Abstract
This study was conducted to analyze the association of Luteinizing Hormone/Choriogonadotropin Receptor (LHCGR) gene rs4953616 and rs7371084 polymorphisms with the risk of polycystic ovary syndrome (PCOS) in Punjab, India. A total of 823 women (443 PCOS cases and 380 healthy controls) were enrolled in the present study. The polymerase chain reaction-restriction fragment length polymorphism technique (PCR–RFLP) was used for genotyping. Anthropometric parameters, lipid and hormonal profiles, were compared between the two groups. Demographic features were compared using Mann Whitney U test while the Chi-square test and odds ratios (ORs) were used to assess the genetic association and risk towards PCOS, respectively. A one-way analysis of variance (ANOVA) test was employed to analyze the correlation of genotypes with baseline parameters in PCOS cases. A statistically significant difference was revealed in the genotypic and allelic frequencies of rs4953616 polymorphism between PCOS cases and controls (p = 0.01 and p = 0.004, respectively). The mutant genotype (TT), mutant allele (T), and recessive model of rs4953616 polymorphism conferred 1.77, 1.3, and 1.5 times risk towards PCOS, respectively. No significant distribution for genotypes and alleles was found for rs7371084 in both groups (p = 0.25 and p = 0.26, respectively). In addition to dyslipidemia, PCOS women also had significantly higher body mass index (BMI) and waist-to-hip ratio (WHR), testosterone (T), and luteinizing hormone (LH). Upon haplotype analysis, the TT haplotype was found to be significantly associated with the increased risk of PCOS. Our results demonstrated a significant role of LHCGR rs4953616 polymorphism in the development of PCOS.
Similar content being viewed by others
Introduction
PCOS is the most prevalent endocrine-metabolic condition in women of fertile age with a global prevalence of 5% to 20%1,2. The variation in the prevalence of PCOS could be due to the heterogeneity in ethnicity and age distribution in the population from which data has been collected3. During the 2003 Rotterdam Consensus Workshop, PCOS was defined as a multi-system matrix of anomalies including obesity, hyperinsulinemia, menstrual irregularities, hyperandrogenism, small cysts in one or both ovaries, and elevated concentrations of LH4. In addition, PCOS has also been linked to impaired glucose tolerance, increased risk of type 2 diabetes, endometrial cancer, cardiovascular diseases, dyslipidemia, and depression which further worsen the quality of life5,6. Several hypotheses have been proposed over time to pinpoint the precise underlying processes that lead to the development of PCOS. However, due to its heterogeneous nature and uncertain etiology, by the time a diagnosis is made, PCOS manifests as a self-perpetuating cycle of multiple system dysfunction7. Family studies and genome-wide association studies (GWAS) have supported the contribution of genetic factors to the pathophysiology of PCOS8,9. The phenotype of PCOS, diagnostic criteria employed, and racial background, all influence the narrowing down of the PCOS susceptibility loci10. However, a few genetic loci that were found to be associated with PCOS development include LHCGR, FSHR, THADA, and DENND1A and the interaction among these loci and multiple proteins under the influence of environmental factors affects PCOS progression11.
The LHCGR is directly involved in the orchestrated series of events that regulate normal sexual maturation and fertility in males and females12. LHCGR acts as a high-affinity receptor for LH and upon binding leads to steroidogenesis, follicular development, and formation of corpus luteum13. The LHCGR belongs to the G-protein coupled receptor family, and in women, is primarily expressed in ovarian theca cells and differentiated granulosa cells14,15. In contrast to theca cells which constitutively express LHCGR, granulosa cells express LHCGR only at the later stages of follicular development after they become fully differentiated. Induction of LHCGR allows the preovulatory follicle to respond to the mid-cycle surge of LH with ovulation13.
The LHCGR gene is mapped on chromosome 2 (2p16.3) comprising 11 exons that code for 675 amino acid trans-membrane glycoprotein16. In GWAS, several polymorphisms in the LHCGR have been reported and these SNPs may alter the gene expression or protein function influencing its biological activity which causes typical features of PCOS in women of reproductive age17,18. The studies that investigated the association of susceptible SNPs across the globe have come up with strong evidence for the association of LHCGR polymorphisms with PCOS despite conflicting results19,20,21,22.
The rs13405728 intronic polymorphism was reported as the most significant and found to be associated with PCOS in Chinese23. However, in European ancestry, rs13405728 was not associated with the risk of PCOS17. Our previous study demonstrated the crucial role of rs2293275 and rs12470652 polymorphisms in the development of PCOS22. A study on Bahraini Arab women was the first to report the association of novel rs4953616 and rs7371084 SNPs with PCOS24. All these inconsistencies in the results of different association studies could be attributed to ethnic disparities and the availability of different diagnostic criteria.
The present study aimed to evaluate the association of LHCGR rs4953616 and rs7371084 polymorphisms with a risk of PCOS in the Punjabi population.
Material and methods
Sample collection and biochemical evaluation
The study was approved by the Ethics Review Board of Guru Nanak Dev University, Amritsar (297/HG) which is in accordance with the Declaration of Helsinki. A total of 823 women were enrolled in the present study, 443 of whom were diagnosed with PCOS and 380 age-matched healthy controls with no signs of PCOS. Women with PCOS were recruited from Beri Maternity Hospital, Amritsar, Punjab, India after the confirmed diagnosis by a gynecologist. Informed consent was obtained from all the participants followed by a withdrawal of 5 mL peripheral blood from each case and control, 3 mL was transferred to a vacutainer containing 0.5 M EDTA for molecular assays and 2 mL was poured into the vacutainer containing clot activator for biochemical analysis. The predesigned proforma was used to collect the relevant information like demographics, reproductive history, family history, and pedigree. The included subjects' anthropometric data including height, weight, WHR, and BMI was also obtained. The inclusion and exclusion criteria for the selection of both groups have been described in our previous study25. The 2 mL blood was used for serum extraction which was then subjected to biochemical analysis including measurements of total cholesterol, high-density lipoprotein (HDL), and triglycerides levels, and specific kits provided by Erba Mannheim were used for the analysis. Friedewald’s formula was used to estimate the proportion of low-density lipoprotein (LDL) and very low-density lipoprotein (VLDL)26. The levels of T, LH, and follicle-stimulating hormone (FSH) were also measured using Calbiotech’s ELISA kits.
DNA extraction and genotyping
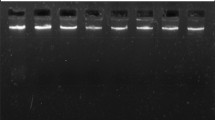
Genomic DNA was isolated from the 3 ml of blood using the phenol–chloroform method27. Nanodrop and agarose gel electrophoresis were used to assess the quality and concentration of isolated DNA. For genotype rs4953616, an amplification refractory mutation system (ARMS) PCR technique was used. Tetra primers (2 outer primers and 2 inner primers) were designed using the Primer 1 software to amplify the target region (http://primer1.soton.ac.uk/primer1.html) and then 1.8% ethidium bromide-stained gel was used to visualize the amplified products. The bands of 406 bp and 185 bp represented the CC homozygous genotype, bands of 406 bp and 268 bp indicated the TT homozygous genotype whereas the bands of 406 bp, 185 bp, and 268 bp signified CT heterozygous genotype. The PCR–RFLP technique was performed to genotype the rs7371084 polymorphism. The amplification was carried out using a specific set of primers which were designed using the Primer 3 tool (https://bioinfo.ut.ee/primer3-0.4.0/) to obtain a 315 bp product followed by restriction digestion using the HaeIII enzyme (New England Biolabs) at 37 °C for 2 h. After that, RFLP products were electrophoresed on 2.2% agarose gel and the band of 315 bp indicated wild-type genotype (TT), bands of 315 bp, 229 bp and 86 bp signified heterozygous genotype (TC) and bands of 229 bp and 86 bp represented homozygous mutant genotype (CC). Details of the primers used for amplification are given in Table 1.
Statistics
The continuous variables were checked for normal distribution using the Kolmogorov test and as variables did not follow normal distribution Mann Whitney test was applied and results were given as median and interquartile range and a p-value less than 0.05 was considered significant. CaTS–Power Calculator was used to evaluate the power of the study and sample size indicating power to be 82.5% with a confidence interval (CI) of 95%. The Hardy–Weinberg equilibrium (HWE) was applied to all the controls for rs4953616 and rs7371084 polymorphisms and it was found that both of the SNPs were significantly following the HWE. The Statistical Package for Social Sciences (version 21, IBM SPSS, NY, USA) was used to analyze the data. The chi-square test was performed to evaluate the significant distributions of genotypic and allelic frequencies of both the SNPs among PCOS cases and controls. To quantify the risk of each polymorphism for the development of PCOS, ORs were calculated using MedCalc software. The biochemical variables, anthropometric features, and hormonal characteristics were compared concerning genotypes by performing an ANOVA test. Haplotype analysis was carried out using Haploview version 4.2 software. Bonferroni correction was adjusted for genetic analysis and ANOVA tests.
Results
Baseline characteristics of the study participants
The median age for PCOS women in this case–control study was 24, whereas 23 for healthy controls as both groups were age-matched, no significant difference was detected. However, in the studied population, women with PCOS appeared to be experiencing early-age menarche as compared to control women (p = 0.03). Dyslipidaemia was associated with PCOS women with significantly elevated cholesterol (p < 0.0001), triglycerides (p < 0.0001), LDL (p = 0.04), and VLDL (p < 0.0001) levels, and lower HDL levels compared to control women (p < 0.0001). The levels of T (p < 0.0001) and LH (p = 0.01) were raised whereas FSH levels were consistent between both cohorts following the hormonal evaluation. BMI and WHR showed significantly higher values in PCOS females (p < 0.0001) (Table 2).
Genotype analysis
The frequency distribution of genotypes and alleles for rs4953616 polymorphism was statistically significantly different among both of the groups (p = 0.01 and p = 0.004, respectively). The carriers of mutant genotype (TT) and mutant allele (T) were at 1.77 (OR: 1.77; CI 1.19 to 2.63; p = 0.004) and 1.3 (OR: 1.3; CI 1.09 to 1.61; p = 0.004) times more risk to develop PCOS, respectively. The recessive model for rs4953616 polymorphism was also revealed to confer a 1.5-fold risk for PCOS progression (p = 0.005). On the contrary, no significant genotypic and allelic frequency distribution was found for rs7371084 in cases and controls (p = 0.25 and p = 0.26, respectively) (Table 3).
Multiple comparisons analysis
The ANOVA test was conducted to evaluate the possible impact of individual genotypes on BMI, WHR, lipid profile, and hormonal parameters of PCOS for both polymorphisms in cases. The study findings indicated a marginal but not significant increase in the levels of triglyceride (p = 0.08), VLDL (p = 0.16) (Table 4), and T (p = 0.16) (Table 5) among women with PCOS who carried the CC genotype of the rs7371084 polymorphism.
Haplotype analysis
The Haploview version 4.2 software was used to analyze the haplotypes of LHCGR rs4953616 and rs7371084 polymorphisms in cases and controls. Both the SNPs appeared to be moderately in linkage disequilibrium (LD) (D′ = 0.498, LOD = 2.86, r2 = 0.016) (Fig. 1). We observed the TT haplotype to be significantly associated with an increased risk of PCOS (OR: 1.40; CI 1.04 to 1.85; p = 0.02) (Table 6).
Discussion
Association studies have always been valuable for determining the putative genetic loci that correlate to disease risk, and the significance of these studies dramatically increased in multifaceted disorders like PCOS where several loci from different pathways are involved in the pathogenesis of the syndrome. By conducting association analyses researchers may accurately narrow down the causal SNPs believed to be linked with the onset or progression of the disease. The present study comprised of 823 women was conducted to evaluate the association of LHCGR rs4953616 and rs7371084 polymorphisms with the risk of PCOS development. In the studied population, women with PCOS experienced early menarcheal age as compared to non-PCOS women (p = 0.015). However, our findings are in disagreement with the studies conducted on Colombian and Bahraini Arab women (p = 0.18 and p = 0.24, respectively)24,28. In this study, we found dyslipidemia to be significantly associated with PCOS cases (p < 0.015). Our findings were supported by study on Chinese women revealing 41.3% of women had dyslipidemia29. Another study from China demonstrated the high prevalence of dyslipidemia to be associated with PCOS women and the most prevailing factor was low HDL levels30. However, our findings are in disagreement with the study from Dubai31. A study from Mardan, Pakistan reported an association of abnormal lipid profiles with anxiety and depression in women with PCOS32. The present study demonstrated higher values of BMI and WHR in PCOS women (p < 0.0001). Our results are in agreement with the study from Madhya Pradesh33 and Maharashtra, India34. On the contrary, a study conducted by Kaluzna et al. on Polish females found no significant difference in WHR between both groups35. A significant association of high BMI in women with PCOS was also documented in the Pakistani population36. Another significant association between high BMI and WHR values and PCOS was reported by a Northeast Indian study37.
Among the hormonal parameters, LH (p = 0.01) and T (p < 0.0001) concentrations were significantly elevated in women with PCOS as compared to controls. We also evaluated the correlation between genotypes of both polymorphisms and hormonal profiles. No significant association was observed between any genotype of rs4953616 and rs7371084 polymorphisms and hormones. This is in contrast with the findings published on Arab women where researchers demonstrated rs4953616 to be negatively associated with T although no association of rs7371084 with hormones (LH, FSH, and T) was observed24. On the contrary, another study illustrated the increased LH levels (p = 0.02) in an overdominant model (TT + CC) of rs7371084 in individuals with PCOS, however, results for rs4953616 were in agreement with our findings28.
Our study found a statistically significant difference in the genotypic (p = 0.01) and allelic frequencies (p = 0.004) for rs4953616 polymorphism upon comparing cases and controls. It was revealed that the mutant genotype (TT) and mutant allele (T) conferred 1.77 (CI 1.19 to 2.63; p = 0.004) and 1.3 (CI 1.09 to 1.61; p = 0.004) folds risk to the PCOS development. We also observed that among the genetic models, the recessive model provided 1.5 (CI 1.14 to 2.16; p = 0.005) times more risk of PCOS (Table 3). Our findings are supported by a study on Bahraini Arab women demonstrating rs4953616 polymorphism to be associated positively with PCOS24. However, the present study is in disagreement with a pilot study conducted on Colombian women28. In contrast, no significant difference in frequency distribution is found for rs7371084 polymorphism. However, Almawi et al. (2015) found a negative association between rs7371084 and PCOS24. Similar findings were delivered by Alarcón-Granados et al. where they reported rs7371084 polymorphism to be linked negatively with PCOS in the dominant, overdominant, and codominant models28.
Both the SNPs were subjected to haplotype analysis which resulted in moderate LD between the two polymorphisms (D′ = 0.498 and r2 = 0.016). A similar trend of LD for rs4953616 and rs7371084 was reported by Almawi et al.24. However, complete LD (D′ = 1) and low recombination (r2 = 0.08) were illustrated in a pilot study on Colombian women28. Our study also revealed a significant difference in the distribution of haplotypes among both cohorts and the occurrence of haplotype TT was found to be associated with an increased risk of PCOS (OR: 1.40; CI 1.04 to 1.85; p = 0.02) (Table 6). These findings were found to be in disagreement with other studies on Bahraini Arab and Colombian women24,28.
Conclusion
The present case–control study demonstrated the association of LHCGR rs4953616 polymorphism with PCOS in the Punjabi population. Genetic association studies have been proven to uncover the potential genes or genomic regions and elucidate novel pathways that make a contribution to certain disease or trait. Further research on larger scale including populations from related or distinct ethnic groups is required to validate the association of LHCGR polymorphisms with PCOS. The data can be utilized to facilitate the advancement of therapeutic interventions, and screening purposes to take preventive measures before onset of disease.
Data availability
The manuscript contains all the data which have been collected and analyzed during the course of this study.
References
Elasam, A. N. et al. The prevalence and phenotypic manifestations of polycystic ovary syndrome (PCOS) among infertile Sudanese women: A cross-sectional study. BMC Womens Health 22, 165 (2022).
Ding, H. et al. Resistance to the insulin and elevated level of androgen: A major cause of polycystic ovary syndrome. Front. Endocrinol. 12, 741764 (2021).
Engmann, L. et al. Racial and ethnic differences in the polycystic ovary syndrome metabolic phenotype. Am. J. Obstet. Gynecol. 216, 493-e1 (2017).
Eshre R, ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Hum. Reprod. 19(41–7), 2004 (2004).
Mao, Z. et al. Identification of epigenetic interactions between microRNA and DNA methylation associated with polycystic ovarian syndrome. J. Hum. Genet. 66, 123–137 (2021).
Hussain, N. Polycystic ovarian syndrome (PCOS), pathophysiological role of a SNP in CYP17 gene and PCOS management by phytoconstituents of food. J. Acad. Fam. Phys. Pak. 14, 56–75 (2022).
Yasmin, A. et al. Polycystic ovary syndrome: An updated overview foregrounding impacts of ethnicities and geographic variations. Life. 12, 1974 (2022).
Chen, Z. J. et al. Genome-wide association study identifies susceptibility loci for polycystic ovary syndrome on chromosome 2p16.3, 2p21 and 9q33.3. Nat. Genet. 43, 55–59 (2011).
Khan, M. J., Ullah, A. & Basit, S. Genetic basis of polycystic ovary syndrome (PCOS): Current perspectives. Appl. Clin. Genet. 12, 249–260 (2019).
Mumusoglu, S. & Yildiz, B. O. Polycystic ovary syndrome phenotypes and prevalence: Differential impact of diagnostic criteria and clinical versus unselected population. Curr. Opin. Endocr. Metab. Res. 12, 66–71 (2020).
El-Shal, A. S., Zidan, H. E., Rashad, N. M., Abdelaziz, A. M. & Harira, M. M. Association between genes encoding components of the leutinizing hormone/luteinizing hormone–choriogonadotrophin receptor pathway and polycystic ovary syndrome in Egyptian women. IUBMB life. 68, 23–36 (2016).
Oduwole, O. O., Huhtaniemi, I. T. & Misrahi, M. The roles of luteinizing hormone, follicle-stimulating hormone and testosterone in spermatogenesis and folliculogenesis revisited. Int. J. Mol. Sci. 22, 12735 (2021).
Shaaban, Z. et al. Decreased expression of arginine-phenylalanine-amide-related peptide-3 gene in dorsomedial hypothalamic nucleus of constant light exposure model of polycystic ovarian syndrome. Int. J. Fertil. Steril. 12, 43 (2018).
Singh, R. & Pathak, A. Gonadotropin Receptor Cross-Talk and Altered Functions in Gonadal and Non-Gonadal Tissues. J Endocrinol Reprod. 27, 169–177 (2023).
Zhang, Z. et al. Novel mutations in LHCGR (luteinizing hormone/choriogonadotropin receptor): Expanding the spectrum of mutations responsible for human empty follicle syndrome. J. Assist. Reprod. Genet. 37, 2861–2868 (2020).
Qiao, J. & Han, B. Diseases caused by mutations in luteinizing hormone/chorionic gonadotropin receptor. Prog. Mol. Biol. Transl. Sci. 161, 69–89 (2019).
Mutharasan, P. et al. Evidence for chromosome 2p16.3 polycystic ovary syndrome susceptibility locus in affected women of European ancestry. J. Clin. Endocrinol. Metab. 98, E185–E190 (2013).
Huhtaniemi, I. & Alevizaki, M. Gonadotrophin resistance. Best Pract. Res. Clin. Endocrinol. Metab. 20, 561–576 (2006).
Themmen, A. P. An update of the pathophysiology of human gonadotrophin subunit and receptor gene mutations and polymorphisms. Reproduction. 130, 263–274 (2005).
Bassiouny, Y. A., Rabie, W. A., Hassan, A. A. & Darwish, R. K. Association of the luteinizing hormone/choriogonadotropin receptor gene polymorphism with polycystic ovary syndrome. Gynecol. Endocrinol. 30, 428–430 (2014).
Ha, L., Shi, Y., Zhao, J., Li, T. & Chen, Z. J. Association study between polycystic ovarian syndrome and the susceptibility genes polymorphisms in Hui Chinese women. PLoS ONE. 10, e0126505 (2015).
Singh, S., Kaur, M., Kaur, R., Beri, A. & Kaur, A. Association analysis of LHCGR variants and polycystic ovary syndrome in Punjab: A case–control approach. BMC Endocr. Disord. 22, 335 (2022).
Cui, L. et al. Genotype–phenotype correlations of PCOS susceptibility SNPs identified by GWAS in a large cohort of Han Chinese women. Hum. Reprod. 28, 538–44 (2013).
Almawi, W. Y. et al. Leutinizing hormone/choriogonadotropin receptor and follicle stimulating hormone receptor gene variants in polycystic ovary syndrome. J. Assist. Reprod. Genet. 32, 607–614 (2015).
Kaur, M., Singh, S., Kaur, R., Beri, A. & Kaur, A. Analyzing the impact of FSHR variants on polycystic ovary syndrome—A case-control study in Punjab. Reprod. Sci. 30, 2563–2572 (2023).
Friedewald, W. T., Levy, R. I. & Fredrickson, D. S. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin. Chem. 18, 499–502 (1972).
Adeli, K. & Ogbonna, G. Rapid purification of human DNA from whole blood for potential application in clinical chemistry laboratories. Clin. Chem. 36, 261–264 (1990).
Alarcón-Granados, M. C., Moreno-Ortiz, H., Rondón-Lagos, M., Camargo-Villalba, G. E. & Forero-Castro, M. Study of LHCGR gene variants in a sample of colombian women with polycystic ovarian syndrome: A pilot study. J. King Saud. Univ. Sci. 34, 102202 (2022).
Luo, X., Cai, W. Y. & Wu, X. K. Prevalence, pattern and predictors for dyslipidemia of Chinese women with polycystic ovary syndrome. Front. Cardiovasc. Med. 8, 790454 (2021).
Guo, F. et al. The lipid profiles in different characteristics of women with PCOS and the interaction between dyslipidemia and metabolic disorder states: A retrospective study in Chinese population. Front. Endocrinol. 13, 892125 (2022).
Khamis, A. H. Prevalence of Dyslipidemia among Women with Polycystic Ovary Syndrome Based on Body Mass Index (2020.).
Habib, R., Rehman, S. U., Zubair, T. & Tariq, M. Association of dyslipidemia with anxiety and depression in patients of polycystic ovarian syndrome. Khyber Med. Univ. J. 13(2), 113–7 (2021).
Yadav, S. & Tarware, R. Waist hip ratio: An anatomical predictive marker of risk of PCOS. Int. J. Reprod. Contracept. Obstet. Gynecol. 8(4), 1630–1633 (2019).
Makhija, N., Tayade, S., Toshniwal, S. & Tilva, H. Clinico-metabolic profile in lean versus obese polycystic ovarian syndrome women. Cureus https://doi.org/10.7759/cureus.37809 (2023).
Kałużna, M. et al. Effect of central obesity and hyperandrogenism on selected inflammatory markers in patients with PCOS: A WHtR-matched case-control study. J. Clin. Med. 9, 3024 (2020).
Rehman, R., Mehmood, M., Ali, R., Shaharyar, S. & Alam, F. Influence of body mass index and polycystic ovarian syndrome on ICSI/IVF treatment outcomes: A study conducted in Pakistani women. Int. J. Reprod. Biomed. 16, 529 (2018).
Pillai, S. S., Phukan, P. K. & Dihingia, P. Significance of body mass index in the classification of PCOS: A comparative study in Northeast India. J. South Asian Fed. Obstet. Gynaecol. 12(3), 145–149 (2020).
Acknowledgements
The authors are grateful to all study participants for their valuable contribution.
Funding
This work was supported by funding from a UGC fellowship to SS and MK and by RUSA 2.0 Component 4 provided to AK.
Author information
Authors and Affiliations
Contributions
The study was designed by A.K. The diagnosis of PCOS was approved by A.B. The collection of samples and execution of experiments were conducted by S.S. and M.K., while the composition of the manuscript was undertaken by S.S. The statistical analysis was performed by S.S. and M.K. The manuscript has been reviewed and accepted by all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Singh, S., Kaur, M., Beri, A. et al. Significance of LHCGR polymorphisms in polycystic ovary syndrome: an association study. Sci Rep 13, 22841 (2023). https://doi.org/10.1038/s41598-023-48881-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-48881-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.