Abstract
Although uncovered self-expandable metal stents (SEMSs) possess certain advantages such as averting cystic duct obstruction and stent migration, they are susceptible to ingrowth occlusion. The combination of the double bare stent (DBS) and endobiliary radiofrequency ablation (RFA) may reduce ingrowth. Hence, this study aimed to examine the utility of this method for the treatment of unresectable malignant distal biliary obstruction (MDBO). This prospective, single-center, pilot study enrolled 51 patients who met the eligibility criteria between February 2020 and January 2022. The study outcomes included technical success, clinical success, recurrent biliary obstruction (RBO), and other adverse events (AE) besides RBO associated with DBS placement with RFA for MDBO. The technical success rate was 98.0% (50/51). Clinical success was achieved in all patients in whom technical success was achieved. The rates of early and late AEs were 5.9% (3/51) and 8.0% (4/50), respectively. The incidence rate of RBO was 38.0% (19/50). Sludge occlusion, ingrowth occlusion, and overgrowth occlusion occurred in 26.0% (13/50), 8.0% (4/50), and 2.0% (1/50) of patients, respectively (the main cause of RBO was undeterminable in 1 patient). The median time to RBO was 241 days. DBS with RFA showed good technical feasibility, good long-term outcomes, acceptable AE rates, and most importantly, a low ingrowth occlusion rate when employed for the treatment of MDBO.
Similar content being viewed by others
Introduction
Endoscopic self-expandable metal stent (SEMS) deployment is recommended for unresectable malignant distal biliary obstruction (MDBO) because it offers a longer patency period compared to plastic stent placement1. The SEMS can be categorized into the uncovered SEMS and covered SEMS2, each of which has advantages and disadvantages; however, the superiority of one system over the other remains inconclusive1,3,4. In the current scenario, the prevalence of recurrent biliary obstruction (RBO) is relatively high, irrespective of the type of stent used, owing to the advancement in antitumor therapy. Recently, a uniquely structured SEMS, which is constructed by the cross-overlapping of two uncovered SEMS called the “double bare stent (DBS),” has been developed with the aim to extend the patency period even further5. This unique SEMS is expected to reduce ingrowth, which is a major cause of uncovered SEMS occlusion, by reducing the size of the stent cells.
On the other hand, endobiliary radiofrequency ablation (RFA), which has been reported to prolong the patency period, has recently emerged as an adjuvant procedure during biliary stent placement6. It is assumed that RFA can reduce ingrowth by inducing coagulative necrosis of the tumor tissue in the strictures. Therefore, the combination of DBS and RFA may further prevent ingrowth, which prolongs patency, while retaining the advantages of the uncovered SEMS. This study aimed to examine the feasibility and utility of this combination treatment with DBS and RFA in patients with MDBO.
Methods
Study design and population
This prospective, single-center, pilot study included consecutive patients aged 20 years or older who developed obstructive jaundice and/or cholangitis due to unresectable MDBO between February 2020 and January 2022. The exclusion criteria were as follows: difficulty in reaching the duodenal papilla, surgically altered gastrointestinal anatomy, short stricture length unsuitable for the RFA catheter used in the study7, Eastern Cooperative Oncology Group performance status 4, severe dysfunction in any other organ, and refusal to participate in the study. Temporary predrainage was implemented with a plastic stent or nasobiliary drainage until the presence of a malignancy and unresectability, such as metastasis, locally advanced, and/or poor general condition were confirmed.
The institutional review board of Aichi Medical University Hospital approved this study, which was conducted in accordance with the principles of the Declaration of Helsinki (approval number: 2019-169). All patients provided written informed consent before the procedure and study participation. The study protocol was registered with the University Hospital Medical Information Network Clinical Trial Registry database (Identifier: UMIN000039563).
Devices
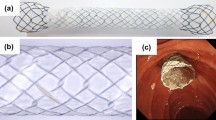
The EGIS biliary DBS (S&G Biotech, Seoul, Korea) and the Habib EndoHPB catheter (Boston Scientific, Marlborough, MA, USA) were used for the biliary drainage procedure in this study (Fig. 1). The DBS is composed of two cross-overlapping standard uncovered stents. The overlap creates smaller stent cells and generates sufficient radial force. A 10-mm diameter stent was used for all cases, and the stent length was chosen according to the stricture length. The Habib bipolar catheter is composed of two 8-mm ring electrodes placed 8-mm apart at the catheter tip. The tissues surrounding the catheter are ablated when the electrodes come into proper contact with the stricture.
The structure of the EGIS biliary double bare stent (S&G Biotech, Seoul, Korea) is composed of two cross-overlapping standard uncovered stents, which can reduce the cell size and ensure sufficient radial force (A,B). The Habib EndoHPB catheter (Boston Scientific, Marlborough, MA, USA) is a bipolar catheter specializing in endobiliary radiofrequency ablation with two 8-mm ring electrodes placed 8-mm apart at the catheter tip (C).
Procedure
The procedure was performed in the prone position under conscious sedation using midazolam with pethidine. A standard side-viewing duodenoscope (Olympus Medical Systems, Tokyo, Japan) was inserted into the duodenum. Biliary cannulation and cholangiography were performed, followed by insertion of the Habib catheter over the guidewire, which was positioned with the electrodes in contact with the stricture site. Subsequently, the stricture was ablated at a power of 7–10 W for 90 s using a VIO300D generator (ERBE Elektromedizin GmbH, Tübingen, Germany). RFA application was repeated until the entire stricture was ablated, if the length of the stricture was greater than the scope of ablation with a single application. After ablation, the bile duct was cleaned sufficiently with a retrieval balloon and/or basket catheter. Finally, the DBS was inserted and deployed to cover the stricture (Fig. 2 and Video 1). Endoscopic sphincterotomy was performed in all cases.
In the event of RBO, transpapillary reintervention was attempted initially. First, the inner aspects of the DBS and bile duct were swept sufficiently with a retrieval balloon catheter. If recanalization was good, the primary reason for RBO was judged to be sludge formation, and the procedure was completed using balloon cleaning alone. If good recanalization could not be obtained after balloon cleaning, the primary reason for RBO was judged to be ingrowth with/without overgrowth (persistent stricture located within the stent was ingrowth, and persistent stricture located below or above the stent was overgrowth), and additional stent placement was performed with/without RFA.
An endoscopist who was experienced in biliary stenting and endobiliary RFA procedures conducted or directly supervised all procedures, including initial stenting and reintervention.
Follow-up
All patients were followed-up after the procedure using clinical examinations and laboratory tests at least once every 4 weeks until death or transfer to another institution. Imaging studies, including computed tomography, were performed when adverse events (AE), including RBO, were suspected. Computed tomography was conducted every 2–3 months to evaluate disease progression in patients who underwent chemotherapy, even in those without suspected AEs.
Outcomes and definitions
The study outcomes included technical success, clinical success, RBO, and other AEs besides RBO that were associated with DBS placement with RFA for MDBO.
Technical success was defined as the successful completion of biliary cannulation, RFA catheter insertion, stricture ablation, and DBS placement. Clinical success was defined as the decrease in bilirubin and liver enzyme levels to normal or < 50% of preoperative levels within 14 days. RBO was defined as the recurrence of jaundice and/or cholangitis accompanied by biliary dilation on imaging studies8. The time to RBO was defined as the period from the date of DBS placement with RFA to the date of occurrence of RBO. AEs (except RBO) were defined and graded according to the criteria provided by the American Society for Gastrointestinal Endoscopy9.
Statistical analysis
Categorical variables were expressed as numbers and percentages, and continuous variables were expressed as means and standard deviation (SD). The Kaplan–Meier method was used to estimate the time to RBO. The data of patients who did not develop RBO until the time of death, transfer to another institution, or the end of the study period were censored. All statistical analyses were conducted using EZR version 1.54 (Saitama Medical Center, Jichi Medical University, Saitama, Japan)10. P-values < 0.05 were considered statistically significant.
Results
Patient characteristics
Fifty-one patients who met the eligibility criteria were enrolled in this study. Table 1 presents the patients’ characteristics, including sex, age, etiology, bilirubin level, presence of cholangitis, stricture status, presence of concomitant duodenal stricture, and chemotherapy status. The median follow-up period was 172 (IQR, 80–280) days.
Outcomes
Table 2 presents the outcomes of DBS placement combined with RFA. The technical success rate was 98.0% (50/51), and biliary cannulation failed in 1 patient. The median operative time was 18 (IQR, 15–22) min. Clinical success was achieved in all patients in whom technical success was achieved.
The rate of early AEs was 5.9% (3/51), which included mild pancreatitis (n = 1), mild cholangitis (n = 1), and moderate cholecystitis (n = 1), necessitating endoscopic ultrasound-guided gallbladder drainage. The rate of late AEs was 8.0% (4/50). Non-occlusion cholangitis, which occurred in 1 patient, improved with conservative management. One patient developed a liver abscess, which required percutaneous drainage. Hemobilia occurred in 2 patients, one of whom was treated with conservative management and the other required interventional radiology.
The incidence rate of RBO was 38.0% (19/50). The primary causes of RBO were sludge formation in 13 patients, ingrowth in 4 patients, overgrowth in 1 patient, and remained indeterminate in 1 patient. The incidence rates of sludge occlusion, ingrowth occlusion, and overgrowth occlusion were 26.0%, 8.0%, and 2.0%, respectively. Successful transpapillary reintervention for RBO was performed in 94.7% (18/19) of patients, balloon cleaning was performed in 13 patients, and 5 patients required additional stent placement. One patient exhibited duodenal obstruction at reintervention, for which endoscopic ultrasound-guided hepaticogastrostomy was performed. The median time to RBO was 241 (95% confidence interval, 134-not applicable) days (Fig. 3). The median duration of overall survival was 175 (95% confidence interval, 115–281) days (Fig. 4).
Discussion
This study demonstrated that DBS with endobiliary RFA possessed good technical feasibility and yielded good long-term outcomes and acceptable AE rates, especially a low ingrowth occlusion rate, for the management of MDBO.
Covered and uncovered SEMSs have their respective advantages and disadvantages. Covered SEMSs can prevent ingrowth, but are susceptible to sludge formation and stent migration, in addition to cholecystitis due to cystic duct obstruction3,4. The advantage of uncovered SEMSs is that they are not beset by issues such as cystic duct obstruction and migration, although occlusion due to ingrowth is a frequent occurrence. It is necessary to consider the major factors leading to RBO in each type of SEMS to achieve a longer stent patency period. Attempts have been made to develop covered SEMSs with anti-migration and anti-reflux functions11,12. The DBS was invented with the objective of reducing ingrowth, while preserving the advantages of uncovered stents. Lee et al.5 compared the DBS and conventional uncovered SEMS and reported that tumor ingrowth was less frequent and stent patency was longer with the DBS, indicating that it is a promising option, at least when choosing uncovered SEMSs.
Endobiliary RFA was first developed to extend the duration of stent patency. Some studies have shown that the stricture diameter can be improved after ablation13,14, which is considered to be one of the bases for the extension of the stent patency effect. Since RFA can prevent ingrowth or hyperplasia, it is assumed that it would have good compatibility when used in combination with the uncovered SEMS rather than the covered SEMS or plastic stent. Although a robust consensus has not been reached, some studies have shown prolonged stent patency when RFA is used in combination with the uncovered SEMS6,15,16. In this study, we hypothesized that ingrowth could be further reduced by using DBS in conjunction with RFA. Consequently, the ingrowth rate was low at 8.0%, which seems to be a promising result.
This study should be considered in the context of the limitations associated with its single-center setting and non-randomized design. Because of the lack of control group, whether the favorable outcome was contributed from both DBS and RFA or one independently cannot be answered with this study. Additionally, the results may not be directly applicable to other institutions because all procedures were performed or supervised by a single endoscopist experienced in performing endobiliary RFA and biliary stenting. Since observation is possible only under fluoroscopy during RFA, the ablation effect may depend on the experience of each endoscopist. Further multicenter prospective studies are needed to assess the utility of the combination of DBS and RFA and confirm the findings of the present study while comparing to other approaches.
In conclusion, this is the first study to evaluate the feasibility of the combination of DBS and RFA for the treatment for unresectable MDBO with favorable results. The two modalities demonstrated good compatibility and may serve as an effective option to reduce ingrowth, while preserving the benefits of the uncovered SEMS.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Dumonceau, J. M. et al. Endoscopic biliary stenting: indications, choice of stents, and results: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline—Updated October 2017. Endoscopy 50, 910–930 (2018).
Isayama, H. et al. A prospective randomised study of “covered” versus “uncovered” diamond stents for the management of distal malignant biliary obstruction. Gut 53, 729–734 (2004).
Tringali, A. et al. Covered vs. uncovered self-expandable metal stents for malignant distal biliary strictures: A systematic review and meta-analysis. Endoscopy 50, 631–641 (2018).
Yamashita, Y. et al. Covered versus uncovered metal stent for endoscopic drainage of a malignant distal biliary obstruction: Meta-analysis. Dig. Endosc. https://doi.org/10.1111/den.14260 (2022).
Lee, H. J. et al. A prospective randomized study for efficacy of an uncovered double bare metal stent compared to a single bare metal stent in malignant biliary obstruction. Surg. Endosc. 31, 3159–3167 (2017).
Inoue, T. & Yoneda, M. Updated evidence on the clinical impact of endoscopic radiofrequency ablation in the treatment of malignant biliary obstruction. Dig. Endosc. 34, 345–358 (2022).
Inoue, T. et al. Endobiliary radiofrequency ablation combined with bilateral metal stent placement for malignant hilar biliary obstruction. Endoscopy 52, 595–599 (2020).
Isayama, H. et al. Tokyo criteria 2014 for transpapillary biliary stenting. Dig. Endosc. 27, 259–264 (2015).
Cotton, P. B. et al. A lexicon for endoscopic adverse events: Report of an ASGE workshop. Gastrointest. Endosc. 71, 446–454 (2010).
Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 48, 452–458 (2013).
Hamada, T. et al. Antireflux covered metal stent for nonresectable distal malignant biliary obstruction: Multicenter randomized controlled trial. Dig. Endosc. 31, 566–574 (2019).
Lee, H. W. et al. Usefulness of newly modified fully covered metallic stent of 12 mm in diameter and anti-migration feature for periampullary malignant biliary strictures: Comparison with conventional standard metal stent. J. Gastroenterol. Hepatol. 34, 1208–1213 (2019).
Figueroa-Barojas, P. et al. Safety and efficacy of radiofrequency ablation in the management of unresectable bile duct and pancreatic cancer: a novel palliation technique. J. Oncol. 2013, 910897 (2013).
Wang, F. et al. Endoscopic radiofrequency ablation for malignant biliary strictures. Exp. Ther. Med. 11, 2484–2488 (2016).
Cui, W. et al. Comparison of intraluminal radiofrequency ablation and stents vs. stents alone in the management of malignant biliary obstruction. Int. J. Hyperth. 33, 853–861 (2017).
Uyanık, S. A. et al. Percutaneous endobiliary ablation of malignant biliary strictures with a novel temperature-controlled radiofrequency ablation device. Diagn. Interv. Radiol. 27, 102–108 (2021).
Author information
Authors and Affiliations
Contributions
T.I. Conception and design, data acquisition, analysis and interpretation, and drafting and revision of the manuscript. M.I., R.K., K.S., S.K., Y.K., Y.S., Y.N., K.I. and M.Y.: Data interpretation, and revision of the manuscript.
Corresponding author
Ethics declarations
Competing interests
Tadahisa Inoue received honoraria from Boston Scientific Japan and Japan Lifeline Co., Ltd, outside the submitted work. The other authors disclose no financial relationships relevant to this publication.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary Video 1.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Inoue, T., Ibusuki, M., Kitano, R. et al. Double bare metal stent deployment combined with intraductal radiofrequency ablation for malignant distal biliary obstruction: a prospective pilot study. Sci Rep 13, 2654 (2023). https://doi.org/10.1038/s41598-023-29955-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-29955-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.