Abstract
This study aimed to ascertain the pooled prevalence and trend of consistent condom use in Sub-Saharan Africa, addressing the fragmented and inconsistent research on its role in preventing HIV transmission. In this meta-analysis, we systematically searched electronic databases such as PubMed, Embase, Scopus, Web of Science, Global Index Medicus, ScienceDirect, Africa-Wide Information (via EBSCOhost), as well as clinical trial registries, and the search engine Google Scholar. All necessary data were extracted using a standardized data extraction format. The data were analyzed using STATA 17 statistical software. Heterogeneity among the studies was assessed using the I2 test. A random-effect model was computed to estimate the pooled rate of consistent condom utilization. This meta-analysis, which included thirty-three full-text studies, found a pooled prevalence of 44.66% (95% CI 18.49–70.83; I2 = 0.00%) for consistent condom use in Sub-Saharan Africa. While the prevalence fluctuated between 2007 and 2022, the year-to-year variations were not statistically significant. The current study identified low rates of consistent condom use, with utilization fluctuating annually in the study area. Therefore, uncovering the underlying reasons and addressing barriers to consistent condom use is crucial in the region.
Similar content being viewed by others
Introduction
Great efforts have been made to end the Human Immunodeficiency Virus/Acquired Immunodeficiency Syndrome (HIV/AIDS) epidemic by 2030, yet it remains a global problem in post Millennium Development Goal (MDG) era. In 2022, approximately 39.0 million people were living with HIV globally. Among these, two-thirds (25.6 million) were in Africa1. Among the 39.0 million people living with HIV globally, 20.6 million were women, and 1.5 million were children. Additionally, 630,000 people died from AIDS-related illnesses in 20222.
Modeled estimates show that new infections declined from a peak of 3.4 million in 1996 to 1.8 million in 2017. However, this progress was slower than what was necessary to meet the 2020 milestone of fewer than 500,000 new infections3,4, indicating more effort is required.
Condoms are central to a combination HIV prevention approach and serve as cost-effective tools for preventing other sexually transmitted infections and unintended pregnancies5. Preventing unintended pregnancy among HIV-positive women constitutes a critical and cost-effective approach to the primary prevention of mother-to-child (PMTCT) of HIV. It is also a global public health priority to address the compromised state of maternal and child health in areas with high HIV prevalence6.
Despite a decrease in new HIV infections and AIDS-related deaths in recent years7, the international goal of reducing sexual transmission among youth and adults by 50% from 2010 to 2015 was not met8. This failure to achieve the target is associated with inconsistent condom use, attributed to limited knowledge about HIV and the belief that using condoms reduces sexual pleasure9.
Although consistent condom utilization (CCU) is vital for the prevention of HIV transmission, the studies conducted on this issue were fragmented and inconsistent in Sub-Saharan Africa (SSA). The prevalence of CCU ranges from 16.1%10 to 78.9%11 which showed a great variation across different geographical settings and different periods. Hence, evidence related to CCU should be identified by researchers to provide the leadership that will enable 90–90–90 to succeed in the globe in general and in SSA in particular. Therefore, the current study aimed to assess the pooled prevalence and trend of CCU among sexually active HIV positive individuals in SSA countries, 2023.
Methods
Protocol and registration
The findings presented in this review adhere to the guidelines outlined in the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) statement12 (Supplementary Table S1). The protocol for this review has been prospectively registered in the International Prospective Register of Systematic Reviews (PROSPERO), under the registration number CRD42022382283.
Search strategy and selection criteria
To gather relevant studies, we searched through various databases, including PubMed, Embase, Scopus, Web of Science, Global Index Medicus, ScienceDirect, Africa-Wide Information (via EBSCOhost), and clinical trial registries such as ClinicalTrials.gov and the International Clinical Trials Registry Platform (ICTRP). We also utilized Google Scholar and accessed the online libraries of Addis Ababa University and Bahir Dar University to further explore literature. Additionally, we manually reviewed the reference lists of included articles to identify any additional relevant studies.
The core search terms and phrases included "prevalence," "consistent," "utilization," "condom," "HIV," "positive," "person," "individual," and the names of sub-Saharan African countries. We used various techniques in our search strategies, such as truncation (*), Boolean operators (OR and AND), and phrase searching ("…"). Furthermore, we included MeSH terms in PubMed, Emtree terms in Embase, and synonyms to ensure comprehensive searches. The detailed search strategy is presented in Table (Supplementary Table S2).
Inclusion and exclusion criteria
Our study included all types of studies reported in the English language on the prevalence of consistent condom utilization, without restrictions on the study period. We considered articles available in our search sources from December 20, 2022, to January 30, 2023. We excluded articles without abstracts or full texts, anonymous reports, editorials, and qualitative studies.
Quality assessment and data abstraction procedure
The retrieved studies were imported into Endnote version 7, a reference manager software, to eliminate duplicate studies. Four authors (YW, TW, DE, and SB) independently reviewed and screened the titles and abstracts of the identified studies. Any disagreements that arose were resolved based on pre-established article selection criteria. To assess the quality of each study, we utilized The Newcastle–Ottawa Scale13, which was adapted for the systematic review to evaluate cross-sectional studies14. The assessment tool consists of three domains: selection, comparability, and outcome, each encompassing specific items detailed in the supplementary file (Supplementary Table S3). Each original study underwent independent evaluation by the four authors using this tool. In case of disagreements among the authors, a consensus was reached by averaging the scores provided by the four authors. The inter-rater agreement was calculated using a Fleiss kappa statistic that yielded a value of 0.226 (95% CI 0.222–0.231, p value < 0.001), indicating a fair level of agreement (Supplementary Table S4).
Outcome measurement
Consistent condom utilization is the percentage of respondents who used a condom every time they had sex with any non-spouse or non-cohabiting partner over time15. The prevalence was determined by dividing the total number of HIV-positive individuals who consistently used condoms by the total number of HIV-positive individuals included in the study, then multiplying by 100.
Data extraction and analysis
For data extraction, a standardized format adapted from the data extraction format of the Joanna Briggs Institute (JBI)16 was utilized. Four authors independently extracted the necessary data using this format. In case of any discrepancies during the data extraction process, they were resolved through discussion and consensus. The data extraction format consisted of the primary author’s name, publication year, study site, study design, response rate, sample size, participant gender, and prevalence of consistent condom use with a 95% confidence interval (CI).
STATA version 17 statistical software was used for meta-analysis. Pooled analysis was conducted using a random-effects model17. The level of heterogeneity among the studies was assessed using the I-squared statistic, with values of 25%, 50%, and 75% indicating low, moderate, and high heterogeneity, respectively17,18. However, in this analysis, there was no heterogeneity between studies (I2 = 0.00%). Sub-group analysis was done based on study region, design, and participants’ gender. To examine publication bias, we utilized funnel plots and performed Begg's and Egger's regression tests19 for a more objective assessment. Trim and fill analyses were also performed. Furthermore, sensitivity analysis was employed to assess the influence of individual studies on the overall estimation.
Results
Search results
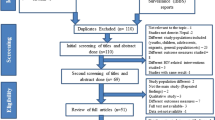
The initial search yielded 4,623 articles from various sources. After removing duplicates, 2402 unique articles were identified. Among these, 2,286 irrelevant records were excluded, leaving 116 articles for further review. Out of these, 61 articles were excluded after reviewing their titles and abstracts due to lack of relevance. Subsequently, 55 full-text articles were thoroughly assessed based on the inclusion criteria10,11,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72. Finally, a total of 33 studies10,11,20,21,22,24,25,26,27,29,32,34,36,38,45,46,47,48,49,50,51,52,53,54,55,65,66,67,68,69,70,71,72 meeting the inclusion criteria were included in the meta-analysis (Fig. 1).
Characteristics of reviewed studies
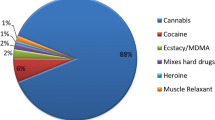
This review included thirty-three studies published between 2007 and 2022, with a cumulative sample size of 11,499. The majority of the included studies originated from Ethiopia (eleven) and Nigeria (ten). Thirty-one studies employed a cross-sectional study design, while two utilized a cohort study design (Table 1).
Meta-analysis
Risk bias Assessment
The studies included in this systematic review and meta-analysis had no considerable risk based on the Newcastle–Ottawa Scale quality appraisal criteria. Therefore, all the studies were considered in this review10,11,20,21,22,24,25,26,27,29,32,34,36,38,45,46,47,48,49,50,51,52,53,54,55,65,66,67,68,69,70,71,72 (Table 1).
Publication bias
A funnel plot indicated an asymmetrical distribution (Fig. 2), and Begg’s test yielded statistically significant results (p < 0.001). However, Egger’s test showed insignificant results for estimating the prevalence of CCU. To assess the impact of publication bias on the pooled analysis, trim fill analysis was conducted, and thirteen studies were filled. In this analysis, the pooled prevalence of CCU became 35.1% (CI 15.3%, 54.8%). Consequently, the confidence interval suggests no significant difference in the pooled prevalence of CCU (Fig. 3).
Sensitivity analysis
As shown in the figure, no individual study had an impact on the overall estimation of the result in the leave-one-out meta-analysis (Fig. 4).
Prevalence of consistent condom utilization
In this review, the prevalence of consistent condom utilization ranged from 16.1% to 78.9%10,11. Using the random effects meta-analysis model, the pooled prevalence of CCU was 42.52% (95% CI; 20.29, 64.74; I2 = 0.00%). The estimated overall prevalence of CCU is presented in a forest plot (Fig. 5).
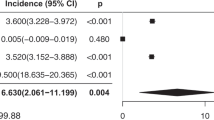
Subgroup analysis result of consistent condom use across sub-Sharan Africa
We have investigated whether study region, study design, sample size, publication year, and participants’ gender influence variability in the pooled estimation, utilizing a meta-regression model. However, none of these factors showed statistical significance (Supplementary Table S5). Subgroup analysis was done based on region, study design, and participants’ gender. This analysis revealed that consistent condom use was relatively higher in the Southern Africa region, among studies employing a cohort design, and in studies focusing exclusively on women (Fig. 6).
Trend of CCU
The prevalence of consistent condom use fluctuated between 2007 and 2022 (Fig. 7). However, our meta-regression analysis indicated that the year-to-year variability was not statistically significant (Supplementary Table S5).
Discussion
This systematic review and meta-analysis investigate consistent condom use among sexually active HIV-positive individuals in Sub-Saharan Africa. Globally, consistent condom use rates range from 4 to 52.4% among young, sexually active individuals73,74. In Sub-Saharan Africa, HIV transmission still constitutes a public health concern, with many adolescents and young adults engaging in unprotected sex and transactional sex73,75. This systematic review and meta-analysis finding also indicated that consistent condom utilization among sexually active HIV-positive individuals in SSA is low (42.5%). This finding is lower than a study conducted in the Asia–Pacific region (54–57%)44. Even if the response to HIV was started four decades before, CCU is low in SSA due to the existence of different harmful traditional practices such as age restrictions, gender norms, religious norms, stigma, and insufficient supply and, in some places, laws that make it an offense to carry condoms76,77. Many countries in Sub-Saharan countries also prohibit condom promotion and distribution in schools and other venues where adolescents socialize76. Hence, this brings a low level of consistent condom utilization in SSA countries as compared with Asian Pacific countries. In the current study, there is no substantial heterogeneity of consistent condom utilization across SSA.
The prevalence of consistent condom utilization was swinging up and down from 2007 to 2022. However, year-to-year variability was not statistically significant. Consistent condom utilization by HIV-positive individuals varies from year to year. This could be because, in recent years there is decrement in international funding for condom procurement in Sub-Saharan Africa. Moreover, domestic funding has not sufficiently increased its focus on the issue. Finally, this leads to stalled condom promotion and demand creation due to a lack of funding and decreased investment in several Sub-Saharan countries78.
Currently, the AIDS response and the broader global community have united around the goal of achieving 90–90–90 and ending the AIDS epidemic as a public health threat79. However, the low level of consistent condom utilization and its variability from year to year among HIV-positive individuals in Sub-Saharan countries will threaten the achievement of the 90–90–90 approach by 2030. Hence, focused efforts by health professionals should be given to developing skills that allow consistent condom utilization and overcome the specific obstacles that reduce the efficient and effective condom use in Sub-Saharan Africa's HIV-positive populations.
The low consistent condom utilization among sexually active HIV-positive individuals in Sub-Saharan Africa highlights an urgent need for targeted interventions to promote safer sexual practices and reduce HIV transmission rates within this vulnerable population.
Limitation
Limiting studies to publications in English may introduce bias to the overall findings in sub-Saharan Africa.
Conclusion
There is low consistent condom utilization among sexually active HIV-positive individuals in SSA. Additionally, consistent condom use has fluctuated over the years in the region. Therefore, it is crucial to investigate the underlying reasons and address the barriers. This endeavor can enhance HIV prevention efforts and, ultimately, improve public health outcomes.
Data availability
All data generated or analyzed during this study are included in the manuscript or supplementary information.
Abbreviations
- AIDS:
-
Acquired immuno-deficiency syndromes
- CI:
-
Confidence interval
- CCU:
-
Consistent condom utilization
- HIV:
-
Human immuno virus
- SSA:
-
Sub-Saharan Africa
- WHO:
-
World Health Organization
References
Organization WH. HIV and AIDS-Key Facts (World Health Organization, Geneva, 2023). https://www.who.int/news-room/fact-sheets/detail/hiv-aids
UNAIDS. Global HIV & AIDS Statistics—Fact Sheet (UNAIDS, 2023). https://www.unaids.org/en/resources/fact-sheet
HIV/AIDS JUNPo. UNAIDS Data 2017 (UNAIDS 2017, Geneva, Switzerland, 2018).
Organization, W. H. Global health sector strategy on HIV 2016–2021 (World Health Organization, Geneva, 2016).
Davis, L., Rountree, M. M. & Davis, J. A. Global cause awareness: Tracking awareness through electronic word of mouth. J. Nonprofit Public Sect. Mark. 28(3), 252–272 (2016).
Chersich, M. et al. Contraception coverage and methods used among women in South Africa: A national household survey. S. Afr. Med. J. 107(4), 307–314 (2017).
Organization WH. Enhanced Capacity Building Training for Frontline Staff on Building Trust and Communication: Facilitator’s Guide, July 2015 (World Health Organization, 2015).
Dehne, K. L. et al. HIV Prevention 2020: A framework for delivery and a call for action. Lancet HIV 3(7), e323–e332 (2016).
Crepaz, N. & Marks, G. Towards an understanding of sexual risk behavior in people living with HIV: A review of social, psychological, and medical findings. Aids 16(2), 135–149 (2002).
Conserve, D., Sevilla, L., Younge, S., Mbwambo, J. & King, G. Condom use among HIV-positive sexually active adults and partner’s HIV status in Dar es Salaam, Tanzania. J. Health Care Poor Underserv. 23(1), 191 (2012).
Shewamene, Z., Legesse, B., Tsega, B., Bhagavathula, A. S. & Endale, A. Consistent condom use in HIV/AIDS patients receiving antiretroviral therapy in northwestern Ethiopia: Implication to reduce transmission and multiple infections. HIV/AIDS (Auckland, NZ) 7, 119 (2015).
Liberati, A. et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions. BMJ 339 (2009).
Ioannidis, J. P. Interpretation of tests of heterogeneity and bias in meta-analysis. J. Eval. Clin. Pract. 14(5), 951–957 (2008).
Modesti, P. A. et al. Panethnic differences in blood pressure in Europe: A systematic review and meta-analysis. PloS One 11(1), e0147601 (2016).
Amon, J., et al. Behavioral Surveillance Surveys BSS. Guidelines for repeated behavioral surveys in populations at risk of HIV (2000).
Zeng, X. et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: A systematic review. J. Evid. Based Med. 8(1), 2–10 (2015).
Borenstein, M., Hedges, L. V., Higgins, J. P. & Rothstein, H. R. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res. Synth. Methods 1(2), 97–111 (2010).
Rücker, G., Schwarzer, G., Carpenter, J. R. & Schumacher, M. Undue reliance on I 2 in assessing heterogeneity may mislead. BMC Med. Res. Methodol. 8(1), 79 (2008).
Higgins, J. P. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 21(11), 1539–1558 (2002).
Haddad, L. B. et al. Factors associated with condom use among men and women living with HIV in Lilongwe, Malawi: A cross-sectional study. BMJ Sex Reprod. Health 44(1), 1–12 (2018).
Pilapil, M. et al. Retrospective analysis of the prevalence of and factors associated with condom use among young HIV-infected women in Cameroon. SAGE Open Med. 4, 2050312115626432 (2016).
Busari, O. A., et al. Consistent Condom Use and Its Associated Factors Among HIV Patients in a Tertiary Hospital in Southwest Nigeria.
Adetunji, J. & Meekers, D. Consistency in condom use in the context of HIV/AIDS in Zimbabwe. J. Biosoc. Sci. 33(1), 121–138 (2001).
Yalew, E., Zegeye, D. T. & Meseret, S. Patterns of condom use and associated factors among adult HIV positive clients in North Western Ethiopia: A comparative cross sectional study. BMC Public Health 12(1), 308 (2012).
Ezeala-Adikaibe, B., Okafor, I. & Umeh, M. Condom use among HIV-infected patients after initiation of highly active anti-retroviral therapy (HAART): A cross sectional hospital based survey. Int. J. Med. Health Dev. 22, 89–96 (2017).
Ayiga, N. Rates and predictors of consistent condom-use by people living with HIV/AIDS on antiretroviral treatment in Uganda. J. Health Popul. Nutr. 30(3), 270 (2012).
Salaudeen, A. G. et al. Condom use among people living with HIV/AIDS attending Abejukolo General Hospital in Kogi State, North Central Nigeria. Ann. Afr. Med. 13(3), 99–103 (2014).
Macharia, A., Kombe, Y., Mwaniki, P. & Habtu, M. Barriers of condom use among HIV positive women at Thika Level 5 Hospital, Kenya. J. AIDS Clin. Res. 8(8), 722 (2017).
Nduka, I., Enwereji, E. E., Nduka, E. C. & Ahuizi, E. R. Determinants of consistent condom use among Hiv-positive women in Abia State, South-east Nigeria. J. Clin. Res. HIV AIDS Prevent. 2(2), 1 (2014).
Fladseth, K., Gafos, M., Newell, M. L. & McGrath, N. The impact of gender norms on condom use among HIV-positive adults in KwaZulu-Natal, South Africa. PLoS One 10(4), e0122671 (2015).
Salaudeen, A. et al. Condom use among HIV sero-concordant couples attending a secondary health facility in North-Central Nigeria. Niger. J. Basic Clin. Sci. 10(2), 51 (2013).
Macharia, A. G., Kombe, Y. & Mwaniki, P. Consistent condom use among HIV positive women attending comprehensive care centre of thika level 5 hospital, Kenya (2015).
Alene, K. A. Consistent condom use among sexually active HIV positive women in Amhara region, Ethiopia. Open Access J. Contracept. 5, 85–90 (2014).
Ali, M. S., Tesfaye Tegegne, E., Kassa Tesemma, M. & Tesfaye Tegegne, K. Consistent condom use and associated factors among HIV-positive clients on antiretroviral therapy in North West Ethiopian Health Center, 2016 GC. In AIDS Research and Treatment 2019 (2019).
Bateganya, M. et al. Antiretroviral therapy and sexual behavior: A comparative study between antiretroviral-naive and-experienced patients at an urban HIV/AIDS care and research center in Kampala, Uganda. AIDS Patient Care STDs 19(11), 760–768 (2005).
Ayoola, O. D. et al. Pattern, challenges and correlates of condom use among Nigerians living with HIV infection. Asian Pac. J. Trop. Biomed. 4, S198–S203 (2014).
Adih, W. K. & Alexander, C. S. Determinants of condom use to prevent HIV infection among youth in Ghana. J. Adolesc. Health 24(1), 63–72 (1999).
Ezeanochie, M., Olagbuji, B., Ande, A. & Oboro, V. Fertility preferences, condom use, and concerns among HIV-positive women in serodiscordant relationships in the era of antiretroviral therapy. Int. J. Gynecol. Obstet. 107(2), 97–98 (2009).
Baiden, P. & Rajulton, F. Factors influencing condom use among women in Ghana: An HIV/AIDS perspective. SAHARA-J J. Soc. Asp. HIV/AIDS 8(2), 46–54 (2011).
Moazen, B. et al. Determinants of consistent condom use among iranians living with HIV/AIDS: Implication for prevention. Int. J. High Risk Behav. Addict. 6(4), 15 (2017).
Liu, H. et al. Effectiveness of ART and condom use for prevention of sexual HIV transmission in serodiscordant couples: A systematic review and meta-analysis. PLoS One 9(11), e111175 (2014).
Maharaj, P. & Cleland, J. Risk perception and condom use among married or cohabiting couples in KwaZulu-Natal, South Africa. Int. Fam. Plan. Perspect. 31, 24–29 (2005).
Lurie, M. et al. Sexual behavior and reproductive health among HIV-infected patients in urban and rural South Africa. J. Acquir. Immune Defic. Syndr. 47(4), 1–21 (2008).
Deuba, K., Kohlbrenner, V., Koirala, S. & Ekström, A. M. Condom use behaviour among people living with HIV: A seven-country community-based participatory research in the Asia-Pacific region. Sex. Transm. Infect. 94(3), 200–205 (2018).
Haddad, L. B. et al. Pregnancy prevention and condom use practices among HIV-infected women on antiretroviral therapy seeking family planning in Lilongwe, Malawi. PloS One 10(3), e0121039 (2015).
Berhane, Y., Berhe, H., Abera, G. B. & Berhe, H. Utilization of modern contraceptives among HIV positive reproductive age women in Tigray, Ethiopia: A cross sectional study. In Isrn Aids, 2013 (2013).
Dessie, Y., Gerbaba, M., Bedru, A. & Davey, G. Risky sexual practices and related factors among ART attendees in Addis Ababa Public Hospitals, Ethiopia: A cross-sectional study. BMC Public Health 11(1), 422 (2011).
Alene, K. A. Consistent condom use among sexually active hiV-positive women in Amhara region, Ethiopia. Open Access J. Contracept. 5, 85–90 (2014).
Adebayo, A. M. et al. Disclosure to sexual partner and condom use among HIV positive clients attending ART clinic at a tertiary health facility in South West Nigeria. Pan Afr Med J. 18, 245 (2014).
Adefala, N., Sodeinde, K., Osinaike, A., Bamidele, F. & Omotosho, A. Condom use and associated factors among HIV-positive patients accessing care at a private tertiary health institution in the southwest, Nigeria. Babcock Univ. Med. J. 3(1), 49–58 (2020).
Anore, D. L., Mengistie, B. & Geltore, T. E. Unprotected sexual practices and associated factors among adult people living with HIV on antiretroviral therapy in public hospitals of Kembata Tembaro Zone, Southern Ethiopia. Pan Afr. Med. J. 38, 176 (2021).
Geleta, R. H. & Tiruneh, M. A. Condom Utilization and affecting factors among people living with HIV/AIDS attending ART clinics in Addis Ababa, Ethiopia. HIV AIDS (Auckl) 12, 583–590 (2020).
Tadesse, W. B. & Gelagay, A. A. Risky sexual practice and associated factors among HIV positive adults visiting ART clinics in public hospitals in Addis Ababa city, Ethiopia: A cross sectional study. BMC Public Health. 19(1), 113 (2019).
Tesfaye, B., Seifu, Y., Tekleselassie, B. & Ejeso, A. The magnitude and associated factors of consistent condom utilization among ART users in Hawassa City, Sidama, Ethiopia. HIV AIDS (Auckl) 12, 909–922 (2020).
Yeshaneh, A. et al. Consistent condom utilization and associated factors among HIV positive clients attending ART clinic at Pawi general hospital, North West Ethiopia. PLoS One. 16(12), e0261581 (2021).
Ayele, W. M., Tegegne, T. B., Damtie, Y., Chanie, M. G. & Mekonen, A. M. Prevalence of consistent condom use and associated factors among serodiscordant couples in Ethiopia, 2020: A mixed-method study. Biomed. Res. Int. 2021, 9923012 (2021).
Aynalem, G. L., Badi, M. B. & Solomon, A. A. Consistent condom utilization and its associated factors among sexually active female anti-retro viral treatment users in Finoteselam District Hospital, Northwest Ethiopia, 2018. J. Int. Assoc. Provid. AIDS Care 21, 23259582221088430 (2022).
Dessalegn, N. G. et al. HIV Disclosure: HIV-positive status disclosure to sexual partners among individuals receiving HIV care in Addis Ababa, Ethiopia. PLoS One. 14(2), e0211967 (2019).
Thior, I. et al. Urban-rural disparity in sociodemographic characteristics and sexual behaviors of HIV-positive adolescent girls and young women and their perspectives on their male sexual partners: A cross-sectional study in Zimbabwe. PLoS One. 15(4), e0230823 (2020).
Workie, H. M., Kassie, T. W. & Hailegiyorgis, T. T. Knowledge, risk perception, and condom utilization pattern among female sex workers in Dire Dawa, Eastern Ethiopia 2016: A cross-sectional study. Pan Afr. Med. J. 32, 185 (2019).
Tilahun, Y., Bala, E. T., Bulto, G. A. & Roga, E. Y. Dual contraceptive utilization and associated factors among reproductive-age women on anti-retroviral therapy at hospitals in Central Ethiopia. Risk Manag. Healthc. Policy 14, 619–627 (2021).
Walusaga, H. A., Kyohangirwe, R. & Wagner, G. J. Gender differences in determinants of condom use among HIV clients in Uganda. AIDS Patient Care STDS 26(11), 694–699 (2012).
Enegela, J. E. et al. Rates of condom use among HIV positive patients on ART in Nasarawa Eggon North Central Nigeria. Biomed. J. Sci. Tech. Res. 18(5), 13842-13847 (2019).
Madiba, S. & Letsoalo, B. Disclosure, multiple sex partners, and consistent condom use among HIV positive adults on antiretroviral therapy in Johannesburg, South Africa. World J. AIDS 04(01), 12 (2014).
Aboubacrine, S. A. et al. Inadequate adherence to antiretroviral treatment and prevention in hospital and community sites in Burkina Faso and Mali: A study by the ATARAO group. Int. J. STD AIDS 18(11), 741–747 (2007).
Ajayi, O. A. et al. Consistent condom use and associated factors among HIV positive women of reproductive age on anti-retroviral treatment in Ogun State, Nigeria. Pan Afr. Med. J. 43, 101 (2022).
Ankunda, R., Atuyambe, L. M. & Kiwanuka, N. Sexual risk related behaviour among youth living with HIV in central Uganda: Implications for HIV prevention. Pan Afr. Med. J. 24, 49 (2016).
Keetile, M. & Kgosidintsi, G. Sexual behaviours of HIV positive adults receiving HAART in Botswana: A cross sectional study. Afr. Health Sci. 18(3), 503–511 (2018).
Nakiganda, L. J. et al. Cross-sectional comparative study of risky sexual behaviours among HIV-infected persons initiated and waiting to start antiretroviral therapy in rural Rakai, Uganda. BMJ Open 7(9), e016954 (2017).
Obi, S. N., Onah, H. E., Ifebunandu, N. A. & Onyebuchi, A. K. Sexual practices of HIV-positive individuals: The need for continued intervention in developing countries. J. Obstet. Gynaecol. 29(4), 329–332 (2009).
Ragnarsson, A. et al. Sexual risk taking among patients on antiretroviral therapy in an urban informal settlement in Kenya: A cross sectional survey. J. Int. AIDS Soc. 20, 1–8 (2011).
Wagner GJ, Holloway I, Ghosh-Dastidar B, Ryan G, Kityo C, Mugyenyi P. Factors Associated with Condom Use Among HIV Clients in Stable Relationships with Partners at Varying Risk for HIV in Uganda. AIDS and Behavior. 2010:1–11.
Wong, W. C. W. et al. Contextual factors associated with consistent condom use and condom self-efficacy amongst African asylum seekers and refugees in Hong Kong. Infect. Dis. Health 23(1), 23–32 (2018).
Bryan, A. E. et al. Condom-insistence conflict in women’s alcohol-involved sexual encounters with a new male partner. Psychol. Women Q. 41(1), 100–113 (2017).
Ajayi, A., Nwokocha, E., Akpan, W., Adeniyi, O. & Goon, D. It’s sweet without condom”: Understanding risky sexual behaviour among Nigerian Female University students. Online J. Health Allied Sci. 16(4), 9 (2017).
Patterson, A. S. The African State and the AIDS Crisis (Routledge, London, 2018).
Kharsany, A. B. & Karim, Q. A. HIV infection and AIDS in Sub-Saharan Africa: Current status, challenges and opportunities. Open AIDS J. 10, 34–48 (2016).
Indravudh, P. P., Choko, A. T. & Corbett, E. L. Scaling up HIV self-testing in sub-Saharan Africa: A review of technology, policy and evidence. Curr. Opin. Infect. Dis. 31(1), 14 (2018).
HIV/AIDS JUNPo. Fast-Track: Ending the AIDS Epidemic by 2030 2014 (UNAIDS, Geneva, 2014).
Acknowledgements
We are grateful to the authors and publishers for giving open-access articles for the review of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors are involved in the overall review process. Y.W., T.W., D.E., G.D., A.E., and S.B. participated in conception, literature review, and data extraction. E.K.B. and T.D.T. did the analysis and interpretation of data. A.S.K. and S.A. participated in manuscript preparation. D.E. revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Endeshaw, D., Dessie, G., Kasa, A.S. et al. Consistent condom utilization among sexually active HIV positive individuals in Sub-Saharan Africa: systematic review and meta-analysis. Sci Rep 14, 5837 (2024). https://doi.org/10.1038/s41598-024-56574-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-56574-5
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.