Abstract
N-Nitrosodimethylamine (NDMA) detected above the acceptable level in ranitidine products has been a great global concern. To examine the risk of cancer among people treated with ranitidine, we conducted a cohort study using the National Health Insurance Service-National Sample Cohort data (2002–2015) of South Korea. Patients were aged 40 or above as of January 2004 and began receiving ranitidine or other histamine-2 receptor antagonist (H2RA), active comparator, without a history of H2RAs prescription during the prior 2-years. The lag time was designated up to 6 years. The outcomes were an overall incident cancer risk and the risk of major single cancers during the follow-up. The association between ranitidine use and cancer risk was examined by Cox regression model. After exclusion and propensity score matching, 25,360 patients were available for analysis. The use of ranitidine was not associated with the overall cancer risk and major individual cancers [overall cancer: incidence rate per 1000 person-years, 2.9 vs 3.0 among the ranitidine users and other H2RAs users, respectively; adjusted hazard ratio (HR) and 95% confidence interval (95% CI) for all cancers, 0.98 (0.81–1.20)]. The higher cumulative exposure to ranitidine did not increase the cancer risk. Given the insufficient follow-up period, these findings should be interpreted carefully.
Similar content being viewed by others
Introduction
N-Nitrosodimethylamine (NDMA) is a volatile chemical belonging to the nitrosamine class of compounds. It is a by-product of manufacturing processes involving alkylamines that leaches into the air, water, and soil. Human exposure to NDMA may occur through tobacco smoke, food items, especially nitrite-preserved foods, such as cured meats, and various household goods1,2. NDMA can also form in the stomach endogenously during digestion of alkylamine-containing foods3. It is well-established that NDMA is carcinogenic in animals2,4,5,6. Although data in humans is scarce, based on the laboratory studies, NDMA has been classified as “possibly carcinogenic to humans (group 2A)” by the International Agency for Research on Cancer (IARC)7.
The most significant issue in recent years related to NDMA seems to be pharmaceutical contamination. In 2018, NDMA was detected above the acceptable level in pharmaceutical products containing valsartan, an antihypertensive drug8. It was subsequently detected in products containing ranitidine9, nizatidine10, and metformin11 in 2019. In particular, NDMA impurities in ranitidine, a histamine-2 receptor antagonist (H2RA) used to treat and prevent gastric ulcer has raised great concern, considering ranitidine is widely used both as an over-the-counter and prescription drug. Besides, a recent laboratory study using liquid chromatography-high resolution mass spectrometry suggested that ranitidine may be a significant source of NDMA under simulated gastric conditions12. Some evidence suggests that NDMA can arise from the degradation of ranitidine itself with increasing levels over its shelf life. Ranitidine is also suspected of producing NDMA in the human body. These considerations necessitate a study of where ranitidine use itself is linked to cancer risk, regardless of whether NDMA was detected in individual ranitidine products13,14.
In South Korea, all seven ranitidine-based raw ingredients were inspected promptly after the U.S. Food and Drug Administration (FDA) announcement concerning the NDMA impurities in ranitidine drug substances. All of them were found to exceed the domestic acceptable daily limit (0.16 ppm), while the variation is considerable from undetected to 53 ppm depending on the test sample. Accordingly, the Ministry of Food and Drug Safety (MFDS) prohibited the manufacturing, marketing, and prescription of 269 finished products. At that time, the number of patients taking ranitidine reached 1.44 million15. Contamination of NDMA in ranitidine is a global issue. The U.S. FDA has determined that the impurities in NDMA in ranitidine products increases over time to unacceptable levels and, as the latest step, has requested manufacturers withdraw all ranitidine drugs from the market immediately. Similarly, in September 2020, EMA suspended all ranitidine medicines in the EU to the presence of low levels of an impurity of NDMA13.
Studies examined overall cancer risk among ranitidine users in terms of potential NDMA impurities are scarce16,17,18,19. While these studies found no association between ranitidine and risk of cancer, they have limitations such as a short follow-up and generalization16, insufficient control of potential confounding variables17, and use of self-reported exposure18. Studies on the association between exposure to ranitidine and specific cancer site were mostly focused on gastric cancer19,20,21, and the relationship between ranitidine and risk of other single cancer were less investigated22,23. While no evidence of increased risk of gastric cancer was provided by existing studies19,20,21,22, results regarding the risk of bladder cancer are conflicting22,23.
Korea is recognized for highly prevalent prescriptions for acid-suppressing drugs including ranitidine and a wide variety range of ranitidine products demanding a more thorough investigation24. Besides, Korea has the highest rate of gastric cancer in the world25. The present study aimed to estimate the risk of overall cancer and nine cancers by specific sites among people treated with ranitidine with NDMA impurities compared with those treated with other H2RAs.
Materials and methods
Data source
The National Health Insurance Service-National Sample Cohort (NHIS-NSC), a population-based cohort established by the NHIS in South Korea, was used in this study26. This cohort included detailed information regarding medical utilization of about 1 million people as of 2006 (corresponding to about 2.0% of the total eligible Korean population), who were followed for 14 years starting in 2002 until 2015, unless participants’ eligibility was disqualified due to death or emigration. The National Health Insurance (NHI) is a single-insurer system with complete universal healthcare coverage in Korea since 200026. The medical-treatment database includes details of electronic medical-treatment bills, diagnoses, and prescriptions. Information on the database can be obtained from the NHI Sharing Service website (https://nhiss.nhis.or.kr/bd/ab/bdaba005iv.do). Information regarding all medical products licensed and distributed in Korea was obtained from the Health Insurance Review and Assessment Service (HIRA), a government-affiliated organization that reviews and evaluates healthcare costs and healthcare service quality (https://www.hira.or.kr/rd/insuadtcrtr/InsuAdtCrtrList.do?pgmid=HIRAA030069000400).
Study design and population
This was a retrospective cohort study that utilized the NHIS-NSC data (2002–2015). We selected those who were over 40 years of age as of January 1, 2004 (the cohort entry date) as the study subjects to increase the power of individual cancer analysis by securing cases, and to consider the difference in the etiology of cancer in children and adults. New users of ranitidine or other H2RAs were defined as those who took these drugs for the first time between January 1, 2004 and December 31, 2015, without a history of H2RAs prescription two years prior (2002–2003). Patients who had been diagnosed with any cancer during the preceding two-year period were excluded. The exclusion of two years was not a sufficient period to screen only new cancer patients. However, it was determined not to further reduce the period for following up cancer occurrence, considering NHIS-NSC data was available only from 2002 to 2015. Patients who had once switched between ranitidine and an active control drug were also excluded. In addition, patients who received more than one H2RA on the index date, and whose index date was the last day of the study, were excluded. Patients diagnosed with cancer between cohort entry and index date were also excluded. Figure 1 illustrates the algorithm for the selection of study participants.
Exposure definition
While our primary exposure of interest was the use of NDMA-containing ranitidine, we used ranitidine prescription as an alternative measure for the following considerations: First, the MFDS investigated all of the seven active pharmaceutical ingredients(APIs) manufacturers in circulation, and as NDMA was detected in all of them, it was acknowledged that all finished ranitidine products circulating in Korea had potential NDMA impurities and MFDS suspended all ranitidine medicines15. Second, it has been suggested that ranitidine is easily decomposed during storage to form NDMA due to its inherently unstable nature and tertiary amine structure14. Finally, no approach for determining exposure to NDMA-contaminated ranitidine currently. An active comparator was defined as a new user of any of the following H2RA other than ranitidine: cimetidine, lafutidine, nizatidine, famotidine, and roxatidine. Although NDMA was detected in nizatidine, we did not exclude nizatidine users in the control group since the level only slightly exceeded the authorities' criterion of 0.32 ppm (range: 0.34 ppm ~ 1.43 ppm), which corresponds to 1/37 of the detection amount in ranitidine based on the maximum detection amount27. The index date was designated as the first prescription date of ranitidine or other H2RAs.
The cumulative duration of ranitidine use was calculated by summing up all the prescription days, regardless of continuity (< 14 days, 15–30 days, 31–60 days, 61–90 days, 91–180 days, and > 180 days). The cumulative dose of ranitidine in defined daily dose (DDD) provided by World Health Organization (WHO) was also measured, and subjects were categorized into three groups (< 6 DDD, 6–50 DDD, and > 50 DDD).
Outcome and follow-up
The primary outcome was a composite of all cancers during the follow-up period, identified by the International Classification of Disease 10th Revision (ICD-10) (C00-C97). The cancer outcome was double-checked using the V code, a South Korea-specific classification to validate cancer for reimbursement policy purposes. Subjects were followed up from the beginning to diagnosis of cancer, death, loss to follow-up, or December 31, 2015, whichever occurred first. The risk of individual cancers for which animal studies or observational studies previously explored was also assessed. To reflect the induction and latent period until cancer was diagnosed and exclude the possibility of protopathic bias (reverse causation), the lag time was set to two years, and cancer that was diagnosed within the lag time was censored.
Potential confounders
The following potential confounding variables were included as covariates: basic demographic variables, such as age, sex, income level, region, insurance type; Charlson comorbidity index; polypharmacy (number of average daily prescribed drugs ≥ 5); index year; medical histories, such as chronic obstructive pulmonary disease, obesity, alcohol-related disease, hypertension, severe liver disease, diabetes mellitus, kidney disease, disorders of the gallbladder, biliary tract, and pancreas; congestive heart failure; ischemic heart disease; atrial fibrillation; stroke; ulcerative colitis; and co-medications, such as 5-alpha-reductase inhibitors, glucocorticoids for systemic use, hormone replacement therapy, low-dose aspirin, non-aspirin non-steroidal anti-inflammatory drugs, spironolactone, statins, angiotensin-2-antagonists, antidepressants, antipsychotics, and proton pump inhibitors. Comorbidity and co-medication were defined according to previous diagnoses and the prescription of drugs within one year before the index date. The ICD-10 codes used to define the comorbidities are presented in the Supplementary Table 1.
Propensity score matching
After exact 1:3 matching of sex, age, and duration from cohort entry to index date, the propensity scores were estimated for receiving ranitidine prescription by multiple logistic regressions for the all of the aforementioned potential confounding variables (all variables presented in the Table 1). Model discrimination was assessed using C-statistic28. Matching was performed using the Greedy 8 → 1 digit match macro with the estimated propensity score29. The standardized difference was used to compare baseline characteristics of patients treated with ranitidine and other H2RAs, and defined imbalance as an absolute value greater than 0.130.
Stratified analysis and sensitivity analysis
Stratified analyses were conducted according to sociodemographic factors (sex, age, insurance type, income level, and region), comorbidities such as hypertension, diabetes, severe liver disease, chronic pulmonary disease, and comedications, including glucocorticoids for systemic use and non-aspirin non-steroidal anti-inflammatory drugs (NSAIDs). In the stratified design, interactions between ranitidine use and each stratification variable were calculated based on the additive model and presented as a p-value. Sensitivity analyses were performed to examine the robustness of the primary result and to avoid any biases in causality. First, different lag-times were applied, such as no-lag, two years (primary analysis), four years, and six years. Second, the type of intention-to-treat observational study was analyzed to closely emulate a randomized controlled trial31,32, wherein subjects who switched between therapies were not excluded. Third, the person-time of patients diagnosed with cancer during the two-year lag-time period was excluded from the person-time summation to prevent possible underestimation of cancer risk. Fourth, to limit the inclusion of non-compliant individuals, the analysis was performed only for patients who received at least two prescriptions. Finally, since several studies have demonstrated that increasing the look-back period improves the precision in identifying comorbid diseases33, we extended the look-back period for comorbidities and co-medications to 2 years.
Supplementary analysis
We calculated attributable risk (AR) and population attributable risk (PAR) to quantify both the excess risk due to the exposure and the proportion of all incident cancers in the population that could be attributed to the exposure.
Statistical analysis
Descriptive statistics were used to summarize the characteristics of ranitidine users and other H2RAs users at cohort entry34. The crude incidence rates per 1000 person-years with 95% confidence intervals (95% CIs) were calculated based on the Poisson distribution, overall and for each exposure category. Cox proportional hazards models were used to estimate adjusted hazard ratios (HRs) and 95% CIs for cancer associated with ranitidine use compared with other H2RAs use. The Schoenfeld residuals were examined to test proportional hazard assumption35. All data were analyzed using the SAS statistical application program (Version 9.4, SAS Institute Inc, NC, USA).
Ethical approval
This study was approved by the institutional review board of Sungkyunkwan University (No SKKU 2019-12-009), which waived the requirement for informed consent as only deidentified data were used in this study.
Results
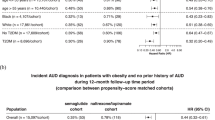
In the overall cohort, 18,666 ranitidine users and 69,294 other H2RA (other than ranitidine) users met the study criteria. After propensity score estimation and one-to-one matching, the cohort included 12,680 ranitidine users and 12,680 other H2RA users (c-statistic: 0.543). The median follow-up period was 5.49 years and 5.79 years in ranitidine users and other H2RA users, respectively. Table 1 provides the baseline characteristics of ranitidine users and H2RA users in the overall cohort and propensity score-matched cohort. All the standardized difference scores in the propensity based matched cohort were less than 0.1 as an absolute value. Figure 1 illustrates the algorithm for the selection of study participants. Table 2 presents the risk for all cancers and individual cancer associated with the use of ranitidine. The use of ranitidine was not associated with all cancers or any type of cancer when compared with H2RAs use. Incidence rate per 1000 person-years was 2.9 and 3.0 among the ranitidine users and other H2RAs users, respectively. The adjusted HR and 95% CI for all cancers were 0.95 (0.83–1.09) in the overall cohort and 0.98 (0.81–1.20) in the propensity score-matched cohort. In both the overall and propensity score-matched cohorts, the risk of kidney cancer related to ranitidine use appeared to be greater than with other H2RAs use, but there was no statistical significance [HR (95% CI), 1.49 (0.61–3.61) in the overall cohort; 2.65 (0.51–13.67) in the propensity score-matched cohort]. In all the other individual cancers examined, no association with ranitidine use was observed either. The higher cumulative exposure to ranitidine, measured by duration in days and dose in milligrams, did not increase the risk of developing cancer than with other H2RAs use (Table 3).
In stratified analysis, ranitidine use was not associated with risk of cancer in any stratum, and indicated no significant interaction. However, relatively high HR with wide confidence interval was estimated in the women [adjusted HR (95% CI), 1.28 (0.92–1.78)] given the statistical insignificance. (Table 4).
The results from the sensitivity analyses I, in which the lag time varied from no lag-time to six years, did not differ from the main findings. This finding suggested that no association existed between the use of ranitidine and cancer risk at any lag-time setting (Table 5). However, despite the lack of statistical significance, a slightly higher risk of cancer was present in the six-year lag-time setting in the propensity score-matched analysis [HR (95% CI), 1.12 (0.79–1.59)] (Table 5). Sensitivity analysis II, which included all subjects who experienced switching, and sensitivity analysis III, which included all patients with cancer during lag-time, provided similar results to those of the primary analysis (Tables 6, 7). The results of the sensitivity study IV, which excluded those who had only ever received one prescription, and V, which extended the look-back time for comorbidities and co-medications to two years, did not differ from the primary results (Supplementary Tables 2 and 3). Supplementary analysis did not show cancer risk attributed to ranitidine use (Supplementary Table 2).
Discussion
As unacceptable levels of NDMA impurities were detected in many ranitidine products in 2019, health authorities, such as the FDA, EMA, and MFDS, took measures to withdraw ranitidine products from the market. In this population-based study, the association between the use of ranitidine and cancer risk was investigated. This study provided no evidence of association of NDMA impurities in ranitidine products with the risk of cancer. Little can be suggested about individual cancers due to the lack of power, these results remained consistent in the stratified analysis and several sensitivity analyses. The cohort’s follow-up was 5.5 years, not long enough to assess long-term cancer risk. The findings should be considered as short-term cancer risk.
Comparison with other studies
NDMA is a probable human carcinogen, based on laboratory studies, so its effect on humans rely on observational studies. Most studies in humans are nutritional epidemiological research, focusing on the dietary consumption of NDMA36,37,38,39,40,41,42, while some studies have evaluated the impacts of occupational exposure42,43. There are varied results depending on the study design, exposure level, and carcinoma of interest, but significant results have been suggested in a large number of studies.
According to a recent meta-analysis that evaluated the relationship between NDMA and gastric cancer by integrating 11 studies, NDMA increased the risk of gastric cancer [HR (95% CI), 1.34 (1.02 to 1.76)]44. Other studies on dietary intake of NDMA have shown significant findings in lung cancer40, colorectal cancer40, pancreatic cancer45, and upper aerodigestive tract cancer (laryngeal, esophageal, and oral)38. In a recent study with a long follow-up period (49 years) and lag-time (15 years) to evaluate the exposure–response relationship between occupational exposures to N-nitrosamines and cancer mortality in the UK rubber industry, NDMA exposure was associated with overall cancers [HR (95% CI), 2.08 (1.96–2.21)] and cancers of the bladder, stomach, leukemia, multiple myeloma, prostate, and liver43. Another analysis involving a 10-year lag time cohort of rubber employees found that exposure to high concentrations of nitrosamine, calculated as NDMA and N-nitrosomorpholine, was correlated with an increased mortality from oesophagus, oral cavity, and pharynx cancers42.
Our findings were distinct from those of the previous nutritional or occupational epidemiological studies stated above; however, a direct comparison with our study would not be suitable. Confounding is a specific challenge in nutritional epidemiological research because dietary components are correlated, making it difficult to distinguish their impacts. In addition, the self-administered tools for dietary NDMA exposure measurements, such as food frequency questionnaires, have a high risk of recall bias46. The association between dietary NDMA consumption and gastric cancer risk was primarily noted in case–control studies rather than in cohort studies44, indicating the likelihood of differential misclassification in exposure due to recall bias. Regarding studies on occupational NDMA exposure and cancer risk, exposure measures based on airborne concentrations and plant-specific conditions are far from the line of our investigation.
The issue of NDMA contaminated ranitidine was very recently, in 2019. To our knowledge, a few studies have investigated the link between the potential NDMA impurities in ranitidine and overall cancer risk16,17,18. The estimates of overall cancer risk levels in our study were very close to those reported in these studies. Two previous studies are similar to our study in that they used claim data. The Japanese study has a short follow-up period, which can provide insight on short-term cancer risk, and has limitations in terms of external validity as it only targets employed workers and their families16. The study in Korea secured comparability with famotidine users as a control group. However, the researchers noted that simply matching by gender, age, cumulative time, and diabetes mellitus provided insufficient control for potential confounding variables17. In the study using UK Biobank, exposure was self-reported, with little information18. In the case of individual cancers, we did not found statistical significance in any single carcinoma tested which is in line with the previous studies. However, the studies had the same limitation (power was not secured due to the small number of subjects and events). Notably, a recent nested case–control study showed the link between the use of ranitidine and the risk of bladder cancer23.
In the duration/dose response analysis, the group with the longest use period (> 180 days) or highest cumulative dose (> 50 DDD) showed a lower HR (HR [95% CI], 0.53 [0.28–1.01], 0.78 [0.53–1.14], respectively). These results are similar to those of a previous ranitidine/nizatidine study showing the lowest HR in the highest cumulative usage group (above 730 defined daily dose) [HR (95% CI), 0.83 (0.45–1.55)], although it did not reach statistical significance16. Termination of exposure may be related to the presence of disease (a variant of the ‘healthy worker effect’)47. Rather than interpreting these results as a possible reverse causation, it is likely that people with large amounts of cumulative ranitidine use may be due to an increase in person-time because cancer has not yet occurred. This is likely to be less biased if it was possible to determine the cumulative exposure to ranitidine with sufficient exposure window before follow-up, and to follow the cohort long after termination of exposure.
In this study, kidney cancer presented the highest HR among the examined cancer sites [HR (95% CI), 2.65 (0.51–13.67) in the propensity score-matched cohort], although sufficient power was not ensured. A laboratory study that analyzed NDMA levels after oral intake of ranitidine reported that urinary excretion of 150 mg ranitidine after 24 h increased by 400 times, from 110 to 47,600 ng48. Research on the relationship between ranitidine use and kidney cancer needs to be conducted more closely in the future.
The FDA has stated that the levels of NDMA in ranitidine are close to those of common foods items such as grilled or smoked meat49. The FDA determined that ingestion of ≤ 96 ng or 0.32 ppm of NDMA per day should be reasonably safe in humans49. FDA has set the same acceptable daily intake limit for NDMA for ranitidine49. However, the exposure to NDMA from taking ranitidine is likely to be very high in some patients. For instance, if a patient had taken a ranitidine product containing 14.68 ppm of NDMA, which is the minimum detected amount of a specific company's raw ranitidine substance sample in Korea15, for 1 year consecutively, that is the same as taking a quantity of 46 times the FDA's acceptable limit (0.32 ppm) throughout the year. Considering that clinicians usually keep prescribing a specific pharmaceutical brand in Korea, this level of exposure will not be very rare. For comparison, in nutritional epidemiologic studies that explored the risk of dietary intake of NDMA, the cancer risk in the highest tertile or quintile was 1.437, 1.9650, or 2.4351 compared to that in the lowest exposure group. However, the daily dietary exposure to NDMA estimated in these studies ranged from 190 to 240 ng/day, which is only 2–4 times the acceptable limit of FDA.
Strengths and limitations
This study has several strengths. First, through propensity score analysis and employing active control, comparability was enhanced, and confounding by indication could be lessened. Second, misclassification by switching was prevented by excluding patients who had experienced switching between ranitidine and active comparator. Third, as the risk window and latency were difficult to determine, the latency period was included by placing multiple risk windows for a lag time of up to 6 years. Finally, the possible misclassification of outcome variables was lowered by utilizing the V code when identifying cancer occurrence. In a study using Korean National Health Insurance (NHI) claims database, cases registered as pancreatic cancer by ICD-10 and V codes without pathologic confirmation achieved a high accuracy including a positive predictive value of 98.08%. Whether ranitidine, which has been used by many people for a long time, raise the risk of cancer is a critical question that requires long-term investigation. We expect that our study reduce uncertainty by confirming the findings of a limited existing studies that suggested no link between ranitidine use and short term cancer risk. Nonetheless, the results of this study should be interpreted with caution due to certain significant limitations. First, the follow-up period was not long enough to confirm the relationship between NDMA and cancer incidence, which is a critical disadvantage of our study. In addition, NDMA acts as an initiator and takes longer from exposure to cancer, which contrasts with the fact that drug exposure mostly serves as a promotor when exerting cancer development52. Among the prior nutritional epidemiologic studies, the follow-up periods in cohort studies suggesting significant association ranged from 11.4 to 24 years41,50,51,53. Due to the variations in research methodologies, direct comparisons may not be feasible. However, in the two studies with the most extended follow-up periods (18 years and 24 years), the HR for cancer incidence was 2.0 (gastric cancer) and 2.12 (colorectal cancer), respectively41,50, which are higher than those reported in other studies. On the other hand, a research with 6.6 years of follow-up did not indicate relevance54. Second, the risk of individual cancers, high-dose users, and different subgroups was explored in our research. However, the results generally failed to secure statistical power and did not yield sufficiently valuable evidence. The substantial loss of eligible subjects can be attributed to implementing an active comparator and excluding those who experienced switching. Third, the level of NDMA impurities in ranitidine varies by product, defined as exposure in this study, may not accurately represent NDMA exposure. Fourth, the chances of residual confounding may remain because the potential confounding factors, such as food, cigarette smoking, and alcohol consumption, were not included. Fifth, since prescription data from the hospitals’ claim data was used in this study, we could not verify if the prescriptions were actually filled. Finally, one year look-back period for comorbidities and co-medication was insufficient. Finally, measuring the cumulative use from the follow-up start date may lead to immortal time bias.
In summary, no association was found between ranitidine with potential NDMA impurities and the risk of overall cancer and major individual malignancies. Our study supported the findings of other investigations after rigorous controlling for confounding variables to ensure comparability in the population where ranitidine use was highly prevalent. The findings should be interpreted with caution considering insufficient follow-up, and longer follow-up are required to estimate long-term risk of cancer.
Data availability
The health insurance claims database of the National Health Insurance Service can be accessed at https://nhiss.nhis.or.kr/bd/ab/bdaba022eng.do.
References
US Department of Health and Human Services. Hazardous Substances Data Bank (HSDB, Online Database). (National Toxicology Information Program, National Library of Medicine, 1993).
Agency for Toxic Substance & Disease Registry (ATSDR). Public Health Statement for n-Nitrosodimethylamine (ATSDR, 2022).
Vermeer, I., Pachen, D., Dallinga, J. W., Kleinjans, J. & Van Maanen, J. Volatile N-nitrosamine formation after intake of nitrate at the ADI level in combination with an amine-rich diet. Environ. Health Perspect. 106(8), 459–463 (1998).
Koppang, N. & Rimeslåtten, H. Toxic and carcinogenic effects of nitrosodimethylamine in mink. IARC Sci. Publ. 14, 443–452 (1976).
Agency for Toxic Substances and Disease Registry (ATSDR). Toxicological profile for N-nitrosodimethylamine. in US Public Health Service in collaboration with US Environmental Protection Agency (EPA) (1989).
Klein, R. et al. Effects of long-term inhalation of N-nitrosodimethylamine in rats. IARC Sci. Publ. 105, 322–328 (1991).
World Health Organization. N-Nitrosodimethylamine. Concise International Chemical Assessment Document 38 (CICADS 38) (World Health Organization, 2002).
European Medicines Agency. EU Inspection Finds Zhejiang Huahai Site Non-Compliant for Manufacture of Valsartan: EMA and National Authorities Considering Impact on Other Active Substances Produced at the Site [Press Release]. (European Medicines Agency, 2019).
The U.S. Food & Drug Administration. Statement Alerting Patients and Health Care Professionals of NDMA Found in Samples of Ranitidine (2019).
The U.S. Food & Drug Administration. 4/16/2020 Update-FDA Alerts Patients and Health Care Professionals to Amneal's Voluntary Recall of Nizatidine. (2020).
The U.S. Food & Drug Administration. FDA Updates and Press Announcements on NDMA in Metformin (2020).
Braunstein, L. Z. et al. Analysis of ranitidine-associated N-nitrosodimethylamine production under simulated physiologic conditions. JAMA Netw. Open 4(1), e2034766–e2034766 (2021).
European Medicines Agency. Ranitidine-Containing Medicinal Products. (2020). https://www.ema.europa.eu/en/medicines/human/referrals/ranitidine-containing-medicinal-products.
Abe, Y. et al. Temperature-dependent formation of N-nitrosodimethylamine during the storage of ranitidine reagent powders and tablets. Chem. Pharm. Bull. 20, 00431 (2020).
The Ministry of Food and Drug Safety. The Ministry of Food and Drug Safety Temporarily Suspends Manufacturing, Import and Sales of the Gastrointestinal Drug Ranitidine. https://www.mfds.go.kr/brd/m_99/view.do?seq=43717&srchFr=&srchTo=&srchWord=&srchTp=&itm_seq_1=0&itm_seq_2=0&multi_itm_seq=0&company_cd=&company_nm=&page=1. Accessed 10 Sept 2020.
Iwagami, M. et al. Risk of cancer in association with ranitidine and nizatidine vs other H2 blockers: Analysis of the Japan medical data center claims database 2005–2018. Drug Saf. 1, 1–11 (2020).
Yoon, H. J., Kim, J.-H., Seo, G. H. & Park, H. Risk of cancer following the use of N-nitrosodimethylamine (NDMA) contaminated ranitidine products: A nationwide cohort study in South Korea. J. Clin. Med. 10(1), 153 (2021).
Kantor, E. D. et al. Ranitidine use and cancer risk: Results from UK Biobank. J. Gastroenterol. 160(5), 1856–1859 (2021).
Adami, H.-O. et al. Ranitidine use and risk of upper gastrointestinal cancers: Ranitidine and upper gastrointestinal cancers. J. Gastroenterol. 30(12), 2302–2308 (2021).
Kim, S., Lee, S., Hong, J., Ko, I., Kim, J.-Y. & Kim, D.-K. Effect of ranitidine intake on the risk of gastric cancer development. Healthcare (2021).
Kim, Y. D. et al. No association between chronic use of ranitidine, compared with omeprazole or famotidine, and gastrointestinal malignancies. Healthcare 54(5), 606–615 (2021).
Nørgaard, M. et al. Ranitidine and risk of bladder and kidney cancer: A population-based cohort study. Healthcare 31(1), 45–50 (2022).
Cardwell, C. R., McDowell, R. D., Hughes, C. M., Hicks, B. & Murchie, P. Exposure to ranitidine and risk of bladder cancer: A nested case-control study. Am. Coll. Gastroenterol. 116(8), 1612–1619 (2021).
Noh, Y., Lee, J. M. & Sooyoung, S. Analysis of healthcare personnel’s clinical beliefs and knowledge behind overutilization of stress ulcer prophylaxis in hospitalized patients. Korean J. Clin. Pharm. 25(4), 264–272 (2015).
Morgan, E. et al. The current and future incidence and mortality of gastric cancer in 185 countries, 2020–40: A population-based modelling study. EClinicalMedicine. 47, 101404 (2022).
Lee, J., Lee, J. S., Park, S.-H., Shin, S. A. & Kim, K. Cohort profile: the national health insurance service-national sample cohort (NHIS-NSC), South Korea. Int. J. Epidemiol. 46(2), e15–e15 (2017).
Ministry of Health and Welfare. Ministry of Food and Drug Safety Announces Measures to Control Impurities in Raw Ingredients. http://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&page=1&CONT_SEQ=351610. Accessed 12 Dec 2019.
Westreich, D., Cole, S. R., Funk, M. J., Brookhart, M. A. & Stürmer, T. The role of the c-statistic in variable selection for propensity score models. Pharmacoepidemiol. Drug Saf. 20(3), 317–320 (2011).
Parsons, L. Reducing bias in a propensity score matched-pair sample using greedy matching techniques. in Proceedings of the Twenty-Sixth Annual SAS Users Group International Conference. (2001).
Yang, D. & Dalton, J. E. A unified approach to measuring the effect size between two groups using SAS®. SAS Glob. Forum. 335, 1–6 (2012).
Wallis, C. J. et al. Survival and cardiovascular events in men treated with testosterone replacement therapy: An intention-to-treat observational cohort study. Lancet Diabetes Endocrinol. 4(6), 498–506 (2016).
Hernán, M. A. et al. Observational studies analyzed like randomized experiments: An application to postmenopausal hormone therapy and coronary heart disease. Epidemiology 19(6), 766 (2008).
Charlson, M. E., Carrozzino, D., Guidi, J. & Patierno, C. Charlson comorbidity index: A critical review of clinimetric properties. Psychother. Psychosom. 91(1), 8–35 (2022).
Tuccori, M. et al. Pioglitazone use and risk of bladder cancer: Population based cohort study. BMJ 352, 1541 (2016).
Schoenfeld, D. Partial residuals for the proportional hazards regression model. Biometrika 69(1), 239–241 (1982).
Pobel, D., Riboli, E., Cornée, J., Hémon, B. & Guyader, M. Nitrosamine, nitrate and nitrite in relation to gastric cancer: A case-control study in Marseille, France. Eur. J. Epidemiol. 11(1), 67–73 (1995).
La Vecchia, C., D’Avanzo, B., Airoldi, L., Braga, C. & Decarli, A. Nitrosamine intake and gastric cancer risk. Eur. J. Cancer Prev. 4(6), 469–474 (1995).
Rogers, M., Vaughan, T. L., Davis, S. & Thomas, D. B. Consumption of nitrate, nitrite, and nitrosodimethylamine and the risk of upper aerodigestive tract cancer. Cancer Epidemiol. Biomark. Prev. 4(1), 29–36 (1995).
De Stefani, E., Deneo-Pellegrini, H., Carzoglio, J. C., Ronco, A. & Mendilaharsu, M. Dietary nitrosodimethylamine and the risk of lung cancer: A case-control study from Uruguay. Cancer Epidemiol. Biomark. Prev. 5(9), 679–682 (1996).
Zhu, Y. et al. Dietary N-nitroso compounds and risk of colorectal cancer: A case–control study in Newfoundland and Labrador and Ontario, Canada. Br. J. Nutr. 111(6), 1109–1117 (2014).
Knekt, P., Järvinen, R., Dich, J. & Hakulinen, T. Risk of colorectal and other gastro-intestinal cancers after exposure to nitrate, nitrite and N-nitroso compounds: A follow-up study. Int. J. Cancer. 80(6), 852–856 (1999).
Straif, K. et al. Exposure to high concentrations of nitrosamines and cancer mortality among a cohort of rubber workers. Occup. Environ. Med. 57(3), 180–187 (2000).
Hidajat, M. et al. Lifetime exposure to rubber dusts, fumes and N-nitrosamines and cancer mortality in a cohort of British rubber workers with 49 years follow-up. Occup. Environ. Med. 76(4), 250–258 (2019).
Song, P., Wu, L. & Guan, W. Dietary nitrates, nitrites, and nitrosamines intake and the risk of gastric cancer: A meta-analysis. Nutrients 7(12), 9872–9895 (2015).
Zheng, J. et al. Dietary N-nitroso compounds and risk of pancreatic cancer: Results from a large case-control study. Carcinogenesis 40(2), 254–262 (2019).
Vuholm, S., Lorenzen, J. K. & Kristensen, M. Relative validity and reproducibility of a food frequency questionnaire to assess dietary fiber intake in Danish adults. Food Nutr. Res. 58(1), 24723 (2014).
Thomas, D. C. Models for exposure-time-response relationships with applications to cancer epidemiology. Annu. Rev. Public Health. 9(1), 451–482 (1988).
Zeng, T. & Mitch, W. A. Oral intake of ranitidine increases urinary excretion of N-nitrosodimethylamine. Carcinogenesis 37(6), 625–634 (2016).
The U.S. Food & Drug Administration. Laboratory tests. Ranitidine: Laboratory Analysis of Ranitidine and Nizatidine Products. (2019).
Larsson, S. C., Bergkvist, L. & Wolk, A. Processed meat consumption, dietary nitrosamines and stomach cancer risk in a cohort of Swedish women. Int. J. Cancer. 119(4), 915–919 (2006).
Keszei, A. P., Goldbohm, R. A., Schouten, L. J., Jakszyn, P. & van den Brandt, P. A. Dietary N-nitroso compounds, endogenous nitrosation, and the risk of esophageal and gastric cancer subtypes in the Netherlands Cohort Study. Am. J. Clin. Nutr. 97(1), 135–146 (2013).
Pottegård, A., Friis, S., Stürmer, T., Hallas, J. & Bahmanyar, S. Considerations for pharmacoepidemiological studies of drug–cancer associations. Basic Clin. Pharmacol. Toxicol. 122(5), 451–459 (2018).
Loh, Y. H. et al. N-nitroso compounds and cancer incidence: The European prospective investigation into cancer and nutrition (EPIC)–Norfolk Study. Am. J. Clin. Nutr. 93(5), 1053–1061 (2011).
Jakszyn, P. et al. Endogenous versus exogenous exposure to N-nitroso compounds and gastric cancer risk in the European Prospective Investigation into Cancer and Nutrition (EPIC-EURGAST) study. Carcinogenesis 27(7), 1497–1501 (2006).
Acknowledgements
This work was supported by a Grant (21153MFDS607) from Ministry of Food and Drug Safety of South Korea in 2021–2025.
Author information
Authors and Affiliations
Contributions
K.I.J. contributed to the design and interpretation of the research, and wrote the manuscript. J.E.H. designed the overall research, interpreted the data, and contributed to the writing the manuscript. I.S.O. conducted statistical analyses and contributed to the research design. S.I.C. contributed to the data interpretation and writing the manuscript. J.Y.S. designed the study, supervised the statistical analyses and interpretation of data, and critically revised the manuscript. J.Y.S., guarantor of the study, accepts full responsibility for the research, had access to the data, and controlled the decision to publish. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Joung, KI., Hwang, J.E., Oh, IS. et al. Association between ranitidine use with potential NDMA impurities and risk of cancer in Korea. Sci Rep 12, 22396 (2022). https://doi.org/10.1038/s41598-022-26691-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-26691-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.