Abstract
Minimally invasive surgery reduces surgical trauma and the size and number of incisions. The da Vinci SP robotic surgical system was designed to overcome the technical demands of single-incision laparoscopic surgery. This study aimed to demonstrate the safety and feasibility of single-port (SP) robotic distal gastrectomy (SPRDG) for patients with gastric cancer using the da Vinci SP system (Intuitive Surgical Inc., Sunnyvale, CA, USA). This study was designed as a single-arm prospective phase I/II clinical trial of SPRDG (first posted date: 21/09/2021, NCT05051670; clinicaltrials.gov). SPRDG using the da Vinci SP system was performed on 19 patients with gastric cancer between December 2021 and October 2022. The primary outcome was the safety of SPRDG as measured by major postoperative complications. The secondary outcomes were operation time, bleeding amount, bowel motility recovery, and length of hospital stay. SPRDG was performed in all 19 patients without unexpected events, such as use of additional trocars or conversion to laparoscopic or open surgery. No major complications occurred postoperatively (0/19, 0.0%). The mean operation time was 218 min (range 164–286 min). The mean hospital stay duration was 3.2 days (range 2–4 days). This phase I/II clinical trial, performed by a single expert surgeon, demonstrated the safety and feasibility of SPRDG with the da Vinci SP system in selected patients with gastric cancer. SPRDG could be a reasonable alternative to conventional or reduced-port minimally invasive gastrectomy, as it has cosmetic advantages, early recovery, and safe discharge.
Similar content being viewed by others
Introduction
Laparoscopic surgery has become an essential surgical option to treat patients with gastric cancer over the past two decades1,2,3,4. Laparoscopic surgery gives better cosmesis and earlier recovery with less postoperative pain than open surgery techniques5,6,7, especially when fewer trocars are used8,9,10. Although surgeons can suffer the limitations of the laparoscopic instrument and the fulcrum effect technically demanding, reduced-port laparoscopic surgery has been developed to minimize the number of trocar insertions11,12,13.
Robotic surgery systems have been widely used to overcome the restrictions of laparoscopic surgery technology14,15,16,17. The robotic systems have also evolved to a single-site platform to provide a reduced-port approach18,19,20. The da Vinci single-port (SP) system (Intuitive Surgical Inc., Sunnyvale, CA, USA) was developed for a more straightforward reduced-port approach21,22,23,24,25,26.
The earlier da Vinci Si and Xi systems (Intuitive Surgical Inc.) also allowed reduced-port surgery using a single-site system. However, less experienced surgeons found the docking to be challenging, which limited the widespread uptake of these systems. Thus, the da Vinci SP system was developed as a single-port-based multichannel cannula that maintains the advantages of conventional robotic surgical systems, such as high-resolution three-dimensional images and wristed anti-tremor action. Therefore, da Vinci SP is a promising system that combines robotic surgery with a reduced-port approach.
This prospective study aimed to confirm the applicability of reduced-port distal gastrectomy using the da Vinci SP system in patients with gastric cancer. We used surgical outcomes and early complication rates to assess the safety and feasibility of da Vinci SP robotic distal gastrectomy (SPRDG). Furthermore, we describe our initial experiences and surgical techniques to increase the potential application of the da Vinci SP robotic system.
Methods
Patients and study design
This clinical trial was a single-arm prospective phase I/II study conducted at a single institution, performed by a single surgeon with vast experience in both laparoscopic and robotic gastrectomy. We enrolled 19 patients with gastric cancer scheduled for robotic distal gastrectomy from December 2021 to October 2022. The first patient was enrolled on 16/12/2021 (SP-01). The inclusion criteria were a biopsy-confirmed adenocarcinoma of the stomach scheduled to undergo radical gastrectomy, age between 20 and 80 years, American Society of Anesthesiologists (ASA) physical status classification system class I–III, and signed informed consent after a thorough explanation of the study. The exclusion criteria were patients with distant metastasis, candidate for endoscopic mucosal resection, complicated gastric cancer (obstruction or perforation), another active primary tumor, and vulnerable subject (illiterate or pregnant). Patient characteristics, surgical factors, and pathology results of enrolled patients were prospectively collected. Informed consent was obtained from all patients after providing sufficient information about gastrectomy using the da Vinci SP robotic system. This phase I/II single-arm study was approved by the Institutional Review Board of Severance Hospital, Yonsei University Health System (4-2021-0881) and was conducted in compliance with the ethical guidelines of the Helsinki Declaration of 1975. The study protocol was registered at clinicaltrials.gov (first posted date: 21/09/2021, NCT05051670). All methods were performed in accordance with the relevant guidelines and regulations.
Da Vinci SP system
Like the previous da Vinci Xi system, the da Vinci SP system consists of the surgeon console, patient cart, and vision cart21,27,28,29. The da Vinci SP system enables multiple flexible instruments to be docked in a single port, permitting surgeries to be conducted through smaller incisions with fewer ports. Additionally, four multiarticulated instruments and a three-dimensional camera can be inserted through a 25 mm multichannel cannula. The da Vinci SP system provides high-resolution three-dimensional surgical views and sophisticated full-wristed movements that minimize tremors, similar to the da Vinci Xi system. In addition, the newly added joint in the da Vinci SP system instrument acts like an elbow to enhance surgical access within the narrow multichannel cannula, thereby providing a broader working space for surgeons. Using the SP approach, surgeons can manipulate the multiarticulated instruments with a similar sense of control as that of conventional robotic surgery.
Settings and preparation for da Vinci SP robotic distal gastrectomy
Supplementary Figure S1 shows a schematic illustration of the instrument setup. Figure 1 demonstrates the preparation process for patient positioning and robotic system docking for SPRDG. The patient was placed in the lithotomy position for SPRDG (Fig. 1a). A Pfannenstiel incision of about 3.5 cm in length was made to create a pathway for the multichannel cannula instead of the conventional periumbilical midline incision (Fig. 1b). After pneumoperitoneum formation, a 15-degree reverse Trendelenburg position was set, and one additional 12 mm assist trocar was inserted into the patient’s right or left lower quadrant, depending on the reconstruction plan (Fig. 1c). Afterward, the patient cart from the caudal side and the multichannel cannula were docked to the da Vinci SP robotic system. A camera and three full-jointed instruments (arm 1: scissors capable of monopolar electrocauterization; arm 2: a Cadiere atraumatic forcep; and arm 3: Maryland forceps capable of bipolar electrocauterization) were docked through the single-port da Vinci SP cannula (Part number 430004, Part number 430010, and Part number 430009, respectively; Intuitive Surgical Inc.) and used during surgery. The additional assist trocar was used to transfer gauze and needles and to facilitate using the ultrasonic device Sonicision (Medtronic, Minneapolis, MN, USA) for tissue dissection during the surgery; linear stapling for anastomosis or transection using Signia (Medtronic); and vessel clipping. Figure 1d shows the initial landscape of the patient side view after the docking is complete.
Setting up for da Vinci SP robotic distal gastrectomy (SPRDG). (a) Patient in lithotomy and 15-degree reverse Trendelenburg position; (b) Pfannenstiel incision for (c) multichannel cannula docking and multichannel cannular insertion, with additional assist trocar placement also shown; (d) patient-side preparation after the completion of docking for SPRDG.
Surgical procedure
All surgical procedures followed the gastric cancer surgery guidelines3,30. According to the Korean Practice Guideline for Gastric Cancer, D1 + lymphadenectomy was performed for early gastric cancer patients with any suspicion of LN metastasis, and D2 lymphadenectomy was performed for patients with suspicion of LN metastasis or advanced gastric cancer3. Dissection of the lymph nodes was performed while retracting tissue using Cadiere forceps in arm 2. The scissors in arm 1 and Maryland forceps in arm 3 were used for lymph node dissection (Fig. 2a). The duodenum was transected using a surgical stapler through the assist port (Fig. 2b). The cannula was rotated as needed to visualize the suprapancreatic area (Fig. 2c,d). After liver traction, suprapancreatic area lymph node dissection was performed using monopolar scissors and Maryland forceps. Then, the stomach resection was performed using a linear stapler. The stomach specimen was retrieved through the primary Pfannenstiel incision. After confirming the tumor location and margin length, reconstruction by intracorporeal delta-shaped gastroduodenostomy (Fig. 2e) or gastrojejunostomy (Fig. 2f) was performed as previously described31. The closure of the Pfannenstiel incision commenced with peritoneal closure using an absorbable purse-string suture. The rectus muscle was approximated with no suturing. The transversalis fascia was closed using barbed suture material with a continuous suture technique. Finally, the skin was approximated with vertical mattress sutures with a skin stapler (Fig. 3a).
Intraoperative surgical view of SPRDG. (a) Instrument positioning, tissue traction, and dissection; (b) a linear stapler for duodenal transection through the assist trocar; (c) camera placement positioned below till the completion of station #6; (d) after duodenal transection, all instruments were rotated 180 degrees and the camera was positioned above for suprapancreatic lymph node dissection; (e) intracorporeal delta-shaped gastroduodenostomy stapled via trocars located on the patient’s left side; (2f.) gastrojejunostomy stapled via trocars located on the patient’s right side.
Postoperative management
All 19 patients who underwent SPRDG were treated with the same postoperative protocol as patients who undergo minimally invasive distal gastrectomy. In managing postoperative pain, every patient in this study was provided with IV PCA (Intravenous Patient-Controlled Analgesia). Additionally, a drainage tube was routinely placed in all patients after the procedure. According to the enhanced recovery after surgery protocol, patients were allowed sips of water from the evening of the operation day32. Regardless of gas passing, a liquid diet was followed from the morning of the first postoperative day, followed by a soft diet at noon and evening. If there were no specific complications until postoperative day 3, discharge was encouraged if the patient’s condition satisfied the previously reported safe discharge criteria33.
Outcome measurement
The primary endpoint of this phase I/II SPRDG clinical trial was the 30-day major complication rate. Any further prescribed drugs, laboratory or image examinations performed on patients and treatment courses were reviewed. Any complications requiring outpatient clinic attendance, rehospitalization, or unexpected hospital visits within 30 days were observed. Whether complications developed or not was confirmed through a weekly quality control meeting as previously described34. Additionally, secondary endpoints of this single-arm study were operation time, bleeding amount, bowel motility recovery, and length of hospital stay.
Statistical analysis
According to a previous report of complications of robotic subtotal gastrectomy, we set the threshold margin of the complication rate to 15%17,35. A single-stage single-arm phase II clinical trial design was used to test the null hypothesis that the complication rate was more than or equal to 15% and the alternative hypothesis that the complication rate was less than or equal to 4%. The required sample size was estimated to be 19 cases based on a significance level of 0.2 and a power level of 0.7. If the count of verified complications was equal to or less than two, the null hypothesis may be rejected. The sample size was calculated using the R package clinfun (Clinical Trial Design and Data Analysis Functions; R Foundation for Statistical Computing, Vienna, Austria). Categorical variables are reported as numbers and percentages, and continuous variables are reported as means and ranges. We calculated the complication rate estimate and its 80% confidence interval. All analyses were conducted using R software (version 4.1.0; R Foundation for Statistical Computing).
Ethical statement
Informed consent was obtained from all patients after providing sufficient information about gastrectomy using the da Vinci SP robotic system. This phase I/II single-arm study was approved by the Institutional Review Board of Severance Hospital, Yonsei University Health System (4-2021-0881). The study protocol was registered at clinicaltrials.gov (NCT05051670).
Results
The basic characteristics of the 19 patients who participated in the clinical trial are given in Table 1. The mean age of the patients was 54.7 years (range 35–70 years), and nine (47.4%, 9/19) were male. The entire surgical process of SPRDG using the da Vinci SP system was feasible and was successfully performed in all 19 patients. There were no technical problems with instrument docking or movement. No patient needed conversion to laparoscopic or open surgery or additional trocar insertion other than the initially planned assist port. Also, D2 lymph node dissection was successfully performed in three patients. Six patients underwent delta-shaped Billroth I gastroduodenostomy, and the other thirteen patients underwent Billroth II gastrojejunostomy.
Perioperative outcome
Table 2 summarizes the outcome of SPRDG in 19 patients. In all 19 patients, a soft diet was possible at maximum 2 days after surgery, and gas passing was confirmed as evidence of bowel movement recovery after a mean of 2.1 days (range 1–3 days). According to the discharge criteria protocol33, all patients were discharged after a mean of 3.2 days (range 2–4 days) of postoperative hospital stay. There were no early postoperative major complications of Clavien-Dindo classification grade III or higher. The major complication rate was 0% (0/19), and the overall complication rate was 26.3% (5/19). Among the reported postoperative complications, two patients experienced postoperative fever and were treated with either antipyretics or antibiotics. Two others faced postoperative urinary retention. Chylous ascites developed in one patient treated with a low-fat diet and orlistat, but no rehospitalization or unscheduled hospital visit occurred on follow-up to 30 days postsurgery.
The postoperative wound after SPRDG
The Pfannenstiel incision was used to maximize the advantage of a wide working space from small incisions that the da Vinci SP system offers, instead of the transumbilical incision used in conventional laparoscopic or robotic gastrectomy. The da Vinci SP system’s multiarticulated instrument and camera view allowed distal gastrectomy to be conducted through the Pfannenstiel incision without approach or vision problems. A representative example of an immediate postoperative wound is shown in Fig. 3a, and the wound 2 weeks after the healing process is shown in Fig. 3b. From a cosmesis standpoint, only a minimal wound that can be hidden by pubic hair or underwear remained.
Discussion
In this study, we reported da Vinci SPRDG could be safely performed without major complications in patients with gastric cancer. All 19 patients were discharged within 4 days after surgery. Among them, fourteen patients completed their hospital stay within 3 days, and no patients had an unscheduled hospital visit within 30 days postsurgery.
We selected the Pfannenstiel incision for multichannel cannula insertion and specimen retrieval. Classically, the Pfannenstiel incision is favored for colorectal and gynecologic surgery because it has lower incisional hernia incidence and less postoperative pain36,37,38,39,40,41,42,43. For gastric cancer surgery, surgeons usually prefer a periumbilical midline incision (Fig. 4a). In conventional laparoscopic or robotic gastrectomy, including the da Vinci Xi system, a rigid robotic camera usually cannot provide an appropriate surgical view through a Pfannenstiel incision (Fig. 4b). The exposure of an accurate surgical field with anatomic landmarks is difficult in conventional robotic gastrectomy, especially when dissecting the suprapancreatic area.
Schematic illustration of robotic gastrectomy. (a) Camera view range of conventional robotic gastrectomy or laparoscopic gastrectomy through a periumbilical midline incision with a rigid 30-degree camera; (b) imaginary camera view range through a Pfannenstiel incision with a rigid 30-degree scope; (c) camera view range of da Vinci SP robotic gastrectomy through a Pfannenstiel incision with an articulated camera.
The camera of the da Vinci SP robotic system is multijointed and includes an elbow joint, so that the surgical area in the upper abdomen is sufficiently accessed and visualized through the Pfannenstiel approach (Fig. 4c). Herein, in this prospective study, a Pfannenstiel approach in the lithotomy position was chosen for use with the new technology of the da Vinci SP system. The advantages of a Pfannenstiel incision over conventional techniques, including lower incisional hernia rate, less postoperative pain, and better cosmetic effect, are expected to maximize the benefits of this minimally invasive surgery.
Since the introduction of minimally invasive surgery, surgeons have been trying to perform surgically and oncologically safe operations with less trauma. Instruments and imaging systems have been developed to enable comparable or even better dissection quality than conventional surgery with a smaller incision. If surgery can be conducted safely with fewer trocars, then the use of fewer trocars would reduce surgical trauma and consequent adverse effects. Indeed, this phase I/II clinical trial demonstrated that SPRDG through a Pfannenstiel incision using the da Vinci SP system could be a feasible and safe option for gastric cancer surgery.
Single-incision surgery and natural orifice transluminal endoscopic surgery are attractive not only because of lower surgical trauma but also because of reduced scarring. Of course, surgical and oncological safety must first be established. So, if the safety of the operation is qualified, the cosmetic satisfaction from small scars could be valuable for selective patients. This study’s patients had low transverse abdominal wounds that can be covered by underwear. Thus, SPRDG is expected to be a safe surgical option for patients for whom cosmesis is an important factor.
To the best of our knowledge, this study is the first report on the clinical experience of the da Vinci SP system with SPRDG. There was no conversion to other surgical techniques, additional trocar insertion, or grade III or higher major postoperative complications or readmission events in the 19 patients, demonstrating the feasibility and safety of the SP robotic system for distal gastrectomy. However, the use of the Pfannenstiel incision might affect early recovery and good cosmesis. Our procedure could be a valid option for selected patients with the potential for less postoperative pain, lower possibility of incisional hernia, and better cosmesis than standard surgical techniques.
There are several limitations to this study. First, as this was a single-arm study, we could not compare SPRDG with conventional robotic distal gastrectomy or laparoscopic distal gastrectomy, so comparative studies should be conducted to determine if SPRDG has advantages in terms of incisional hernia incidence, postoperative pain or cosmesis satisfaction. Second, we did not assess long-term patient outcomes in this study, which will be important to measure, considering that the most critical factor in radical cancer surgery is oncological safety. Third, although our study was prospective, the primary purpose was to confirm the safety of SPRDG, so there might be selection bias. Additional real-world studies may be needed in patients with challenging conditions such as high body mass index or advanced gastric cancer. Additionally, this study was conducted by a single expert surgeon with various experiences in laparoscopic and robotic gastrectomy. Whether this is generally accepted requires further research. Last, SPRDG procedure described in this manuscript was developed for initial cases, and methods are continuously evolving and undergoing modifications. For instance, we recently used bipolar dissectors in both hands rather than monopolar scissors in the left hand and a bipolar dissector in the right hand. The pursuit of optimizing surgical techniques is ongoing, and the surgical details discussed here may change with increased use of SPRDG.
Conclusion
This phase I/II clinical trial, performed by a single expert surgeon, demonstrated the safety and feasibility of SPRDG in selected patients. SPRDG could be a reasonable alternative to conventional or reduced-port minimally invasive gastrectomy, with cosmetic advantages, early recovery, and safe discharge.
Data availability
Hyoung-Il Kim had full access to all data in the study and took responsibility for the integrity of the data and the accuracy of data analysis.
References
Hyung, W. J. et al. Long-term outcomes of laparoscopic distal gastrectomy for locally advanced gastric cancer: The KLASS-02-RCT randomized clinical trial. J. Clin. Oncol. 38, 3304–3313. https://doi.org/10.1200/jco.20.01210 (2020).
Japanese Gastric Cancer, A. Japanese Gastric Cancer Treatment Guidelines 2021 (6th edition). Gastric Cancer 26(1–25), 2023. https://doi.org/10.1007/s10120-022-01331-8 (2021).
Kim, T. H. et al. Korean practice guidelines for gastric cancer 2022: An evidence-based, multidisciplinary approach. J. Gastric Cancer 23, 3–106. https://doi.org/10.5230/jgc.2023.23.e11 (2023).
Kitano, S. et al. A randomized controlled trial comparing open vs laparoscopy-assisted distal gastrectomy for the treatment of early gastric cancer: An interim report. Surgery 131, S306-311. https://doi.org/10.1067/msy.2002.120115 (2002).
Son, T. & Hyung, W. J. Laparoscopic gastric cancer surgery: Current evidence and future perspectives. World J. Gastroenterol. 22, 727–735. https://doi.org/10.3748/wjg.v22.i2.727 (2016).
Kelly, K. J. et al. Laparoscopic versus open gastrectomy for gastric adenocarcinoma in the west: A case-control study. Ann. Surg. Oncol. 22, 3590–3596. https://doi.org/10.1245/s10434-015-4381-y (2015).
Kim, Y. W. et al. Improved quality of life outcomes after laparoscopy-assisted distal gastrectomy for early gastric cancer: Results of a prospective randomized clinical trial. Ann. Surg. 248, 721–727. https://doi.org/10.1097/SLA.0b013e318185e62e (2008).
Pan, M. X. et al. Single-incision vs three-port laparoscopic cholecystectomy: Prospective randomized study. World J. Gastroenterol. 19, 394–398. https://doi.org/10.3748/wjg.v19.i3.394 (2013).
Kim, T. J. et al. Does single-port access (SPA) laparoscopy mean reduced pain? A retrospective cohort analysis between SPA and conventional laparoscopy. Eur. J. Obstet. Gynecol. Reprod. Biol. 162, 71–74. https://doi.org/10.1016/j.ejogrb.2012.01.007 (2012).
Wong, J. S. et al. Comparison of postoperative pain between single-incision laparoscopic cholecystectomy and conventional laparoscopic cholecystectomy: Prospective case-control study. Surg. Laparosc. Endosc. Percutan. Tech. 22, 25–28. https://doi.org/10.1097/SLE.0b013e318242ea44 (2012).
Kang, D. Y., Kim, H. G. & Kim, D. Y. Reduced-port laparoscopic distal gastrectomy in obese gastric cancer patients. PLoS ONE 16, e0255855. https://doi.org/10.1371/journal.pone.0255855 (2021).
Lee, H. H. et al. Long-Term oncological outcomes of reduced three-port laparoscopic gastrectomy for early-stage gastric carcinoma: A retrospective large-scale multi-institutional study. J. Gastric Cancer 21, 93–102. https://doi.org/10.5230/jgc.2021.21.e8 (2021).
Kim, K. H. et al. Actual 3-year survival after reduced-port laparoscopic distal gastrectomy for gastric cancer (RpLDG): A propensity score matching analysis. J. Gastrointest. Surg. 26, 550–557. https://doi.org/10.1007/s11605-021-05097-9 (2022).
Noshiro, H., Ikeda, O. & Urata, M. Robotically-enhanced surgical anatomy enables surgeons to perform distal gastrectomy for gastric cancer using electric cautery devices alone. Surg. Endosc. 28, 1180–1187. https://doi.org/10.1007/s00464-013-3304-x (2014).
Han, D. S. et al. Comparison of surgical outcomes of robot-assisted and laparoscopy-assisted pylorus-preserving gastrectomy for gastric cancer: A propensity score matching analysis. Ann. Surg. Oncol. 22, 2323–2328. https://doi.org/10.1245/s10434-014-4204-6 (2015).
Okumura, N. et al. Robotic gastrectomy for elderly gastric cancer patients: Comparisons with robotic gastrectomy in younger patients and laparoscopic gastrectomy in the elderly. Gastric Cancer 19, 1125–1134. https://doi.org/10.1007/s10120-015-0560-6 (2016).
Choi, S. et al. Surgical merits of open, laparoscopic, and robotic gastrectomy techniques with D2 lymphadenectomy in obese patients with gastric cancer. Ann. Surg. Oncol. 28, 7051–7060. https://doi.org/10.1245/s10434-021-09952-6 (2021).
Roh, C. K. et al. Comparison of surgical outcomes between integrated robotic and conventional laparoscopic surgery for distal gastrectomy: A propensity score matching analysis. Sci. Rep. 10, 485 (2020).
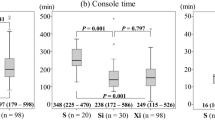
Seo, W. J. et al. Reduced-port totally robotic distal subtotal gastrectomy for gastric cancer: 100 consecutive cases in comparison with conventional robotic and laparoscopic distal subtotal gastrectomy. Sci. Rep. 10, 16015. https://doi.org/10.1038/s41598-020-73118-9 (2020).
Won, S. et al. Robotic single-site plus two-port myomectomy versus conventional robotic multi-port myomectomy: A propensity score matching analysis. J. Pers. Med. 12, 928. https://doi.org/10.3390/jpm12060928 (2022).
Bianco, F. M. et al. Robotic single-port surgery: Preliminary experience in general surgery. Int. J. Med. Robot. 18, e2453. https://doi.org/10.1002/rcs.2453 (2022).
Choi, Y. J., Jo, H. S., Kim, D. S. & Yu, Y. D. Single-port robot plus one port (SP + 1) distal pancreatectomy using the new da Vinci SP system. Langenbecks Arch. Surg. 407, 1271–1276. https://doi.org/10.1007/s00423-022-02477-w (2022).
Lee, I. A. et al. Robotic adrenalectomy using the da Vinci SP robotic system: Technical feasibility comparison with single-port access using the da Vinci multi-arm robotic system. Ann. Surg. Oncol. 29, 3085–3092. https://doi.org/10.1245/s10434-021-11208-2 (2022).
Park, Y. M. et al. Gasless transoral robotic thyroidectomy using the DaVinci SP system: Feasibility, safety, and operative technique. Oral Oncol. 95, 136–142. https://doi.org/10.1016/j.oraloncology.2019.06.003 (2019).
Marks, J. H. et al. SP rTaTME: Initial clinical experience with single-port robotic transanal total mesorectal excision (SP rTaTME). Tech. Coloproctol. 25, 721–726. https://doi.org/10.1007/s10151-021-02449-0 (2021).
Shukla, D., Small, A., Mehrazin, R. & Palese, M. Single-port robotic-assisted partial nephrectomy: Initial clinical experience and lessons learned for successful outcomes. J. Robot. Surg. 15, 293–298. https://doi.org/10.1007/s11701-020-01106-2 (2021).
Kim, J. E. et al. Single-port robotic radical prostatectomy: Short-term outcomes and learning curve. J. Endourol. 36, 1285–1289. https://doi.org/10.1089/end.2021.0885 (2022).
Kim, J. K. et al. Single-port transaxillary robotic thyroidectomy (START): 200-cases with two-step retraction method. Surg. Endosc. 36, 2688–2696. https://doi.org/10.1007/s00464-021-08837-9 (2022).
Kwak, Y. H. et al. Da Vinci SP single-port robotic surgery in gynecologic tumors: Single surgeon’s initial experience with 100 cases. Yonsei Med. J. 63, 179–186. https://doi.org/10.3349/ymj.2022.63.2.179 (2022).
Japanese Gastric Cancer Association. Japanese Gastric Cancer Treatment Guidelines 2021 (6th edition). Gastric Cancer 26(1–25), 2023. https://doi.org/10.1007/s10120-022-01331-8 (2021).
Lee, J. H. et al. Intracorporeal delta-shaped gastroduodenostomy in reduced-port robotic distal subtotal gastrectomy: Technical aspects and short-term outcomes. Surg. Endosc. 32, 4344–4350. https://doi.org/10.1007/s00464-018-6244-7 (2018).
Mortensen, K. et al. Consensus guidelines for enhanced recovery after gastrectomy: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Br. J. Surg. 101, 1209–1229. https://doi.org/10.1002/bjs.9582 (2014).
Guner, A. et al. Safe discharge criteria after curative gastrectomy for gastric cancer. J. Gastric Cancer 22, 395–407. https://doi.org/10.5230/jgc.2022.22.e32 (2022).
Park, S. H. et al. Changes in failure to rescue after gastrectomy at a large-volume center with a 16-year experience in Korea. Sci. Rep. 13, 5252. https://doi.org/10.1038/s41598-023-32593-6 (2023).
Kim, H. I. et al. Multicenter prospective comparative study of robotic versus laparoscopic gastrectomy for gastric adenocarcinoma. Ann. Surg. 263, 103–109. https://doi.org/10.1097/sla.0000000000001249 (2016).
Fiorentini, G. et al. Correlation between type of retrieval incision and postoperative outcomes in laparoscopic liver surgery: A critical assessment. J. Laparoendosc. Adv. Surg. Tech. A 31, 423–432. https://doi.org/10.1089/lap.2020.0470 (2021).
Seong Tan, P. C., Nik Mohamad, N. A. & Gan, S. H. Factors that influence pain intensity and fentanyl requirements after a gynecologic laparotomy. Pain Manag. Nurs. 14, 102–109. https://doi.org/10.1016/j.pmn.2010.12.004 (2013).
Lee, L. et al. Incidence of incisional hernia in the specimen extraction site for laparoscopic colorectal surgery: Systematic review and meta-analysis. Surg. Endosc. 31, 5083–5093. https://doi.org/10.1007/s00464-017-5573-2 (2017).
Tisdale, B. E., Kapoor, A., Hussain, A., Piercey, K. & Whelan, J. P. Intact specimen extraction in laparoscopic nephrectomy procedures: Pfannenstiel versus expanded port site incisions. Urology 69, 241–244. https://doi.org/10.1016/j.urology.2006.09.061 (2007).
Amer, T. et al. Laparoscopic nephrectomy—Pfannenstiel or expanded port site specimen extraction: A systematic review and meta-analysis. Cent. Eur. J. Urol. 68, 322–329. https://doi.org/10.5173/ceju.2015.550 (2015).
Greene, A. K., Michetti, P., Peppercorn, M. A. & Hodin, R. A. Laparoscopically assisted ileocolectomy for Crohn’s disease through a pfannenstiel incision. Am. J. Surg. 180, 238–240. https://doi.org/10.1016/s0002-9610(00)00473-6 (2000).
Luijendijk, R. W. et al. The low transverse Pfannenstiel incision and the prevalence of incisional hernia and nerve entrapment. Ann. Surg. 225, 365–369. https://doi.org/10.1097/00000658-199704000-00004 (1997).
Takagi, K. et al. Role of the pfannenstiel incision in robotic hepato-pancreato-biliary surgery. J. Clin. Med. 12, 1971. https://doi.org/10.3390/jcm12051971 (2023).
Acknowledgements
This trial was supported by an Intuitive Foundation Clinical Research Grant and the Korea Health Technology R&D Project grant through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI22C0767). The authors declare no conflicts of interest. The funding source had no role in the design or conduct of the study; collection, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication. We acknowledge the assistance of Bioscience Writers, LLC (Houston, TX, USA) with editing and correction of English language usage. Statistical consultation for this research was received from the Biostatistics Collaboration Unit (BCU) at the Yonsei University College of Medicine (Seoul, Korea).
Author information
Authors and Affiliations
Contributions
S.H.P. and H.-I.K. had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: S.H.P. and H.-I.K. Acquisition of data: S.H.P., J.H., and K.-Y.K. Analysis and interpretation of data: S.H.P., M.C., Y.M.K., and W.J.H. Drafting of the manuscript: S.H.P. and H.-I.K. Critical revision of the manuscript for import intellectual content: H.-I.K. Statistical analysis: S.H.P., Y.N.K., and J.H. Administrative, technical, or material support: M.C., Y.M.K., and W.J.H. Obtaining funding: H.-I.K. Study supervision: W.J.H. and H.-I.K. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Park, S.H., Kim, Y.N., Hwang, J. et al. Safety and feasibility of reduced-port robotic distal gastrectomy for gastric cancer: a phase I/II clinical trial using the da Vinci Single Port(SP) robotic system. Sci Rep 13, 18578 (2023). https://doi.org/10.1038/s41598-023-45655-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-45655-6
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.