Abstract
In this study, according to the Location, Diameter, Risk factor (LDRf) classification principle, the influence and effect of esophageal varices diameter on the degree of complete ligation of multicyclic ligator were investigated. Methods. The esophageal veins of healthy piglets were filled with methylene blue solution, and the in vitro pig esophageal varices model was made, which were divided into three groups according to the diameter of esophageal varices: D1, 0.4–1.0 cm; D2, 1.1–1.5 cm; and D3, 1.6–2.0 cm. Finally, the ligation effect of each group was analyzed statistically. A total of 407 ligations were performed on the simulated esophageal variceal model. There were 103 ligations in the D1 group and 98 were complete (95.15%, 98/103); 151 ligations in the D2 group and 47 were complete (31.13%, 47/151); and 153 ligations in the D3 group but none were complete (0%, 0/153). There was significant difference in the degree of complete ligation between the two groups (χ2 = 38.0014, P ≤ 0.001). In the varicose ligation model, the complete ligation effect was the most complete and robust when the varicose diameter was 0.4–1.0 cm. This study showed that the varicose vein diameter in LDRf classification was reasonable and feasible to guide endoscopic varicose vein ligation.
Similar content being viewed by others
Introduction
Esophageal variceal bleeding is a serious complication of cirrhosis. If no treatment is given after the first bleeding, the 6-week mortality rate is as high as 15 to 20%, and the 1-year rebleeding rate is as high as 60%. Band ligation or non-selective β blockers (NSBB) are currently the main methods for the primary prevention of cirrhosis and esophageal variceal bleeding. Band ligation combined with NSBB is the main method for the secondary prevention of cirrhosis and rebleeding of esophageal varices1,2,3,4,5.
Meta-analysis showed that the emergency hemostasis rate of EIS was 95% (76–100%), which was not significantly different from EVL6, while EVL had a higher rate of variceal eradication, lower rebleeding rate, and lower complication rate7. At present, foreign guidelines recommend EVL as the first choice of treatment for acute EVB3,8,9,10.
Endoscopic variceal ligation (EVL) is a safe and effective method for the eradication of esophageal varices. It is reported that the effective rate of ligation for esophageal varices is equal to or higher than sclerotherapy11,12. But its effect on different diameters of esophageal varices was not yet well investigated now.
For esophagogastric varices (GOV), the classification and grading criteria are different between domestic and foreign countries, the sarin typing is often used abroad13. In 2008, a new LDRf typing was proposed by the professor Linghu Enqiang in China7,14, and this consensus was recommended by Chinese Association of Digestive Endoscopy. LDRf is based on the previously published grading system15,16,17, which covers the entire gastrointestinal varicosis, and is easy to memorize and easy to write, and integrates recording, typing, treatment, and timing of treatment. The LDRf classification is described and recorded by three factors:location (L), diameter (D) and risk factor (Rf), which was expressed as follows: LXxD0.3–5.0 Rf0,1,2. (see Tables 1, 2).
In this study, a model of esophageal varices of pigs with different diameters was constructed as the research object, and in vitro simulated EVL experiments were carried out to observe the influence of variceal vessels of different diameters on the effect of banding.
Materials and methods
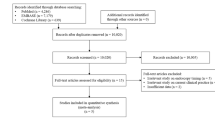
We made model EVL of animals pig, and this simulated experimental study was carried out according to the LDRf classification criteria15. Institutional Animal Care and Use Committee of Capital Medical University (protocol number: 201203031-001) and PLA General Hospital (protocol number: 20110323-001) approved all procedures. All experimental procedures were performed in accordance with relevant guidelines and regulations. This study is reported in accordance with ARRIVE guidelines, https://arriveguidelines.org.
Animals and equipment
Experimental animals
Experimental pigs, 3–24 months old, all female, weighing 40 ± 20 kg, were clinically healthy and were purchased from Liuli River Experimental Pig Farm, Fangshan District, Beijing.
Experimental equipment and drugs
Experimental equipment includes anesthesia machine, monitor, anesthesia bed, laryngoscope, stethoscope and other commonly used items. The equipment includes Olympus-240 electronic gastroscope, Wilson-Cook six-shot ligation device, Vernier caliper, and T-shape tubes. Glucose methylene blue solution was used to fill the veins for visibility.
The experimental drugs included atropine, dexamethasone, midazolam, sodomethacin, succinylcholine, diazepam injection, lidocaine, etc.
Anesthesia method
Piglets were given intravenous general anesthesia, and the anesthesia method is divided into two stages:
Anesthesia induction phase
Administration before induction: Intramuscular injection of atropine 0.5 mg and dexamethasone 10 mg is routinely given before anesthesia induction to reduce the secretion of salivary glands and tracheal glands and prevent allergic reactions. The anesthesia induction drugs were midazolam 0.1–0.2 mg/kg and Sumisan 0.25–0.3 ml/kg compound drugs.
Anesthesia maintenance phase
The anesthesia maintenance medication is to use 6 succinylcholine, 6 diazepam injection, and 7 lidocaine to be added to 500 ml of balanced solution to prepare an anesthetic mixture for slow intravenous infusion, first rapid infusion of 5–10 ml, and after the experimental animal anesthesia is complete, the drip rate is slowed down to 40–60 drops/min.
Selecting the pig veins
We opened the abdominal cavity of the pigs and selected the inferior vena cava, portal vein, superior mesenteric vein, and limb veins of different thickness.
Pig variceal model and measurement of varicose vein diameter
One end of the vein was ligated and the other end connected to the T tube, whose other end was connected to the glass column burette filled with methylene blue liquid The T tube was opened so that the water flowed into the vein, and the water column gradually decreased, while the porcine vein was gradually filled. When the water flow stopped, the end of the vein that was connected to the T tube was ligated to produce porcine variceal models with different diameters ranging from 0.4 to 2.0 cm and lengths of 3.0–4.0 cm, as measured with a vernier caliper (Figs. 1, 2).
Selecting the pig esophagus
The pig's esophagus is about 40 cm long, divided into three sections, each about 13 cm long,, and the esophageal lining was flipped out. The mucosa and muscularis propria layers were bluntly dissected with a hemostat, forming a submucosal tunnel (Figs. 3, 4).
Pig model of esophageal varices
Using a hemostat, the pig modeled varicose vein was introduced through the esophageal tunnel between the muscularis propria and submucosal layers, to form the pig model of esophageal varices.
Measuring esophageal variceal diameter
The diameter of the esophageal varices was measured by a vernier caliper, and divided into three groups according to the LDRf classification of the variceal different diameters: D1, 0.4–1.0 cm; D2, 1.0–1.5 cm; and D3, 1.6–2.0 cm (Fig. 5).
Pig variceal ligation model
The multiple-shot ligation device pre-fixed to the front end of the endoscope was used to target the esophageal varicose vein to create continuous suction. When the suction pressure rose to 0.03–0.05 MPa18 and the endoscopic vision gradually became completely blue, the rubber band was released to stop the suction and ligated at the base of the vein19 (Fig. 6). The esophageal mucosa was cut off and separated after ligation, and the vein was dissected after submucosal ligation. The ligation effect was observed and judged as complete (100%), incomplete (50%), and no ligation (Fig. 7a–c).
Statistical analysis
We have used SPSS Version 13.0 software to carry out the statistical analysis which is given in this manuscript. P < 0.05 was considered statistically significant.
Results
Esophageal variceal diameter
A total of 407 ligation models of simulated esophageal varices were formed: 103 in the D1 group, 151 in the D2 group, and 153 in the D3 group.
Pig variceal ligation rate
Univariate analysis of the effect of in vitro ligation of esophageal varices of different diameters was as follows. For the D1 group, there were 98 complete ligations (24.1%, 98/407), one incomplete ligation (0.2%, 1/407), and four ligation failures (1%, 4/407). For the D2 group, there were 47 complete ligations (11.5%, 47/407), 41 incomplete ligations (10.1%, 41/407), and 63 ligation failures (15.5%, 63/407). For the D3 group, there were no complete ligations (0%, 0/407), no incomplete ligations (0%, 0/407), and 153 ligation failures. The results showed that there was a significant difference in the number of complete ligations between the groups (χ2 = 38.0014, P < 0.05). The results for ligation of varices with different diameters are shown in Tables 3 and 4.
Discussion
Endoscopic treatment of esophageal varices is mainly by ligation and supplemented by sclerosis.. Ligation and sclerotherapy have their own advantages and disadvantages, and should be based on the characteristics of each method. Re-examination of gastroscopy 1 week after emergency ligation of severe esophagogastric varices and the discharge time should be determined according to the results of gastroscopy, which can effectively reduce rebleeding after banding. Severe esophageal varices should be mainly ligation, with emphasis on preventing re-bleeding and alleviating varices. Mild and moderate esophageal varices should be mainly scleroded, focusing on the treatment of deep mucosal varices and perforating branches to reduce recurrence, and at the same time, due to the small amount of sclerosing agent, the incidence of complications after sclerosing agent injection is effectively reduced. When necessary, the treatment should be supplemented with transparent caps and tissue glue.
EVL therapy is one of the latest methods in treatment of esophageal variceal bleeding, which was first reported by Stiegmann in 198620. The therapeutic effect of EVL has the following mechanisms21: (1) mechanical blockade of the blood flow of the varicose veins to make the varices shrink; (2) thrombosis at the ligation site of the varicose vein and occurrence of organizing or calcification; (3) scar formation and fibrosis in the wall of the ligated vein; (4) degradation or disappearance of the varicose veins after ligation.
Esophageal variceal bleeding is the major complication and cause of death in patients with cirrhosis. How to seize the opportunity to reduce or eliminate the esophageal varicosis is the most important means to prevent bleeding.
The principle of EVL is to block the varicose vein blood flow emergency hemostasis, so that the ligation of venous thrombosis, tissue necrosis, fibrosis formation, and finally make the varicose vein disappear. EVL includes single ligature, multiple ligature and nylon rope ligature. Repeated ligation is superior/not inferior to repeated sclerotherapy in the treatment of esophageal varices, but the incidence of side effects (including esophageal stenosis, perforation, infection, etc.) is significantly lower. Simultaneous combination of ligation and sclerotherapy for esophageal variceal vein rupture bleeding is not superior to repeated ligation treatment22,23,24,25.
Many studies have shown 90% hemostasis after emergency therapy for esophageal variceal bleeding by endoscopic ligation26. Ligation therapy has become the first choice of endoscopic treatment with good results, due to the rapid disappearance of varices, few complications, simple operation, and low rebleeding rate after ligation. However, variceal ligation has some risk, especially the ligation ring may fall off triggering the bleeding which is difficult to control. Three results can occur after ligation of esophageal varices: (1) complete ligation, indicating that the ligation effect is certain and complete, and the ligation ring at the root of the ligated varicose veins is not easy to slip off and is strong and stable; (2) incomplete ligation (the root of the varicose veins is not completely ligated, ligation only less than or equal to 50%), indicating that the effect of banding was uncertain and incomplete, and the ligature knot was easy to fall off early, which was easy to induce massive bleeding and increase mortality. (3) ligation failure, indicating that the banding ring cannot ligature the root of varicose veins.
From above consideration, it is necessary to carry out clinical studies on the surgical methods, indications and other aspects of EVL. Studies have shown that the factors affecting EVL efficacy include the following. (1) Variceal diameter > 1.0 cm, at which point the ligature ring is unable to tie the entire varicose vein, and the ligature ring often falls off, resulting in fatal bleeding. (2) Ligation techniques that directly affect the efficacy include: correct positioning of varicose veins, adequate attachment of sucking, making the venous bulb in the transparent cap as full as possible, and avoiding ineffective sucking. This study shows that for varicose vein diameter > 1.5 cm, not completely ligation. For varicose vein diameter < 0.3 cm, the ligation device directly inhaled the esophageal muscle layer into the transparent cap; Then ligation the muscle layer. In this case, the patient experienced long-term postoperative pain and scar stenosis. (3) For varicose veins with severe mucosal erosions or blood blisters, excessive sucking during ligation can sometimes cause severe mucosal damage and induce bleeding, which directly affects the efficacy27.
In this study, in the 103 variceal ligations in D1 group (diameter 0.4–1.0 cm), the rate of complete ligation was 95.15% (98/103), it indicates that the ligated vascular root is firm and determined. In 151 variceal ligations in D2 group (diameter 1.1–1.5 cm), the rate of complete ligation was 31.13% (47/151). However, in 153 variceal ligations in D3 group (diameter 1.6–2.0 cm), the rate of complete ligation was 0%. Thus, for varices with diameter 0.4–1.0 cm, the ligation effect was most complete, and the success rate was the highest, while the ligation failure rate was highest for varices > 1.6 cm in diameter. Therefore, it is particularly important to measure the diameter of esophageal varices on an endoscopic scale27,28. This can better apply LDRf typing to guide endoscopic therapy, reduce the risk of endoscopic variceal hemorrhage, and improve the success rate of hemostasis.
In this study, the ligation diameter of esophageal varices in pigs was < 1.5 cm, and this experimental results are consistent with those reported in previous literatures. EVL has rapid eradication of varicose veins and few complications, but the recurrence rate of varicose veins is high. EVL can block the bleeding collateral of the left gastric vein, esophageal vein and vena cava, but after the blood flow of the esophageal vein is blocked, the gastric coronary vein and the perigastric venous plexus have vascular dilation, increased blood flow, and increased recurrence rate over time, so repeated ligation and consolidation therapy are often required21,22,23,24.
When cirrhosis portal hypertension occurs, the pressure in esophageal varices increases, causing venous dilation, diameter increase, venous wall thinning, and venous wall tension increase. When the critical value is reached, the venous wall rupture bleeding29,30,31. Our previous experimental studies have confirmed that the esophageal variceal pressure is a major factor affecting ligation32.
To date, there have been published literature on life threatening massive bleeding due to ulceration following variceal banding and early spontaneous slippage of rubber bands33,34,35, especially 5 to 10 days after the procedure when the O-ring detaches.However, we will be unable to predict the presence of an ulceration with a residual vein at its base and to evaluate the thrombosis of that vein after EVL until detachment of the O-ring36. There are other literature reports that percutaneous transhepatic obliteration (Percutaneous transhepatic obliteration, PTO) is one of the useful rescue procedures for life-threatening bleeding after EVL for severe esophagogastric varices37. or additional sclerotherapy immediately after EVL may be required to prevent this fatal complication. Thus ,further studies will be needed in order to identify the specific risk factors for potentially fatal complications of this type38.
In this experimental model, one limitation of the present study was that we used normal vessels dilated that do not correspond to the natural esophageal varices formation since the varicose veins vessels are not normal because their varicose veins angiogenesis happen as a vessel slowly becomes blocked, and the lack of the present method is that could not be compared to the natural esophageal varices produced by cirrhosis. I think although interfering in the results for guiding role of esophageal variceal diameter in treatment of endoscopic ligation, but this experiment is based on the previous research project "Esophageal variceal pressure influence on the effect of ligation"31, and variceal veins of different diameters were simulated with the esophagus of animal pigs to perform endoscopic ligation experiments, and further verified the guiding effect of variceal vein diameter on endoscopic ligation in LDRf typing. So, I believe this animal simulation experiment has preliminarily verified the guiding effect of varicose diameter in LDRf typing on endoscopic ligation. However, a large number of clinical studies are needed to verify the guiding role of LDRf typing. Certainly, the results of this animal simulation experiment maybe it would be more efficient as a simulation for endoscopic ligation training.
Therefore, multi-factor experiments are needed, and measuring the diameter and pressure of esophageal varices has important clinical significance for evaluating the risk of bleeding and its control effect.
Data availability
The majority of dataset analysed during the current study is available in Supplementary Table 1, while other raw datasets generated during this study are available form the corresponding author (Zhiqun Li) on reasonable request.
References
Tripathi, D. et al. UK guidelines on the management of variceal haemorrhage in cirrhotic patients. Gut 64, 1680–1704 (2015).
de Franchis, R. Expanding consensus in portal hypertension Report of the Baveno VI Consensus Workshop: Stratifying risk and individualizing care for portal hypertension. J. Hepatol. 63, 743–752 (2015).
European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis. J. Hepatol. 69(2), 406–460 (2018).
Garcia-Tsao, G., Abraldes, J. G., Berzigotti, A. & Bosch, J. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the Study of Liver Diseases. Hepatology 65(1), 310–335 (2017).
de Franchis, R. Revising consensus in portal hypertension: Report of the Baveno V consensus workshop on methodology of diagnosis and therapy in portal hypertension. J. Hepatol 53, 762–768 (2010).
Chinese Society of Hepatology, Chinese Society of Gastroenterology, Chinese Society of Digestive Endoscopy, Chinese Society of Liver Cirrhosis. Portal hypertension, esophageal and gastric variceal bleeding prevention and treatment guidelines. Chin. J. Gastrointest. Endosc. 2(4), 1–21 (2015).
Dai, C. et al. Endoscopic varicel ligation compared with endoscopic injection sclerotherapy for treatment of esophageal variceal hemorrhage: A meta-analysis. World J Gastroenterol 21(8), 2534–2541 (2015).
Tripathi, D. et al. Clinical Services and Standards Committee of the British Society of Gastroenterology UK guidelines on the managerment of variceal haemorrhage in cirrhotic patients. Gut 64(11), 1680–1704 (2015).
Garcia-Tsao, G. et al. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management:2016 practice guidance by the American Association for the study of liver diseases. Hepatology 65(1), 310–335 (2017).
de Franchis, R. et al. Baveno VII Faculty. Baveno VII-renewing consensus in hypertension. J. Hepatol. 76(4), 959–974 (2022).
Laine, L. & Cook, D. Endoscopic ligation compared with sclerotherapy for treatment of esophageal variceal bleeding: A meta-analysis. Ann. Intern. Med. 123, 280–287 (1995).
Tait, I. S., Krige, J. E. & Terblanche, J. Endoscopic band ligation of oesophageal varices. Br. J. Surg. 86, 437–446 (1999).
Sarin, S. K. & Kumar, A. Gastric varices: Profile, classification, and management. Am. J. Gastroenterol. 84(10), 1244–1249 (1989).
Esophageal and Gastric Varices Group, Society of Digestive Endoscopy, Chinese Medical Association. Endoscopic diagnosis and treatment of gastrointestinal varices and hemorrhage. Chin. J. Digest. Endosc. 27(1), 1–4 (2010).
Linghu, E. A new endoscopic varicose vein classification method was preliminarily discussed. Chin. J. Dig. Endosc. 25, 505–506 (2008).
Japanese Research Society for Portal Hypertension. The general rules for recording endoscopic findings on esophageal varices. Jpn. J. Surg. 10, 84–87 (1980).
Idezuki, Y. General rules for recording endoscopic findings of esophagogastric varices (1991). Japanese Society for Portal Hypertension. World J. Surg. 19, 420–422 (1995).
Wang, G. F. & Xie, H. Intraoperative nursing in esophageal varices ligation therapy. J Clin Med Res 13, 1039 (2007).
Liu, M. et al. Clinical application of self-made new pneumatic activated esophageal ligator. Chin. J. Endoscop. 8, 48–49 (2002).
Stiegmann, G. V., Gambre, T. & Sun, J. H. A new endoscopic elastic band ligating device. Gastrointest. Endosc. 32, 230–233 (1986).
Hu, W. M. & Yin, C. L. Endoscopic rubber band ligation for treatment of esophageal/gastric varices. New Gastroenterol. Dis. 4, 587–588 (1996).
Dai, C., Liu, W.-X., Jiang, M. & Sun, M.-J. Endoscopic variceal ligation compared with endoscopic injection sclerotherapy for treatment of esophageal variceal hemorrhage: A meta-analysis. World J. Gastroenterol. 21, 2534–2541 (2015).
de Quadros Onofrio, F., Pereira-Lima, J. C., Valença, F. M., Azeredo-da-Silva, A. L. & Stein, A. T. Efficacy of endoscopic treatments for acute esophageal variceal bleeding in cirrhotic patients: Systematic review and metaanalysis. Endosc. Int. Open 7(11), E1503–E1514 (2019).
Karsan, H. A. et al. Combination Endoscopic band ligation and sclerotherapy compared with endoscopic band ligation alone for the secondary prophylaxis of esophageal variceal hemorrhage: A meta-analysis. Dig. Dis. Sci. 50, 399–406 (2005).
Singh, P., Pooran, N., Indaram, A. & Bank, S. Combined ligation and sclerotherapy versus ligation alone for secondary prophylaxis of esophageal variceal bleeding: A meta-analysis. Am. J. Gastroenterol. 97, 623–629 (2002).
Berkelhammer, C. et al. “Pinch” injury during over-tube placement in upper endoscopy. Gastrointest. Endosc. 39, 186–188 (1993).
Shan, Z. Y. et al. Clinical effect of endoscopic variceal ligation on esophageal varices bleeding of cirrhotic patients. Infect. Dis. Info 20, 105–106 (2007).
Li, Z. Q. & LingHu, E. Q. Application of LDRf typing methods on ectopic varices in the digestive tract. Chin. J. Gastroenterol. 2, 64–66 (2013).
Li, Z. Q. et al. Feasibility study on use of the esophageal varices diameter scale in measuring the in vitro simulated varicose veins. Chin. J. Endoscop. Surg. Electron. Vers. 4, 402–404 (2011).
LingHu, E. Q. Preliminary study on a new endoscopic variceal typing. J Gastroenterol 25, 505–506 (2008).
Polio, J. et al. Critical evaluation of a pressure-sensitive capsule for measurement of esophageal varix pressure Studies in vitro and in canine mesenteric vessels. Gastroenterology 92(5 pt 1), 1109–1115 (1987).
Li, Z.-Q. et al. Esophageal variceal pressure influence on the effect of ligation. World J. Gastroenterol. 21(13), 3888–3892 (2015).
Sakai, P. et al. Is endoscopic band ligation of esophageal varices contraindicated in Child-Pugh C patients?. Endoscopy 26, 511–512 (1994).
Van Vlierberghe, H., De Vos, M., Haute-keete, M. & Elewaut, A. Severe bleeding fol-lowing endoscopic variceal ligation: Should EVL be avoided in Child C patients?. Acta Gastroenterol. Belg. 62, 175–177 (1999).
Toyoda, H. et al. Fatal bleeding from a residual vein at the esophageal ulcer base after successful endoscopic variceal ligation. J. Clin. Gastroenterol. 32, 158–160 (2001).
Toyoda, H. et al. Fatal bleeding from a residual vein at the esophageal ulcer base after successful endoscopic variceal ligation. J. Clin. Gastroenterol. 32(2), 158–160 (2001).
Chikamori, F., Ito, S. & Sharma, N. Percutaneous transhepatic obliteration for life-threatening bleeding after endoscopic variceal ligation in a patient with severe esophagogastric varices. Radiol. Case Rep. 18(2), 624–630 (2022).
Mishin, I. & Dolghii, A. Early spontaneous slippage of rubber bands with fatal bleeding: A rare complication of endoscopic variceal ligation. Endoscopy 37(3), 275–276 (2005).
Acknowledgements
The authors wish to thank Capital Medical University Pinggu Hospital (Beijing, China) for technological assistance in carrying out this research.
Funding
The authors of this paper received the Special Grant of China’s Postdoctoral Science Fund (No.2012T50868), and the District Emergency Project Startup Fund of Beijing Municipal Government Priority Programs (No. Z111107056811048) towards the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
E.L. developed the LDRf typing concept and designed the research protocol. Z.L. performed data analysis and wrote the manuscript. B.S., W.L. prepared figures. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, Z., LingHu, E., Li, W. et al. Guiding role of esophageal variceal diameter in treatment of endoscopic ligation: an animal experimental study. Sci Rep 14, 3929 (2024). https://doi.org/10.1038/s41598-024-53752-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-53752-3
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.