Abstract
Patients with rare solid tumors treated on early phase trials experience toxicities from their tumors and treatments. However, limited data exist to describe the detailed symptom burden suffered by these patients, particularly those with rare solid tumors treated with immunotherapy. We performed a prospective longitudinal study to capture patient-reported symptom burden. Patients completed the validated MD Anderson Symptom Inventory (MDASI)—Immunotherapy with 20 symptoms including 7 immunotherapy-specific items and 6 interference items at baseline and weekly thereafter for up to 9 weeks. Symptoms and interference were rated on 0–10 scales (0 = none or no interference, 10 = worst imaginable or complete interference). Group-based trajectory modelling determined higher and lower symptom groups. A total of 336 MDASI questionnaires were completed by 53 patients (mean age 55.4y, 53% male) with advanced rare cancers receiving pembrolizumab in a Phase II clinical trial. Symptoms reported as most severe over the course of the treatment over 9 weeks were fatigue [mean (M) = 3.8, SD = 2.3], pain (M = 3.7, SD = 2.9), disturbed sleep (M = 2.7, SD = 2.3), drowsiness (M = 2.6, SD = 2.0) and lack of appetite (M = 2.5, SD = 2.1). Pain in the abdomen (M = 2.2, SD = 2.4), rash (M = 1.1, SD = 1.8) and diarrhea (M = 0.9, SD = 1.5) were less severe. Interference with walking was rated the highest (M = 3.4, SD = 2.8) and relations with others was rated the lowest (M = 2.1, SD = 2.6). Using a composite score based on the five most severe symptoms (fatigue, pain, lack of appetite, feeling drowsy and sleep disturbance), 43% were classified into the high symptom burden group. Using a score based on immunotherapy-specific symptoms (e.g., rash, diarrhea) 33% of patients were included in the high symptom group. Symptom burden stayed relatively stable in the high- and low-symptom burden patient groups from baseline through 9 weeks. Some patients with rare malignancies experienced high symptom burden even at baseline. In patients with rare cancers, symptom trajectories stayed relatively stable over nine weeks of treatment with pembrolizumab.
Trial registration: ClinicalTrials.gov identifier: NCT02721732.
Similar content being viewed by others
Introduction
Patient reported outcomes (PRO) provide a patient the opportunity to describe what a patient is experiencing during and after treatment, the degree to which treatment produces such symptoms, and impact on functioning. The use of validated PRO measures in clinical trials can provide the patient’s assessment of the severity and impact of treatment-related symptoms of new therapies. This assessment provides critical information to patients, providers, regulators, and third-party payers for evaluating the tolerability of these therapies1 and for judging the safety and value (ratio of treatment benefit relative to cost)2 of one therapy over another. This is especially true when new therapies provide only small increases in overall survival or time to progression, or are effective for only a modest percentage of the patients who receive them. Thus, PROs may be considered an essential component of oncology drug development, without which clinicians and regulators have an incomplete picture of how patients are affected by a new agent3. Indeed, in a policy review, international regulatory agencies from the USA, Europe, and Canada have acknowledged interest in the inclusion of PROs throughout the drug development process4. Most symptomatic toxicities data currently are from clinician-registered adverse event (AE) reports, and prior research by others suggest that symptomatic AEs are likely to be underreported by clinicians5.
Immune checkpoint inhibitors are a new class of immunotherapeutic agents that remove the inhibitory signal provided to immune T cells so they can launch a cytotoxic attack on tumor cells. It is increasingly clear that immune checkpoint inhibitors produce a unique and emerging set of irAEs6,7, many of which present as symptoms and can thus be well captured by patient report. Because irAEs are classically autoimmune in nature8 and are often T-cell-mediated9, the toxicities of checkpoint inhibitors may be caused by T cells indiscriminately attacking both tumor cells and normal cells. Given the effects of checkpoint inhibitors on the immune system, their side-effect profiles may differ somewhat from those of other cancer therapies, including conventional cytotoxic chemotherapy. Yet, although immune checkpoint inhibitors seem promising in prolonging survival, little is known about their symptom related benefit or burdens from the patient’s perspective. As immunotherapy become generally used, it is important to be able to describe to patients what types of side effects they could expect from the treatment10. While there are trials that have used PRO, few have used frequent assessments to describe the trajectory of symptoms longitudinally across treatment in patients with rare cancers.
Pembrolizumab is an immune checkpoint inhibitor that blocks the programmed cell death protein 1 (PD1), an inhibitory receptor expressed by immune T cells. PD1 blockade enables T cells to destroy cancer cells. Pembrolizumab was granted accelerated approval by the FDA not only for treatment of multiple tumor types, but also for tumor-agnostic conditions such as high microsatellite instability (MSI-H) or mismatch repair deficient (dMMR) solid tumors and those with high tumor mutational burden11. We have previously reported clinical activities of Pembrolizumab in patients with advanced rare tumors12.
We report here frequent assessment of symptomatic status of patients in a Phase II trial of patients with rare cancer receiving pembrolizumab. We describe the symptom patterns of these patients and classified them into two groups based on the severity of their longitudinal symptom severity. We elucidate how these patients feel and function with regards to their immune checkpoint inhibitor treatment.
Methods
Study participants
Ten patient cohorts with advanced rare cancers were used to describe the symptom burden associated with pembrolizumab. Patients completed the validated MD Anderson Symptom Inventory—Immunotherapy (MDASI-Immunotherapy EPT) module for early phase trials (13) at baseline and weekly thereafter for up to 9 weeks. Symptoms and interference were rated on 0–10 scales (0 = none or no interference, 10 = worst imaginable severity or complete interference).
Patients were in a Phase II basket trial in the Clinical Center for Targeted Therapy clinic at MD Anderson and were receiving 200 mg of pembrolizumab intravenously every three weeks. (12) Sample size for this descriptive longitudinal study was based on reporting the symptom results with reasonable confidence limits using eligible patients. To be eligible for this PRO-based study, patients were required to be at least 18 years old, speak English, and have a pathological diagnosis of a rare cancer, whose disease had progressed while on standard therapies (if available) within the previous 6 months. Patients were excluded if clinical research staff felt that they did not understand the intent of the study or could not complete the assessment measures. This study was approved by the Institutional Review Board of The University of Texas MD Anderson Cancer Center in Houston, Texas (MDACC protocols 2015–0948 and PA15-0315). The study was conducted in accordance with the Declaration of Helsinki and the International Conference on Harmonization Good Clinical Practice guidelines. All the study participants provided written informed consent before enrollment.
Demographic and clinical data
At the time of patient enrollment, research staff asked study participants to complete self-administered questionnaires, answered questions, and assisted with completion of survey forms as needed. Patient demographic information (e.g., sex, age, marital status, education level, and employment status) were collected during the initial clinic visit.
Medical background information was extracted from electronic medical records, including cancer diagnosis, and Eastern Cooperative Oncology Group performance status (ECOG PS). ECOG PS14 was used to estimate disease severity and is a physician-rated measure of functional ability, ranging from 0 (fully active; able to carry on all pre-disease performance without restriction) to 4 (completely disabled; cannot perform self-care; totally confined to bed or chair).
Study instrument
The M. D. Anderson Symptom Inventory – Immunotherapy for early phase trials (EPT)
The MDASI-Immunotherapy EPT has 20 symptoms including 7 immunotherapy-specific items in addition to the 13 MDASI core symptoms15. The MDASI asks patients to rate the severity of disease-related and treatment-related symptoms during the past 24 h. Each symptom (pain, fatigue, nausea, disturbed sleep, emotional distress, shortness of breath, difficulty remembering, lack of appetite, drowsiness, dry mouth, sadness, vomiting, numbness or tingling, rash, diarrhea, pain the abdomen, swelling in the hands and legs, headache, night sweats and fever and/or chills) is rated on an 11-point scale ranging from 0 (not present) to 10 (as bad as you can imagine). The MDASI-Immunotherapy EPT has been shown to be valid and reliable13.
Patients also rate the degree to which symptoms interfered with various aspects of life during the past 24 h. Each interference item (general activity, mood, normal work [including both work outside the home and housework], relations with other people, walking ability, and enjoyment of life) is rated on an 11-point scale ranging from 0 (did not interfere) to 10 (interfered completely). The interference factor can be decomposed into (1) an activity-related interference dimension consisting of the items normal work, general activity, and walking ability, and (2) a mood-related interference dimension composed of the items relations with people, enjoyment of life, and mood16.
Statistical analysis
Most statistical analyses were conducted using Statistical Package of the Social Sciences (SPSS) software version 26. Correlations, means, standard deviations (SDs), ranges, and 95% confidence limits (CL) were computed for all symptoms and subscales. Statistical significance was set using a two-tailed alpha level of 0.05.
Group-based trajectory modeling (GBTM)
Cluster analysis is a commonly used method to group patients based on how similarly they report the severity of their symptoms. But because symptoms change over the course of cancer treatment, patient groupings may vary across time points. To account for this, we used group-based trajectory model (GBTM) under PROC TRAJ in SAS. This method is a statistical approach designed to group longitudinal observations into interrelated subgroups. Like cross-sectional methods, GBTM takes into consideration measures at a given time point, but unlike cross sectional methods, GBTM considers the change patterns of those measures across multiple time points. GBTM may identify two or more groups with distinct trajectories. For simplicity and because of our limited sample size, we sought to determine group membership in either high or low symptom burden over 9 weeks depending on the outcome variable used. In our case, we performed GBTM using two outcome variables. First, we created high and low symptom burden groups based on the average of the top 5 symptoms namely, fatigue, pain, lack of appetite, feeling drowsy and disturbed sleep. Second, we used the average of the 7 immunotherapy-specific symptoms to form groups. The group trajectories were described as linear regression lines with intercept and slope. A non-significant slope estimate suggests a stable pattern.
Results
Demographic and clinical characteristics of study cohorts
If all 53 patients completed every MDASI assessments from baseline to the end of 9 weeks, then we will have 530 MDASIs. Because some patients dropped out of the study, no further MDASI assessments were expected for those patients. Out of the 502 expected MDASI questionnaires, 336 were completed by 53 patients for a 67% completion rate. Reasons for dropout/termination included non-compliance (n = 7), progression (n = 20), withdrawal of consent (n = 2), and toxicity (n = 2). Demographic and clinical characteristics of the patient cohort of 53 patients are summarized in Table 1. Overall, the average and median age were 55.4 and 61 years respectively, and the mean education level was 14 years. Male represented 53% (n = 28), and the sample was predominantly non-Hispanic white. Most patients had an ECOG performance status of 1.
Pattern of symptom burden during the first 9 weeks of pembrolizumab treatment
Table 2 shows symptom severity in patients with rare solid tumors at baseline, at weeks 1–3, at weeks 4–6, weeks 7–9, and the average of values for 9 weeks of treatment with pembrolizumab. Symptoms with the worst severity at baseline were fatigue, pain, disturbed sleep, lack of appetite and drowsiness. The most severe symptoms at 7–9 weeks of treatment with pembrolizumab were pain, fatigue, lack of appetite, disturbed sleep and drowsiness. Symptoms reported as most severe over the course of the treatment over 9 weeks were fatigue [mean (M) = 3.8, SD = 2.3), pain (M = 3.7, SD = 2.9), disturbed sleep (M = 2.7, SD = 2.3), feeling drowsy (M = 2.6, SD = 2.0) and lack of appetite (M = 2.5, SD = 2.1). Pain in the abdomen (M = 2.2, SD = 2.4), rash (M = 1.1, SD = 1.8) and diarrhea (M = 0.9, SD = 1.5) were rated lower and ranked as 6th, 16.5th and 18th worst of the 20 symptoms. Interference with walking was rated the highest (M = 3.4, SD = 2.8) with relations rated as the lowest (M = 2.1, SD = 2.6).
Figure 1a shows relative stability of a composite score of the top five symptoms (albeit with very minor variations) over 9 weeks of treatment with pembrolizumab using all available data at each time points. In order to determine whether dropouts affected the severity of symptom patterns, we reproduced the plot in Fig. 1a but using data only from patients with complete data for all 9 weeks. Figure 1b is very similar to Fig. 1a in that the mean severity is around 3 on a 0 to 10 scale.
(a) Mean values for the composite score of the top five symptoms (pain, fatigue, disturbed sleep, lack of appetite, and drowsiness) over 9 weeks of treatment with pembrolizumab in all patients with rare tumors who started the trial (N = 53). (b) Mean values for the composite score of the top five symptoms over 9 weeks of treatment with pembrolizumab in patients with rare tumors who completed 9 weeks of treatment with pembrolizumab (N = 22).
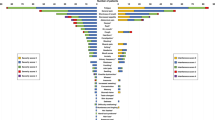
Figure 2 shows the percentages of patients experiencing moderate to severe levels of the 13 most prominent symptoms over the 9 weeks grouped into 4 time periods of pembrolizumab treatment. More than a third of patients experience fatigue at the beginning of their treatment with a quarter of the patients still reporting fatigue to be moderate to severe. At least 10% of patients reported moderate to severe levels at baseline for any of the top 13 symptoms. With the exception of pain and dry mouth, patients reported that many symptoms either stayed the same or showed slight improvement from baseline to Weeks 7–9.
Group-based trajectory pattern of symptom burden during the first 9 weeks of pembrolizumab treatment
Figure 3a shows the results of group- based trajectory modeling of the top 5 symptoms. Using a composite score based on the five most severe symptoms (pain, fatigue, lack of appetite, sleep disturbance and feeling drowsy), 43% were classified into the high symptom burden group. There were no significant increase in symptom during this period for either the high symptom burden group (est = − 0.02, p < 0.87) or the low burden symptom group (est = 0.08, p < 0.65). Figure 3b presents the group-based trajectory modeling using a score based on immunotherapy-specific symptoms (e.g., rash, diarrhea). It resulted in 33% of patients belonging to the high symptom group. Similarly, there were no significant increase in symptom during this period for either the high symptom burden group (est = − 0.001, p < 0.98) or the low burden symptom group (est = 0.08, p < 0.43). Symptom trajectories are relatively stable over 9 weeks of treatment with pembrolizumab. Patients with high symptom burden at baseline continued to have high symptom burden during treatment with pembrolizumab, and patients with low symptom burden at baseline entry into the clinical trial continue to have low symptom burden over the course of 9 weeks of treatment with pembrolizumab.
Discussion
To our knowledge, the present study is the first to examine longitudinally patient-reported symptoms in patients with rare cancers in a clinical trial testing an immune checkpoint inhibitor. Although patient-reported outcomes have been included in immunotherapy trials, this study provides a very frequent (every week) examination of symptom burden associated with immunotherapy compared to assessments done mostly at imaging visits (every 8–9 weeks). Knowing the symptom trajectories associated with the use of immunotherapy contributes to our understanding of symptom benefit and whether patients can continue with their cancer treatment. Tolerability of treatment using patient-reported outcomes is an important component of drug evaluation1.
The finding in the present study that symptom trajectories stayed relatively stable over 9 weeks of treatment with pembrolizumab is parallel to observations by Lacey et al.17 that treatment with pembrolizumab in patients with metastatic melanoma was accompanied by low symptom burden and that changes in symptoms longitudinally were not seen regardless of whether or not patients’ usual care was supplemented with a supportive care intervention. However, the KEYNOTE-087 study in patients with relapsed/refractory classical Hodgkin lymphoma who received pembrolizumab as monotherapy reported improvements in overall quality of life from baseline to weeks 12–24 of treatment with pembrolizumab18. The KEYNOTE-087 study also showed improvements during treatment with pembrolizumab in symptoms assessed (fatigue, nausea and vomiting, pain, dyspnea, insomnia, constipation and diarrhea). Also, a study by Barlesi et al.19 in patients with advanced non-small cell lung cancer (NSCLC) receiving pembrolizumab or docetaxel in a randomized trial found that pembrolizumab was linked to better quality of life scores than docetaxel. Barlesi et al.19 reported nominally significant improvement in many EORTC-QLQC30 symptom domains with pembrolizumab, and nominally significant worsening with docetaxel.
The strengths of the present study include the unique study population of patients with rare cancers participating in a Phase II clinical trial, and the systematic and longitudinal collection of patient-reported outcomes data focused on symptoms in a clinical trial testing an immune checkpoint inhibitor, and that all patients in this Phase II trial received the same dose of pembrolizumab. Weaknesses include a relatively small sample size of 53 patients, and a relatively brief follow-up period of 9 weeks. Yet, this study offers valuable insights into weekly patient-reported symptoms during the first nine weeks of treatment with pembrolizumab in patients with rare tumors. Although symptoms are stable over the first nine weeks, our group-based trajectory analyses showed that there are subgroups of patients who have consistently high symptom burden. The proportion of patients experiencing high symptom burden changes depending on the type of symptoms. For this study, it was 43% based on pain, fatigue, lack of appetite, sleep disturbance and feeling drowsy but was only 33% based on immunotherapy specific symptoms such as rash and diarrhea. Our examination of associations of baseline demographic and clinical characteristics with symptom burden grouping yielded no significant results. Similarly, our examination of differences in symptom ratings by treatment response (objective response: yes/no) resulted in no significant result. Because of the limited sample size, these analyses were inconclusive. Future studies with larger sample sizes can identify demographic and clinical characteristics of those patients with high symptom burden that may allow personalized symptom management.
In summary, our results suggest it is feasible to collect PRO data in patients with rare cancers enrolled in a Phase II trial of an immune checkpoint inhibitor. Our findings indicate that symptom trajectories in patients with rare cancers receiving pembrolizumab remain relatively stable over the first 9 weeks of treatment and that baseline symptom groupings are associated with the trajectory of symptom burden over 9 weeks of treatment with pembrolizumab as monotherapy. Our results may inform clinicians about symptom intervention needs, and provide a benchmark in designing future symptom intervention clinical trial. These findings need to be investigated further in larger samples with longer duration of follow-up.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request according to available guidelines at the time of request.
References
Kluetz, P. G. et al. Informing the tolerability of cancer treatments using patient-reported outcome measures: Summary of an FDA and critical path institute workshop. Value Health. 21(6), 742–747 (2018).
Schnipper, L. E. et al. American society of clinical oncology statement: A conceptual framework to assess the value of cancer treatment options. J. Clin. Oncol. 33(23), 2563–2577 (2015).
Basch, E. Patient-reported outcomes: an essential component of oncology drug development and regulatory review. Lancet Oncol. 19(5), 595–597 (2018).
Kluetz, P. G., O’Connor, D. J. & Soltys, K. Incorporating the patient experience into regulatory decision making in the USA, Europe, and Canada. Lancet Oncol. 19(5), e267–e274 (2018).
Di Maio, M., Basch, E., Bryce, J. & Perrone, F. Patient-reported outcomes in the evaluation of toxicity of anticancer treatments. Nat. Rev. Clin. Oncol. 13(5), 319–325 (2016).
Mendoza, T. R. Symptoms as patient-reported outcomes in cancer patients undergoing immunotherapies. Immunotherapy 995, 165–182 (2018).
Naing, A. Being realistic and optimistic in curing cancer. J. Immunother. Precis. Oncol. 1(2), 53–55 (2018).
Socinski, M. A. Incorporating immunotherapy into the treatment of non-small cell lung cancer: Practical guidance for the clinic. Semin Oncol. 42(Suppl 2), S19-28 (2015).
Weber, J. S., Yang, J. C., Atkins, M. B. & Disis, M. L. Toxicities of immunotherapy for the practitioner. J. Clin. Oncol. 33(18), 2092–2099 (2015).
Naing, A. et al. Strategies for improving the management of immune-related adverse events. J. Immunother. Cancer. 8(2), e001754 (2020).
Marabelle, A. et al. Efficacy of pembrolizumab in patients with noncolorectal high microsatellite instability/mismatch repair-deficient cancer: Results from the phase II KEYNOTE-158 study. J. Clin. Oncol. 38(1), 1–10 (2020).
Naing, A., Meric-Bernstam, F., Stephen, B., Karp, D. D., Hajjar, J., Ahnert, J. R., & Habra, M. A. Phase 2 study of pembrolizumab in patients with advanced rare cancers. J. Immunother. Cancer 8(1) (2020).
Mendoza, T. et al. Evaluating the psychometric properties of the immunotherapy module of the MD anderson symptom inventory. J. Immunother. Cancer. 8(2), e000931 (2020).
Oken, M. M. et al. Toxicity and response criteria of the eastern cooperative oncology group. Am. J. Clin. Oncol. 5(6), 649–655 (1982).
Cleeland, C. S. et al. Assessing symptom distress in cancer patients: The M.D. anderson symptom inventory. Cancer 89(7), 1634–1646 (2000).
Cleeland, C. S. et al. Dimensions of the impact of cancer pain in a four country sample: New information from multidimensional scaling. Pain 67(2–3), 267–273 (1996).
Lacey, J. et al. A supportive care intervention for people with metastatic melanoma being treated with immunotherapy: A pilot study assessing feasibility, perceived benefit, and acceptability. Support. Care Cancer 27(4), 1497–1507 (2019).
von Tresckow, B. et al. Patient-reported outcomes in KEYNOTE-087, a phase 2 study of pembrolizumab in patients with classical Hodgkin lymphoma. Leuk. Lymphoma 60(11), 2705–2711 (2019).
Barlesi, F. et al. Health-Related quality of life in KEYNOTE-010: A phase II/III study of pembrolizumab versus docetaxel in patients with previously treated advanced, programmed death ligand 1-expressing NSCLC. J. Thorac. Oncol. 14(5), 793–801 (2019).
Acknowledgements
We thank the patients and their families and caregivers for participating in the study. Trial Registration ClinicalTrials.gov, NCT02721732, Registered March 29, 2016, https://clinicaltrials.gov/ct2/show/NCT02721732. For any questions, please reach out to Dr. Tito Mendoza (tito.mendoza@nih.gov) who is currently with the Office of Patient-Centered Outcomes Research, Center for Cancer Research, National Cancer Institute, National Institute of Health. However, this work was performed while he was at MD Anderson Cancer Center.
Funding
Preparation of this manuscript was funded in part by RO1CA242565 (Mendoza, Hong and George). Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc. provided the study drug and funded the study. Support was also provided by the National Institutes of Health/National Cancer Institute under award number P30CA016672 (MD Anderson Cancer Center Support grant AIM and Biostatistics).
Author information
Authors and Affiliations
Contributions
Conception and design: T.M., C.B.P., A.N. Provision of study materials/patients: D.S.H., E.D., S.P., A.M.T., T.A.Y., V.S., F.J., S.F., S.A.P., J.R.A., D.D.K., F.M.B., A.N. Technical and administrative support: A.N. Collection and assembly of data: T.M., B.S., L.C., E.R., J.G. Data analysis and interpretation: T.M., C.B.P., A.S., M.A., G.G., C.C., A.N. Drafting the manuscript: T.M., B.S., G.G., A.N. Critical review and Final approval of manuscript: All authors. Accountable for all aspects of the work: All authors.
Corresponding author
Ethics declarations
Competing interests
TM reports personal fees from Bristol Myers Squib, personal fees from Amgen, outside the submitted work; DSH reports grants from AbbVie, grants from Adaptimmune, grants from Adlai-Nortye, grants from Amgen, grants from Astra-Zeneca, grants from Bristol-Myers Squibb, grants from Daiichi-Sankyo, grants from Deciphera, grants from Eisai, grants from Endeavor, grants from Erasca, grants from F. Hoffman-La Roche , grants from Fate Therapeutics, grants from Genentech, grants from Genmab, grants from Ignyta, grants from Infinity, grants from Kite, grants from Kyowa Kirin, grants from Lilly, grants from LOXO, grants from Merck, grants from Medimmune, grants from Mirati, grants from Mologen, grants from Navier, grants from NCI-CTEP, grants from Novartis, grants from Numab, grants from Pfizer, grants from Pyramid Bio, grants from Seagen, grants from Takeda, grants from TCR2, grants from Teckro, from Turning Point Therapeutics, from Verstatem, from VM Oncology, during the conduct of the study; other from Bayer, other from Genmab, from AACR, from ASCO, from SITC, personal fees and other from Telperian, personal fees from Molecular Match , other from Oncoresponse , personal fees from Adaptimmune, personal fees from Alpha Insights, personal fees from Acuta, personal fees from Alkermes , personal fees from Amgen, personal fees from Aumbiosciences, personal fees from Axiom, personal fees from Baxter, personal fees from Bayer, personal fees from Boxer Capital, personal fees from BridgeBio, personal fees from COR2ed, personal fees from COG, personal fees from ECOR1, personal fees from Genentech, personal fees from Gilead, personal fees from GLG, personal fees from Group H, personal fees from Guidepoint, personal fees from HCW Precision, personal fees from Immunogen, personal fees from Infinity, personal fees from Janssen, personal fees from Liberium, personal fees from Medscape, personal fees from Numab, personal fees from Oncologia Brasil, personal fees from Pfizer, personal fees from Pharma Intelligence, personal fees from POET Congress, personal fees from Prime Oncology, personal fees from Seattle Genetics, personal fees from ST Cube, personal fees from Takeda, personal fees from Tavistock, personal fees from Trieza Therapeutics, personal fees from Turningpoint, personal fees from WebMD, personal fees from Ziopharma, outside the submitted work; ED reports grants from Bayer HealthCare Pharmaceuticals Inc, grants from Immunocore LTD, grants from Amgen, grants from NCI, grants from Aileron Therapeutics, grants from Compugen Ltd, grants from TRACON Pharmaceuticals Inc, grants from Unum Therapeutics, grants from Immunomedics, grants from BOLT Therapeutics, grants from Aprea Therapeutics, grants from Bellicum Pharmaceuticals, grants from PMV Pharma, grants from Triumvira, grants from Seagen Inc, grants from Mereo BioPharma 5 Inc, grants from Sanofi, grants from Astex Therapetics, during the conduct of the study; personal fees and other from BOLT Therapeutics, personal fees and other from Catamaran Bio, outside the submitted work; SP receives Research/Grant Funding through the institution from the following sources: AbbVie, Argule, Bristol-Myers Squibb,Eli Lilly, Five Prime Therapeutics, Glaxo Smith Kline, Holy Stone Healthcare Co., InnoPharmax Inc., Ipsen, Mirati Therapeutics, Inc., Novartis, Onco Response,Parexel International LLC, Red Hill Biopharma Ltd.,Rgenix, Sanofi US Services Inc., Sanofi-Aventis, Xencor, other from Financial Relationship/Speakers Bureau ConsultantTyme Inc.4D-Pharma outside the submitted work; TAY reports grants from Repare, AstraZeneca, Artios, Bayer, Beigene, BioNTech, BMS, Clovis, Constellation, Cyteir , Eli Lilly, EMD Serono, Forbius, F-Star, Artios, GlaxoSmithKline, Genentech, Haihe, ImmuneSensor, Ionis, Ipsen, Jounce, Karyopharm, KSQ, Kyowa, Merck, Novartis, Pfizer, Ribon Therapeutics, Regeneron, Rubius, Sanofi, Scholar Rock, Seattle Genetics, Tesaro and Vivace, personal fees from Repare, AstraZeneca, Almac, Aduro, Artios, Athena, Atrin, Axiom, Bayer, Bristol Myers Squibb, Calithera, Clovis, Cybrexa, EMD Serono, F-Star, GLG, Guidepoint, Ignyta, I-Mab, ImmuneSensor, Jansen, Merck, Pfizer, Roche, Schrodinger, Seattle Genetics, Varian, Zai Labs and ZielBio, outside the submitted work; AS reports personal fees from PsiOxus Therapeutics, personal fees from Enanta Pharmaceuticals, outside the submitted work; MA reports grants and other from Nektar therapeutics, grants and other from GSK, grants from Novartis, grants and other from Shattuck Lab, grants from Merck, grants and other from BMS, other from AstraZenecca, grants from Genentech, grants from Jounce therapeutics, grants from Eli Lilly, grants from Gilead, outside the submitted work; VS reports grants from Roche/ Genentech, grants from Novartis, grants from Bayer, grants from GlaxoSmithKline, grants from Nanocarrier, grants from Vegenics, grants from Celgene, grants from Northwest Biotherapeutics, grants from Berghealth, grants from Incyte, grants from Fujifilm, grants from Pharmamar, grants from D3, grants from Pfizer, grants from Multivir, grants from Amgen, grants from Abbvie, grants from Alfa-sigma, grants from Agensys, grants from Boston Biomedical, grants from Idera Pharma, grants from Inhibrx, grants from Exelixis, grants from Blueprint medicines, grants from Loxo oncology, grants from Medimmune, grants from Altum, grants from Dragonfly therapeutics, grants from Takeda, grants from National Comprehensive Cancer Network, grants from NCI-CTEP , grants from Turning point therapeutics, grants from Boston Pharmaceuticals, during the conduct of the study; other from Novartis, other from Pharmamar, other from ASCO, other from ESMO, other from Helsinn, other from Incyte, other from Helsinn, other from LOXO Oncology/ Eli Lilly, other from R-Pharma US, other from INCYTE, other from QED pharma, other from Medimmune, other from Novartis, other from Relay Therapeutics, other from Roche, other from Medscape, outside the submitted work; FJ reports grants from Astex, Novartis, BioMed Valley Discoveries, Fore Bio, Deciphera, Bristol-Myers Squibb, Asana, Ideaya Biosciences, Sanofi, Merck, F-star, JSI Innopharm, Bioxcel, Lilly, Bicara, PureTech Health, FujiFilm Pharmaceuticals, Sotio, Synlogic, NextCure, Hutchinson Medipharma, other from Ideaya Biosciences, Synlogic, Sotio, Puretech Health, Deciphera, Crown Bioscience, Asana, Fore Bio, Novartis, Bicara, and PegaOne, personal fees from Mersana Therapeutics, Flame Bio, Cardiff Oncology, MedinCell, and Immunomet has ownership interests in Cardiff Oncology, Monte Rosa Therapeutics, other from Monte Rosa Therapeutics, outside the submitted work; SF reports grants from NCI/NIH P30CA016672—Core Grant (CCSG Shared Resources), other from Abbisko, other from BeiGene, other from BioAtla, LLC., other from Boehringer Ingelheim, other from Eli Lilly & Co., other from Green2Bio, Inc., other from Hookipa Biotech, other from IMV, Inc., other from Innovent Biologics, Co., Ltd., other from K-Group Beta, other from Lyvgen Biopharm, Co., Ltd., other from MacroGenics, other from Millennium Pharmaceuticals. Inc., other from Nerviano Medical Sciences, other from NeuPharma, Inc., other from Ningbo NewBay Techology Develoment Co., Ltd., other from Novartis, other from NovoCure, other from Parexel International, LLC, other from PureTech Health, LLC, other from Sellas Life Sciences Group, other from Soricimed Biopharma, Inc., other from SQZ Biotechnologies, other from Sumitomo Dainippon, other from Taiho Oncology and NCCN, other from Treadwell Therapeutics, other from Turnstone Biologics, other from Tyligand Bioscience, Ltd., outside the submitted work; SPP reports other from AbbVie, Inc., other from ABM Therapeutics, Inc., other from Acepodia, Inc., other from Alkermes, other from Aminex Therapeutics, other from Amphivena Therapeutics, other from Biomari Pharmaceutical, Inc., other from Boehringer Ingelheim, other from Bristol Myers Squib, other from Cerulean Pharma, Inc., other from Chugai Pharmaceutical Co., Ltd., other from Curis, Inc., other from Cyclacel Pharmaceuticals, other from Daiichi Sankyo, Inc., other from Eli Lilly, other from ENB Therapeutics, other from Five Prime Therapeutics, other from F-Star Beta Limited, other from F-Star Therapeutics, Limited, other from Gene Quantum, other from Genmab A/S, other from GlaxoSmithKline, other from Helix BioPharma Corp., other from HiberCell, Inc., other from Immunomedics, Inc., other from Incyte Corp., other from Jacobio Pharmaceuticals Co., Ltd., other from Lytix Biopharma AS, other from Medimmune, LLC., other from Medivation, Inc., other from Merck Sharp and Dohme Corp., other from Novartis Pharmaceuticals, other from Pieris Pharmaceuticals, Inc., other from Pfizer, other from Principia Biopharma, Inc., other from Puma Biotechnology, Inc., other from Rapt Therapeutics, Inc., other from Seattle Genetics, other from Silverback Therapeutics, other from Synologic Therapeutics, other from Taiho Oncology, other from Tesaro, Inc., other from TransThera Bio, grants from NCI/NIH P30CA016672—Core Grant (CCSG Shared Resources), outside the submitted work; and Worked as a consultant for CRC Oncology; JR reports personal fees from Novartis, Eli Lilly, Orion Pharmaceuticals, Servier Pharmaceuticals, Peptomyc, Merck Sharp & Dohme, Kelun Pharmaceuticals/Klus Pharma, Spectrum Pharmaceuticals, Inc., Pfizer, Roche Pharmaceuticals, Ellipses Pharma, Certera, Bayer, Molecular Partners, NovellusDX, IONCTURA SA, Kisoji Biotechnology, Inc., grants from Bayer, Novartis, Blueprint Medicines, Spectrum Pharmaceuticals, Tocagen, Symphogen, BioAlta, Pfizer, GenMab, CytomX, Kelun-Biotech, Takeda-Millenium, GalxoSmithKline, Ipsen, other from ESMO, Department of Defense, Merck Sharp & Dohme, Louisiana State University, Kelun Pharmaceuticals/Klus Pharma, Huntsman Cancer Institute, Cancer Core Europe, Karolinska Cancer Institute, King Abdullah International Medical Research Center, Bayer, WIN Consortium, Janssen, Molecular Partners, other from European Journal of Cancer, VHIO/Ministero De Empleo Y Seguridad Social, Chinese University of Hong Kong, SOLTI, Elsevier, GlaxoSmithKline, outside the submitted work; DK receives Grant/Research Funding through the institution from the following sources: Phosplatin Therapeutics, Pfizer,Arcus, Arqule, Bristol-Myers Squibb,Eli Lilly, Five Prime Therapeutics, Glaxo Smith Kline, Genmab, Holy Stone Healthcare Co., Ipsen,Mirati Therapeutics, Inc., Novartis, Onco Response, Red Hill Biopharma Ltd., Rgenix, Sanofi-Aventis, Xencor, Astellas, Janssen, Affigen, Black Beret Life Sciences, NIH Clinical Translational Science Award Grant; CSC reports a patent on MD Anderson Symptom Inventory; FMB reports personal fees from AbbVie, Aduro BioTech Inc., Alkermes, AstraZeneca, DebioPharm, eFFECTOR Therapeutics, F. Hoffman-La Roche Ltd., Genentech Inc., IBM Watson, Infinity Pharmaceuticals, Jackson Laboratory, Kolon Life Science, Lengo Therapeutics, OrigiMed, PACT Pharma, Parexel International, Pfizer Inc., Samsung Bioepis, Seattle Genetics Inc., Tallac Therapeutics, Tyra Biosciences, Xencor, Zymeworks, personal fees from Black Diamond, Biovica, Eisai, Immunomedics, Inflection Biosciences, Karyopharm Therapeutics, Loxo Oncology, Mersana Therapeutics, OnCusp Therapeutics, Puma Biotechnology Inc., Seattle Genetics, Silverback Therapeutics, Spectrum Pharmaceuticals, Zentalis, grants from Aileron Therapeutics, Inc. AstraZeneca, Bayer Healthcare Pharmaceutical, Calithera Biosciences Inc., Curis Inc., CytomX Therapeutics Inc., Daiichi Sankyo Co. Ltd., Debiopharm International, eFFECTOR Therapeutics, Genentech Inc., Guardant Health Inc., Klus Pharma, Takeda Pharmaceutical, Novartis, Puma Biotechnology Inc., Taiho Pharmaceutical Co., personal fees from Chugai Biopharmaceuticals, outside the submitted work; AN reports research support and non-financial support from Merck Sharp & Dohme Corp., grants from NCI/NIH, research support from The University of Texas MD Anderson Cancer Center, during the conduct of the study; grants from NCI, EMD Serono, MedImmune, Healios Onc. Nutrition, Atterocor/Millendo, Amplimmune, ARMO BioSciences, Karyopharm Therapeutics, Incyte, Novartis, Regeneron, Merck, Bristol-Myers Squibb, Pfizer, CytomX Therapeutics, Neon Therapeutics, Calithera Biosciences, TopAlliance Biosciences, Eli Lilly, Kymab, PsiOxus, Arcus Biosciences, NeoImmuneTech, ImmuneOncia, Surface Oncology, Monopteros Therapeutics, BioNTech SE, Seven & Eight Biopharma, and SOTIO Biotech AG, personal fees from CytomX Therapeutics, Novartis, Genome & Company, OncoSec KEYNOTE-695, Kymab, STCube Pharmaceuticals, and Deka Biosciences, grants from ARMO BioSciences outside the submitted work. AN Spouse receives grants from Immune Deficiency Foundation, Jeffery Modell Foundation and chao physician-scientist, and Baxalta, grants from Takeda, CSL, Behring, Horizon, and Pharming, outside the submitted work. CBP, BS, GG, LC, ER, and JG, declare no competing interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mendoza, T.R., Hong, D.S., Peterson, C.B. et al. Patient-reported symptom burden in patients with rare cancers receiving pembrolizumab in a phase II Clinical Trial. Sci Rep 12, 14367 (2022). https://doi.org/10.1038/s41598-022-16588-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-16588-3
This article is cited by
-
Advancing cancer immunotherapy: from innovative preclinical models to clinical insights
Scientific Reports (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.