Abstract
The coronavirus disease 2019 (COVID-19) pandemic had severe impact on the outcome of out-of-hospital cardiac arrest (OHCA) patients and the possibility of bystander cardiopulmonary resuscitation (CPR). Previous studies focused only on the short periods of the pandemic and reported a significant increase in the number of infections. In a retrospective cohort study we aimed to compare the outcomes of OHCA patients 1 year before and 1 year after the onset of COVID-19. Data of 519 OHCA patients during the pre-pandemic (January–December 2019; 262 patients) and intra-pandemic (April 2020–March 2021; 257 patients) periods in Yokohama Municipal Hospital, Japan were collected and analysed retrospectively. The study outcomes were the return of spontaneous circulation (ROSC), admission to hospital, survival to discharge, and cerebral performance category at discharge. The intra-pandemic period was associated with decreased bystander CPR (P = 0.004), prolonged transport time (P < 0.001), delayed first adrenaline administration (P < 0.001), and decrease in ROSC (P = 0.023). Logistic regression analysis revealed that the following factors were significantly associated with ROSC: “pandemic”, “shockable initial waveform”, and “witness presence”.
Similar content being viewed by others
Introduction
In September 2021, the city of Yokohama, with a total population of 3,778,876, has experienced the most explosive outbreak since the beginning of the COVID-19 pandemic in Japan, with a cumulative total of 65,585 infected people and 490 deaths (up to 10 September 2021)1. The coronavirus disease 2019 (COVID-19) outbreak resulted in high infection and mortality rates worldwide. The COVID-19 pandemic also affected out-of-hospital cardiac arrest (OHCA) patients. Previous studies have highlighted reduced return of spontaneous circulation (ROSC) rates and survival rates in patients with OHCA during the pandemic2,3,4,5,6. Five elements are critical to the survival of patients with OHCA: a call to emergency medical services (EMS), immediate and high-quality cardiopulmonary resuscitation (CPR), early defibrillation, EMS transport and advanced resuscitation, and treatment after resumption of cardiac rhythm7. Observational studies in COVID-19 endemic areas have noted an increase in OHCA, a decrease in the occurrence of outdoor cardiac arrest, a decrease in bystander CPR and automated external defibrillator (AED) use, and an increase in EMS response time3,4,5,8,9,10,11. However, previous studies have focused only on the short periods of the pandemic, during which there were significant increases in the number of infections.
In this study, we aimed to compare the outcomes of patients with OHCA who were transported to Yokohama Municipal Hospital, a tertiary emergency hospital in Yokohama City, 1 year before and 1 year after the onset of the COVID-19 pandemic.
Results
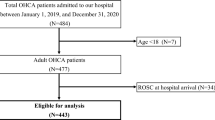
During the study period, 694 OHCA patients were transported to our hospital; of these, 175 patients (DNAR [n = 29], institutional cardiac arrest [n = 49], non-cardiac arrest [n = 14], and trauma [n = 83]) were excluded. In total, 519 patients were included in the study (262 and 257 in the pre-pandemic and intra-pandemic periods, respectively; Fig. 1).
OHCA Patients in Yokohama City during (1 April 2020 to 31 March 2021) and before (1 February 2019 to 31 December 2019) the COVID-19 pandemic. OHCA out-of-hospital cardiac arrest, DNAR do not attempt resuscitation, COVID-19 coronavirus disease 2019, CPR cardiopulmonary resuscitation. (A) Excluded patients. (B–E) Initial wave form, Location, Witnessed arrest and bystander response of included patients. (F) Outcomes after out-hospital cardiac arrest of included patients.
Table 1 shows the patients’ backgrounds and outcomes; there was a statistically significant decrease in bystander CPR, prolongation of transport time (9.6% increase), and delay in first adrenaline administration (13.2% increase) during the intra-pandemic, compared to that in the pre-pandemic period. When bystander CPR rates were compared by location, only OHCA occurring at home was significantly lower during the intra-pandemic period. As an outcome, there was a statistically significant decrease in ROSC rate during the intra-pandemic period. There were no statistically significant differences in other outcomes (survival at admission, survival to discharge, and cerebral performance category (CPC) at discharge).
Table 2 shows the statistically significant differences in the univariate analysis of the various outcomes. ROSC was statistically significantly associated with shockable rhythm (OR 6.27, 95% CI 1.52–25.9), presence of witnesses (OR 5.18, 95% CI 1.74–15.4), and time from calling EMS to arrival (OR 0.85, 95% CI 0.76–0.97). Unlike the results of the multivariate analysis described below, ROSC was not statistically significantly associated with the intra-pandemic period in the univariate analysis. Survival to admission was associated with the provision of bystander CPR (OR 7.78, 95% CI 2.29–26.4), shockable rhythm (OR 10.0, 95% CI 2.51–39.8), and presence of witnesses (OR 9.67, 95% CI 2.41–38.7). Survival to discharge was associated with shockable rhythm (OR 7.05, 95% CI 1.04–47.8), and good neurological prognosis (CPC1–2) was associated with adrenaline administration (OR 18, 95% CI 0.24–261).
Table 3 shows the results of the multivariate analysis of the outcomes, with a cut-off time of 30 min for the first adrenaline administration. ROSC was significantly associated with the intra-pandemic period (OR 0.56, 95% CI 0.33–0.94), shockable rhythm (OR 6.26, 95% CI 2.53–15.50), and presence of witnesses (OR 2.58, 95% CI 1.54–4.33). Survival to admission was associated with age (> 75 years; OR 0.09, 95% CI 0.02–0.27), shockable rhythm (OR 16.4, 95% CI 5.32–50.90), presence of witnesses (OR 2.84, 95% CI 1.13–7.11), and time from calling EMS to arrival (OR 0.92, 95% CI 0.86–0.98). Survival to discharge was statistically significantly associated with shockable rhythm (OR 11.3, 95% CI 1.99–64.5) and first adrenaline administration within 30 min (OR 15.6, 95% CI 1.74–140). We performed analyses with cut-off values of 10, 20, and 35 min for the time of first adrenaline administration, and similar results were observed. The median duration of adrenaline administration in our patient group was 35 min. The time of the first adrenaline administration was not associated with any of the outcomes (Supplementary Table S1).
Table 4 shows the results of the subgroup analysis for the shockable rhythm and non-shockable rhythm groups. The logistic regression analysis for each outcome showed statistically significant differences in variables such as age (> 75 years) and sex, while there were no statistically significant associations in survival to discharge in the shockable rhythm group.
Table 5 shows the results of the subgroup analysis comparing the presence and absence of witnesses. In the witness group, ROSC was associated with the intra-pandemic period (OR 0.42, 95% CI 0.21–0.87) and shockable rhythm (OR 3.09, 95% CI 1.03–9.23). Survival to admission was significantly associated with age (> 75 years; OR 0.14, 95% CI 0.02–0.53), the intra-pandemic period (OR 0.18, 95% CI 0.05–0.70), and shockable rhythm (OR 14.4, 95% CI 3.91–52.7).
Discussion
There was a statistically significant decrease in bystander CPR, prolongation of transport time, and delay in first adrenaline administration during the intra-pandemic, compared to that in the pre-pandemic period. The results of this study suggest that the COVID-19 pandemic reduced the number of ROSCs of patients with OHCA through prolonged transport time and delayed first adrenaline administration time. Although not shown in this study, it may have reduced survival through the reduction of ROSCs, and further large-scale studies are needed.
The COVID-19 pandemic may have included a wide variety of factors that affect the prognosis of OHCA. Previous studies have also suggested that the COVID-19 pandemic possibly worsened the prognosis of OHCA patients through causes other than known confounders12, such as changes in social life, medical history, and COVID-19-related medical practice. Although we could not examine them in this study, these are areas of consideration for future research.
In the EMS protocol in Yokohama city, chest compression was started after covering the mouth and nose of the patient with a surgical mask. At Yokohama City Hospital, where our study was conducted, chest compressions were stopped during intubation to prevent infection due to aerosol production. These may have affected the resuscitation rate.
The results of the two-group comparison showed a decrease in bystander CPR in the prehospital item comparison, but contrary to expectations, there was no change in the breakdown of where the cardiopulmonary arrests occurred or in the percentage of AED use. This result contradicts previous studies reporting a decrease in OHCA in public places and an increase in private areas2,4.
In this study, there was a statistically significant decrease in bystander CPR. When bystander CPR rates were compared by location, only OHCA occurring at home was significantly lower during the intra-pandemic period. Since the number of cardiac arrests in the home itself has increased, the decrease in bystander CPR rates at home may have contributed to the overall decrease in bystander CPR rates. In previous studies, bystander behavioural changes were cited as the reason for the decrease in bystander CPR during the COVID-19 pandemic. Patient contact and aerosol production from chest compressions are pathways for COVID-19 infection13, and bystanders who do not have the expertise may also choose not to perform CPR due to the fear of infection. However, this may not necessarily be true for those who only experienced bystander CPR in their homes in our study. In Japan, where the population is aging and the birth rate is declining, older adults are likely to be home alone, in which case bystander CPR cannot be performed. Restrictions on going out during the COVID-19 pandemic may have spurred this trend by causing isolation among elderly households.
The time between calls to EMS and arrival at the hospital was prolonged during the intra-pandemic period. Shockable rhythms were less frequently observed during COVID-19. The results of this study suggest that the COVID-19 pandemic reduced shockable rhythms through prolonged transport time. The time was divided into four sections: call to the arrival of EMS at the scene, arrival of EMS at the scene to patient contact, patient contact to departure, departure, and arrival at the hospital; the time was prolonged in two sections: EMS call to scene and arrival at the hospital. The time between emergency calls and the arrival of EMS at the scene was extended by 1 min on average, and similar results were found in studies from Paris and Taiwan14,15. The number of emergency calls in Yokohama City was 194,639 during the pre-pandemic period and 159,049 during the intra-pandemic period, with a decrease observed in the intra-pandemic period16. This contradicts the findings of previous studies that showed an increase in emergency calls during the COVID-19 pandemic17,18. One of the reasons for the prolonged response time despite the decrease in the number of calls is the time required to put on PPE. Previous studies have also suggested that wearing PPE leads to longer transport times19. PPE is necessary to prevent COVID-19 infection20, and the equipment used by emergency teams during OHCA responses has been changed in Yokohama City. Specifically, before the pandemic, only a jumper protective suit was worn on the upper half of the body, but during the pandemic, PPE comprising a jacket and pants was additionally worn. Regarding the delayed hospital arrival time, it is possible that the hospital of choice became more distant during the pandemic period or that traffic congestion due to the increased use of private vehicles in consideration of the risk of public transport-associated infection may have had an effect.
A previous study comparing the risk of infection and the lifesaving rate of CPR in COVID-19-infected patients stated that delaying bystander CPR to wear PPE should only be considered if there is a significant increase in the prevalence of COVID-1921. However, it would be difficult to establish specific criteria for changing the protocol when the prevalence increases by a specific amount, and when in reality, PPE should be worn in all cases.
In this study, time to adrenaline administration was prolonged during the intra-pandemic period, and adrenaline administration within 30 min was significantly associated with survival to discharge. The latest guidelines recommend the administration of adrenaline as early as possible22,23. A recent randomized controlled trial and two meta-analyses showed that the use of epinephrine improved the rate of survival to hospital discharge in OHCA patients24,25,26. Although there is no consensus on the timing of adrenaline administration, there are reports that adrenaline administration in less than 15 min is significantly associated with ROSC27. The early administration of epinephrine (≤ 10 min) was also associated with a favourable neurological outcome in adult bystander-witnessed OHCA28,29. However, there are studies that report poor survival outcomes after administration of epinephrine during CPR30. There are controversies regarding the survival benefits of administration of epinephrine during CPR.
Limitations
Some limitations to this study should be noted. First, we may not have adequately controlled for confounding factors, such as staffing, which may have influenced patient outcomes in relation to the COVID-19 pandemic. Second, we have not been able to measure the duration of CPR interruptions due to changes in protocols, which may have worsened the quality of CPR. Additionally, from our retrospective data analysis we cannot tell about the frequency of intermediate ROSC and whether CPR was performed during transport.
Third, although a sufficiently low p value was detected, our study also used a statistical treatment with a significance level of 0.05 for multiple testing. In addition, our study does not reflect data on deaths of patients that were not transported to a medical institution, because death was obvious at the time of discovery.
Fourthly, the number of deaths in Yokohama City increased by 1605, from 33,019 during the pre-pandemic period to 34,624 during the intra-pandemic period. This number may include COVID-19 influenced deaths; for example, the isolation of elderly people living alone or changes in the pathology of background diseases due to less frequent hospital visits. In addition, the data used were from a single institution (Yokohama Municipal Hospital); hence, the findings of this study may not be generalizable to other regions or institutions. Fifthly, since this was an observational study, we could not suggest any causal relationship. Further research is required to enhance prehospital care.
Conclusions
The COVID-19 pandemic possibly worsened the short- and long-term prognoses of patients with OHCA through various factors such as decreased bystander CPR, prolonged transport time, and time to first adrenaline administration. Significant factors affecting the prognosis of OHCA patients could be mitigated by medical personnel who could shorten the transport time and time to adrenaline administration by securing the intravenous route early. However, this was a single-centre study, and multicentre studies are required to validate these findings.
Methods
Study design
We conducted a retrospective cohort study of adult OHCA patients aged ≥ 18 years who were transported to Yokohama Municipal Citizen’s Hospital by EMS between January and December 2019 before COVID-19 pandemic (pre-pandemic group) and between April 2020 and March 2021 during the pandemic (intra-pandemic group), forming the pre-pandemic and intra-pandemic groups, respectively. Cases reported from January to March 2020 were excluded due to being in the transition period. Patients with ROSC at the time of EMS contact, patients with confirmed Do Not Attempt Resuscitation (DNAR) by EMS orders, patients transferred from other medical facilities, and patients with exogenous OHCA—defined as those whose primary cause of death was one of the following: trauma, drowning, hanging, suffocation, or burns—were excluded from the study. We obtained approval from the Ethical Review Committee (Yokohama municipal citizen’s hospital) and permission from the head of the research institution before conducting this study. This study is a retrospective study using existing data. To protect patient's privacy, each patient is assigned a research subject code so that patients cannot be identified from the research subject code. This research did not involve the acquisition of new samples or information and was conducted using only existing information. Since it was difficult to obtain written informed consent from the research subjects, information about the research was disclosed to them via the website of Yokohama Municipal Hospital, and the research subjects were provided the opportunity to refuse participation in the research being conducted. The study was conducted in accordance with the principles of the Declaration of Helsinki, per the Personal Information Protection Law and National Research Ethics Guideline in Japan.
The derivation group data were collected by one emergency physician from electronic medical charts. The validation cohort data were prospectively collected by resident physicians after they received a short lecture on OHCA.
Study setting and population
Yokohama Municipal Hospital is located in Yokohama City, which has a population of approximately 3.78 million people, and the cumulative number of COVID-19 infected persons was 99,955 as of 31 January 202227. During the intra-pandemic (April 2020–March 2021), the country experienced three waves of infections, in April–May 2020, August 2020, and January–February 2021, with the third wave being the largest. The highest number of new infections was 985 per day (15 January 2021), and the highest number of new cases per week was 66.24 per 100,000 people (12–18 January 2021)31,32. A state of emergency was declared for a total of 132 days from 7 April 2020 to 25 May 2020, and from 8 January 2021 to 21 March 2021 (the lockdown policy mainly restricted the use of restaurants).
EMS in Yokohama city basically treat the OHCA patients according to the Japanese resuscitation guidelines published from the Japan Resuscitation Council (JRC)33 which are developed based on the statements from the International Liaison Committee on Resuscitation (ILCOR)34. That includes provision of Intravenous access, adrenaline administration, airway management using laryngeal tube, and manual chest compressions. No mechanical CPR devices were deployed by EMS during the study period. During the COVID-19 infection-spreading period, the EMS in Yokohama city implemented a protocol to treat all the cardiac arrest patients as possibly having COVID-19. In the EMS protocol, before entering the scene, all staff donned PPE that included N95 masks and eye protection, and a high-efficiency particulate air (HEPA) filter was attached securely to any manual or mechanical ventilation device in the path of exhaled gas. Chest compression was started after covering the mouth and nose of the patient with a surgical mask.
At Yokohama City Hospital, where our study was conducted, chest compressions were stopped during intubation to prevent infection due to aerosol production.
Study protocol and measures
The following prehospital and post-surgical information was collected from the transport and medical charts: age (75 years or older or younger), sex, place of occurrence (home, indoor public space, outdoor public space, or ambulance), presence or absence of witnesses, presence or absence of bystander CPR, rate of bystander CPR by place of occurrence, AED use, initial waveform (shockable or non-shockable), EMS response time {EMS call to scene time (from call to arrival on scene), Scene to contact time (arrival on scene to contact), Contact to departure time(on scene emergency care by EMS), Departure to arrival time (from scene to hospital), EMS call to arrival time (from call to arrival hospital)}, prehospital adrenaline administration, initial adrenaline administration time, cause of death (cardiogenic, noncardiogenic, extrinsic), presence of ROSC, survival at hospitalization, survival at discharge, and good neurological prognosis (CPC1–2) at discharge.
The EMS team was required to wear PPE during the pandemic period to prevent airborne infection. Emergency teams can provide advanced airway clearance, venous route clearance, and adrenaline administration by tracheal intubation or use of a laryngeal tube for patients with cardiac arrest.
Data analysis
All variables were compared during the intra-pandemic and pre-pandemic periods. Categorical variables are presented as frequencies (%) and were compared using Fisher’s exact test. Continuous variables are presented as means (standard deviation) and were compared using the Mann–Whitney U test. In addition, the odds ratio (OR) and 95% confidence interval (CI) were calculated to determine the effect of the pandemic after adjusting for relevant factors using a multivariate logistic regression model with a variable reduction method, and factors other than known confounders were examined. Two subgroup analyses were performed with patient groups divided according to the initial waveform and the presence of witnesses.
Four cut-off values of 10, 20, 30, and 35 min for time to adrenaline administration were used for the sensitivity analysis. Patients were considered cardiogenic if a non-cardiogenic disease (cerebrovascular disease, respiratory disease, or malignancy) could be excluded from the clinical course and laboratory findings.
The following independent and dependent variables were used for logistic regression analysis. Independent variables included provision of AED, provision of prehospital electrical defibrillation, age, provision of bystander CPR, presence of COVID infection, cause of death, place of cardiac arrest, occurring during the intra-pandemic, sex, whether the initial waveform was a shockable rhythm or not, presence of witnesses, EMS response time, adrenaline administration, and time of first adrenaline administration. Dependent variables were ROSC, survival at admission, survival at discharge, and good neurological prognosis (CPC 1–2) at discharge.
All tests were two-tailed and considered statistically significant at p < 0.05. All statistical analyses were performed using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria)35. More precisely, it is a modified version of R commander designed to add statistical functions frequently used in biostatistics.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due to the restriction by IRB, but are available from the corresponding author on reasonable request.
References
Information about the new coronavirus infection. Yokohama city website. https://www.city.yokohama.lg.jp/city-info/koho-kocho/koho/topics/covid-19/
World Health Organization. Coronavirus disease (COVID-19). WHO website. https://www.who.int/emergencies/diseases/novel-coronavirus-2019
Fothergill, R. T., Smith, A. L., Wrigley, F. & Perkins, G. D. Out-of-hospital cardiac arrest in London during the COVID-19 pandemic. Resusc. Plus. 5, 100066. https://doi.org/10.1016/j.resplu.2020.100066 (2021).
Mathew, S. et al. Effects of the COVID-19 pandemic on out-of-hospital cardiac arrest care in Detroit. Am. J. Emerg. Med. 46, 90–96 (2021).
Ortiz, R. F. et al. Influence of the Covid-19 pandemic on out-of-hospital cardiac arrest. A Spanish nationwide prospective cohort study. Resuscitation 157, 230–240 (2020).
Huber, B. C., Brunner, S., Schlichtiger, J., Kanz, K. G. & Bogner-Flatz, V. Out-of-hospital cardiac arrest incidence during COVID-19 pandemic in Southern Germany. Resuscitation 157, 121–122 (2020).
American Heart Association. Highlights of the 2020 American heart association guidelines for CPR and ECC. Am. J. Hear. Assoc. 53, 1689–1699 (2020).
Lim, S. L. et al. Impact of COVID-19 on out-of-hospital cardiac arrest in Singapore. Int. J. Environ. Res. Public Health 18, 3646. https://doi.org/10.3390/ijerph18073646 (2021).
Ball, J. et al. Collateral damage: Hidden impact of the COVID-19 pandemic on the out-of-hospital cardiac arrest system-of-care. Resuscitation 156, 157–163 (2020).
Ahn, J. Y. et al. Impact of the Covid-19 outbreak on adult out-of-hospital cardiac arrest outcomes in Daegu, South Korea: An observational study. Clin. Exp. Emerg. Med. 8, 137–144 (2021).
Nishiyama, C. et al. Influence of COVID-19 pandemic on bystander interventions, emergency medical service activities, and patient outcomes in out-of-hospital cardiac arrest in Osaka City, Japan. Resusc. Plus 5, 100088. https://doi.org/10.1016/j.resplu.2021.100088 (2021).
Burns, T. A. et al. Decreases in out of hospital cardiac arrest (OHCA) outcome metrics persist when known COVID patients are excluded from analysis. Am. J. Emerg. Med. 51, 64–68 (2022).
World Health Organization. Infection prevention and control of epidemic-and pandemic prone acute respiratory infections in health care. WHO website. https://www.who.int/publications/i/item/infection-prevention-and-control-of-epidemic-and-pandemic-prone-acute-respiratory-infections-in-health-care
Marijon, E. et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: A population-based, observational study. Lancet Public Health 5, e437–e443. https://doi.org/10.1016/S2468-2667(20)30117-1 (2020).
Yu, J. H. et al. Impact of the COVID-19 pandemic on emergency medical service response to out-of-hospital cardiac arrests in Taiwan: A retrospective observational study. Emerg. Med. J. 38, 679–684 (2021).
Statistical information on fire and disaster prevention in Kanagawa Prefecture. Kanagawa Prefecture website. https://www.pref.kanagawa.jp/docs/kd8/cnt/f470375/index.html
Prezant, D. J. et al. System impacts of the COVID-19 pandemic on New York City’s emergency medical services. J. Am. Coll. Emerg. Physicians Open 1, 1205–1213 (2020).
Al-Wathinani, A. et al. Increased emergency calls during the covid-19 pandemic in Saudi Arabia: A national retrospective study. Healthcare 9, 1–14 (2021).
Chung, H., Namgung, M., Lee, D. H., Choi, Y. H. & Bae, S. J. Effect of delayed transport on clinical outcomes among patients with cardiac arrest during the coronavirus disease 2019 pandemic. Australas Emerg Care https://doi.org/10.1016/j.auec.2021.11.006 (2021).
Wax, R. S. & Christian, M. D. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can. J. Anesth. 67, 568–576 (2020).
Sayre, M. R. et al. Prevalence of COVID-19 in out-of-hospital cardiac arrest: Implications for bystander cardiopulmonary resuscitation. Circulation 142, 507–509 (2020).
Berg, K. M. et al. Adult advanced life support: 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation 142, S92–S139 (2020).
Panchal, A. R. et al. Part 3: Adult basic and advanced life support: 2020 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 142, S366–S468 (2020).
Perkins, G. D. et al. A randomized trial of epinephrine in out-of-hospital cardiac arrest. N. Engl. J. Med. 379, 711–721 (2018).
Aves, T., Chopra, A., Patel, M. & Lin, S. Epinephrine for out-of-hospital cardiac arrest: An updated systematic review and meta-analysis. Crit. Care Med. 48, 225–229 (2020).
Vargas, M., Buonanno, P., Iacovazzo, C. & Servillo, G. Epinephrine for out of hospital cardiac arrest: A systematic review and meta-analysis of randomized controlled trials. Resuscitation 145, 151–157 (2019).
Data related to new coronavirus infections in Yokohama. Yokohama city website. https://data.city.yokohama.lg.jp/covid19/
Tanaka, H. et al. Favorable neurological outcomes by early epinephrine administration within 19 minutes after EMS call for out-of-hospital cardiac arrest patients. Am. J. Emerg. Med. 34, 2284–2290 (2016).
Hayashi, Y. et al. Impact of early intravenous epinephrine administration on outcomes following out-of-hospital cardiac arrest. Circ. J. 76, 1639–1645 (2012).
Fukuda, T. et al. Effect of prehospital epinephrine on out-of-hospital cardiac arrest: A report from the national out-of-hospital cardiac arrest data registry in Japan, 2011–2012. Eur. J. Clin. Pharmacol. 2016(72), 1255–1264. https://doi.org/10.1007/s00228-016-2093-2 (2016).
Outbreaks of patients infected with the new coronavirus. Kanagawa prefecture website. https://www.pref.kanagawa.jp/docs/ga4/covid19/occurrence.html
Latest infection trends in the prefecture. Kanagawa prefecture website. https://www.pref.kanagawa.jp/osirase/1369/
Japan Resuscitation Council. JRC resuscitation guidelines. https://www.jrc-cpr.org/jrc-guideline-2020/
Soar, J. et al. 2019 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation 140, e826-880. https://doi.org/10.1161/CIR.0000000000000734.(2019) (2019).
Kanda, Y. Investigation of the freely-available easy-to-use software “EZR” (Easy R) for medical statistics. Bone Marrow Transpl. 48, 452–458 (2013).
Acknowledgements
We would like to acknowledge the efforts of pre-hospital health professionals in providing excellent health care during the COVID-19 pandemic.
Funding
The authors did not receive any funding for this study.
Author information
Authors and Affiliations
Contributions
All authors have made significant contributions to the preparation of this report in the following areas. (1) Conception and design of the study, analysis, and interpretation of data. (2) Drafting the paper and critically revising it for important intellectual content. (3) Final approval of the submitted version. K.W., K.M., K.S., T.A., S.I., and I.T. were involved in study design, data collection and data interpretation. K.W., K.M., and T.A. were involved in the data analysis. All authors critically revised the report, commented on drafts of the manuscript, prepared all figures and approved the final report.
Corresponding author
Ethics declarations
Competing interests
The authors declare that there are neither financial nor non-financial benefits.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Watanabe, K., Mori, K., Sato, K. et al. Out-of-hospital cardiac arrest patients during the coronavirus disease 2019 pandemic. Sci Rep 13, 23005 (2023). https://doi.org/10.1038/s41598-023-50150-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-50150-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.