Diéguez, C., López, M. & Contreras, C. Glucagon, GLP-1 and thermogenesis. Int. J. Mol. Sci. 20, 3445 (2019).
Kelly, A. S. et al. A randomized, controlled trial of liraglutide for adolescents with obesity. N. Engl. J. Med. 382, 2117–2128 (2020).
Farr, O. M. et al. GLP-1 receptors exist in the parietal cortex, hypothalamus and medulla of human brains and the GLP-1 analogue liraglutide alters brain activity related to highly desirable food cues in individuals with diabetes: a crossover, randomised, placebo-controlled trial. Diabetologia 59, 954–965 (2016).
Beiroa, D. et al. GLP-1 agonism stimulates brown adipose tissue thermogenesis and browning through hypothalamic AMPK. Diabetes 63, 3346–3358 (2014).
Sisley, S. et al. Neuronal GLP1R mediates liraglutide’s anorectic but not glucose-lowering effect. J. Clin. Invest. 124, 2456–2463 (2014).
Vendrell, J. et al. Study of the potential association of adipose tissue GLP-1 receptor with obesity and insulin resistance. Endocrinology 152, 4072–4079 (2011).
Delaneau, O., Zagury, J.-F. & Marchini, J. Improved whole-chromosome phasing for disease and population genetic studies. Nat. Methods 10, 5–6 (2013).
Durbin, R. Efficient haplotype matching and storage using the positional Burrows–Wheeler transform. Bioinformatics 30, 1266–1272 (2014).
Marees, A. T. et al. A tutorial on conducting genome-wide association studies: quality control and statistical analysis. Int. J. Methods Psychiatr. Res. 27, e1608 (2018).
Loh, P.-R. et al. Efficient Bayesian mixed-model analysis increases association power in large cohorts. Nat. Genet. 47, 284–290 (2015).
1000 Genomes Project Consortium et al. An integrated map of genetic variation from 1,092 human genomes. Nature 491, 56–65 (2012).
McLaren, W. et al. The Ensembl variant effect predictor. Genome Biol. 17, 122 (2016).
Jassal, B. et al. The reactome pathway knowledgebase. Nucleic Acids Res. 48, D498–D503 (2020).
Sánchez, L. F. H. et al. PathwayMatcher: proteoform-centric network construction enables fine-granularity multiomics pathway mapping. Gigascience 8, giz088 (2019).
Staley, J. R. et al. PhenoScanner: a database of human genotype–phenotype associations. Bioinformatics 32, 3207–3209 (2016).
Kamat, M. A. et al. PhenoScanner V2: an expanded tool for searching human genotype–phenotype associations. Bioinformatics 35, 4851–4853 (2019).
Chen, J. et al. Dissecting maternal and fetal genetic effects underlying the associations between maternal phenotypes, birth outcomes, and adult phenotypes: a Mendelian-randomization and haplotype-based genetic score analysis in 10,734 mother–infant pairs. PLoS Med. 25, 17 (2020).
Wand, H. et al. Improving reporting standards for polygenic scores in risk prediction studies. Nature 591, 211–219 (2021).
Mahajan, A. et al. Fine-mapping type 2 diabetes loci to single-variant resolution using high-density imputation and islet-specific epigenome maps. Nat. Genet. 50, 1505–1513 (2018).
Acknowledgements
This work was supported by grants (to S.J.) from Helse Vest’s Open Research (nos. 912250 and F-12144), the Novo Nordisk Foundation (NNF19OC0057445) and the Research Council of Norway (no. 315599)); and (to P.R.N.) from the European Research Council (AdG SELECTionPREDISPOSED no. 293574), the Bergen Research Foundation (Utilizing the Mother and Child Cohort and the Medical Birth Registry for Better Health), Stiftelsen Kristian Gerhard Jebsen (Translational Medical Center), the University of Bergen, the Research Council of Norway (FRIPRO no. 240413), the Western Norway Regional Health Authority (Strategic Fund Personalized Medicine for Children and Adults), the Novo Nordisk Foundation (no. 54741) and the Norwegian Diabetes Association. This work was partly supported by the Research Council of Norway through its Centres of Excellence funding scheme (nos. 262700 and 223273), Better Health by Harvesting Biobanks (no. 229624) and The Swedish Research Council, Stockholm, Sweden (2015-02559), the Research Council of Norway (FRIMEDBIO nos. 547711 and 273291) and March of Dimes (no. 21-FY16-121). MoBa is supported by the Norwegian Ministry of Health and Care Services and the Ministry of Education and Research, National Institutes of Health (NIH)/NIEHS (contract no. N01-ES-75558), NIH/NINDS (grant nos. UO1 NS 047537-01 and UO1 NS 047537-06A1).
We are grateful to all the families in Norway who are taking part in the ongoing MoBa cohort study.
We are extremely grateful to all the families who took part in the ALSPAC cohort study, the midwives for their help in recruiting them, and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists and nurses. The UK Medical Research Council (MRC) and Wellcome (grant ref. 217065/Z/19/Z) and the University of Bristol provide core support for ALSPAC. This publication is the work of the authors and S.J and M.V. serve as guarantors for the contents of this paper. A comprehensive list of grant funding is available on the ALSPAC website (http://www.bristol.ac.uk/alspac/external/documents/grant-acknowledgements.pdf); this research was specifically funded by Wellcome Trust and the MRC (core; 076467/Z/05/Z). ALSPAC GWAS data were generated by sample logistics and genotyping facilities at Wellcome Sanger Institute and LabCorp (Laboratory Corporation of America) using support from 23andMe.
All analyses were performed using digital laboratories in HUNT Cloud at the Norwegian University of Science and Technology, Trondheim, Norway. We are grateful for outstanding support from the HUNT Cloud community.
Author information
Authors and Affiliations
Contributions
Ø.H., M.V., P.R.N. and S.J. designed the study. Ø.H. and M.V. analysed the data. Ø.H., M.V. and S.J. interpreted the data. J.J., J.B., G.P.K., T.R.K., P.M., C.S. and O.A.A. contributed to sample acquisition and genotyping. J.J. and J.B. assisted with genotype QC. P.S.-N., C.F., I.L.K., B.B.J., B.J. and P.R.N. critically revised the manuscript for important intellectual content. Ø.H., M.V. and S.J. wrote the manuscript. All authors participated in preparing the manuscript by reading and commenting on drafts before submission. P.R.N. and S.J. acquired the funding.
Corresponding authors
Ethics declarations
Competing interests
O.A.A. is a consultant to HealthLytix. The other authors declare no competing interests.
Peer review
Peer review information
Nature Metabolism thanks Timothy Frayling and the other, anonymous, reviewers for their contribution to the peer review of this work. Primary Handling Editor: Isabella Samuelson, in collaboration with the Nature Metabolism team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Overlay with association profiles obtained from ALSPAC.
Effect size estimates for all 46 hits obtained in the MoBa and ALSPAC cohorts. The quadrant plots to the left display the shape of the effect size estimate over time as obtained in Fig. 1B, for both cohorts, between birth and eight years of age. The effect size estimates are plotted at each age to the right using line and ribbons for MoBa and point and error bars for ALSPAC. Note that to maintain readability of earlier time points, the scale of the x axis is not linear. Thick and thin error bars/ribbons represent one standard error estimate on each side of the effect size estimates and 95% confidence intervals, respectively. See Supplementary Table 1 for the number of samples at each time point.
Extended Data Fig. 2 SNP-based heritability.
H2 estimates from LD score regression for BMI plotted at each time point (black) along with locally estimated scatterplot smoothing (LOESS) local regression (in blue). Error bars represent ±SEM. See Supplementary Table 1 for the number of samples at each time point.
Extended Data Fig. 3 LD-score regression.
Genetic correlation estimate, rg, of selected traits with early growth BMI at birth, 6 weeks, 3, 6, 8 months, and 1, 1.5, 2, 3, 5, 7, and 8 years of age. Ribbons represent one standard error estimate on each side of the rg estimate. See methods for details and Supplementary Table 7 for correlation with other traits. See Supplementary Table 1 for the number of samples at each time point.
Extended Data Fig. 4 Comparison with previous studies on birth weight and adult BMI for the variants near monogenic obesity genes.
Heatmap of the effect size for the none top hits near monogenic diabetes genes (see Supplementary Table 2) from birth to adulthood obtained similarly as for Fig. 2A. Note that, in contrast to Fig. 2A, the name of the nearest monogenic obesity gene is used on the y axis, and not the locus name. See Supplementary Table 1 for the number of samples at each time point.
Extended Data Fig. 5 Loci with multiple independent associations signals.
Effect size estimates with child BMI from birth to eight years of age for the lead SNPs of the signals near (A) LEPR, (B) GLP1R, and (C) PCSK1. Dark and light Ribbons represent one standard error estimate on each side of the effect size estimate and 95% confidence intervals, respectively. For each SNP, regional plots are displayed at the age at peak association, highlighting the lead SNPs with red diamonds and SNPs coloured according to the LD R2, with the exons of the gene according to Ensembl at the bottom and recombination rates in blue. See Supplementary Table 1 for the number of samples at each time point, the methods for the statistical analysis.
Extended Data Fig. 6 Polygenic risk score (PRS) analyses.
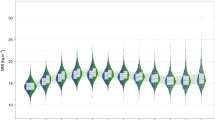
A-D) Mean standardized BMI of children in this study at each time point after stratification in PRS deciles using PRS trained using summary statistics from meta-analyses (bottom), and share of obese children at a given time point in the top PRS decile (top), where obesity is defined as belonging to the top 5 BMI percentile. PRS training was performed using summary statistics for (A) birth weight from Warrington et al29. (B) childhood obesity from Bradfield et al18. (C) childhood BMI from Felix et al16. (D) adult BMI from Yengo et al15. (E) Mean standardized BMI for the children in this study falling in the top and bottom deciles of type 2 Diabetes (T2D) risk scores at each time point. PRS for T2D and T2D adjusted for BMI, represented in dashed and solid lines, respectively, were trained using summary statistics from Mahajan et al67. (F) R2 estimated at each time point when training the PRS for Birth weight, childhood obesity, childhood BMI, adult BMI, and T2D in Fig. 5A-E. (G) Mean standardized BMI of children in MoBa that were kept out of the discovery sample falling in the top and bottom quintiles of time-resolved early growth PRSs trained using summary statistics of this study at each time point (solid lines) and of the adult BMI PRS of Fig. 1D (dashed line) (Bottom), along with the respective R2 estimated when training the PRSs (Top). (H) Mean standardized BMI of children in MoBa that were kept out of the discovery sample falling in the bottom, intermediate, and top quintiles of time-resolved early growth PRSs trained using summary statistics of this study at each time point, in blue, black, and red, respectively. At each time point, rectangles represent one standard error estimate on each side of the mean estimate. Transitions between time points represent the share of children moving from one quintile category to the other. For each time point, mean BMI estimates for these children after stratification in quintiles are plotted for time-resolved early growth PRSs against the adult BMI PRS of Fig. 1D in inserts. All error bars/ribbons represent one standard error estimate on each side of the mean estimate. See Supplementary Table 1 for the number of samples at each time point.
Extended Data Fig. 7 Growth curves processing.
Length and Weight curves were inspected for outliers and missing values were imputed. This process was repeated until no value was changed. Then length values were inspected for negative growth and adjusted. The entire process was repeated until no value was changed.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Helgeland, Ø., Vaudel, M., Sole-Navais, P. et al. Characterization of the genetic architecture of infant and early childhood body mass index. Nat Metab 4, 344–358 (2022). https://doi.org/10.1038/s42255-022-00549-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s42255-022-00549-1
This article is cited by
-
Smoking during pregnancy and its effect on placental weight: a Mendelian randomization study
BMC Pregnancy and Childbirth (2024)
-
Early-childhood body mass index and its association with the COVID-19 pandemic, containment measures and islet autoimmunity in children with increased risk for type 1 diabetes
Diabetologia (2024)
-
A genome-wide association study provides insights into the genetic etiology of 57 essential and non-essential trace elements in humans
Communications Biology (2024)
-
Novel genetic association between obesity, colorectal cancer, and inflammatory bowel disease
Journal of Diabetes & Metabolic Disorders (2023)
-
Genome-wide association study of placental weight identifies distinct and shared genetic influences between placental and fetal growth
Nature Genetics (2023)