Abstract
Several artificial intelligence algorithms have been proposed to help diagnose glaucoma by analyzing the functional and/or structural changes in the eye. These algorithms require carefully curated datasets with access to ocular images. In the current study, we have modeled and evaluated classifiers to predict self-reported glaucoma using a single, easily obtained ocular feature (intraocular pressure (IOP)) and non-ocular features (age, gender, race, body mass index, systolic and diastolic blood pressure, and comorbidities). The classifiers were trained on publicly available data of 3015 subjects without a glaucoma diagnosis at the time of enrollment. 337 subjects subsequently self-reported a glaucoma diagnosis in a span of 1–12 years after enrollment. The classifiers were evaluated on the ability to identify these subjects by only using their features recorded at the time of enrollment. Support vector machine, logistic regression, and adaptive boosting performed similarly on the dataset with F1 scores of 0.31, 0.30, and 0.28, respectively. Logistic regression had the highest sensitivity at 60% with a specificity of 69%. Predictive classifiers using primarily non-ocular features have the potential to be used for identifying suspected glaucoma in non-eye care settings, including primary care. Further research into finding additional features that improve the performance of predictive classifiers is warranted.
Similar content being viewed by others
Introduction
Glaucoma is a progressive optic neuropathy resulting in the loss of retinal ganglion cells; if untreated it can result in complete blindness. It is the leading cause of irreversible blindness in the world. At present, it affects approximately 70 million people, with the number projected to grow to about 112 million by 20401. Although the visual impairment caused by glaucoma is irreversible, early detection and treatment of the disease can reduce the risks of permanent vision loss2. Unfortunately, this is hampered by the asymptomatic nature of glaucoma3 and its complex, resource-intensive, and subjective diagnostic process4,5,6,7. Artificial intelligence (AI)-based approaches may enable the construction, validation, and implementation of predictive models to identify individuals who are at high risk of developing glaucoma, in settings that do not necessarily have access to ophthalmic imaging devices (e.g. primary care) and coordinate their care to ophthalmology.
In recent years, several AI-based approaches have been explored for the diagnosis of ophthalmic pathologies such as diabetic retinopathy8,9, macular edema10,11, and keratoconus12. Some of these efforts have resulted in new medical devices. In 2018, IDx-DR was approved by the US Food and Drug Association as the first fully autonomous AI-based diabetic retinopathy diagnostic system13. Several AI studies have attempted to interpret the structural and functional patterns manifesting in the eye for the prognosis and diagnosis of glaucoma14,15,16,17,18,19,20,21,22,23,24,25. Artificial neural networks (ANN) and machine learning classifiers have been used on functional data, such as visual fields, to identify patterns of glaucomatous progression earlier than more conventional methods14,15,16,17. The advent of deep learning has allowed the use of retinal imaging such as color fundus photographs (CFPs)18,19,20,21,22 and macular optical coherence tomography (OCT) images23,24,25 to extract structural features to differentiate glaucomatous damage. Compared to conditions such as diabetic retinopathy, where clinically feasible AI-based diagnostic technologies have already been adopted, it may be more difficult to develop such tools for glaucoma, owing to the significant variation in the appearance of the optic discs. The need for carefully chosen, large, and diverse training datasets to achieve high diagnostic accuracy adds to this challenge. The performance of glaucoma-specific models depends on the quality and number of images (> 100,000), making it a time consuming and expensive process26. Furthermore, repeated visual field tests are required to account for their inherent subjectivity, making them a major part of the workload being placed on hospital eye services22,27.
Relatively few AI-based studies have focused on developing predictive models for glaucoma without using visual fields, CFPs, or OCT images. Leveraging the wide adoption of electronic health records (EHR), Baxter et al.28 used machine learning classifiers to identify high risk patients with open angle glaucoma (OAG) requiring surgery within 6 months. Mehta et al.29 trained multiple ensemble models, each using a different set of features, to differentiate between glaucomatous and healthy eyes. One of those models used demographic, systemic, and ocular data to make these classifications. Similarly, Tielsch et al.30 fit logistic regression models to a population-based survey to screen for glaucoma, using demographic and other known risk factors. These prior studies have shown the potential for AI-based models to be used for managing glaucoma more effectively, making informed referrals to ophthalmologists, implementing more efficient population-based glaucoma screening, and developing intelligent self-monitoring devices. However, since the models by Baxter et al. and Mehta et al. are not trained on features from an undiagnosed population, they cannot be applied directly to predict glaucoma in the general population outside of those already actively managed by an eye care provider. On the other hand, although Tielsch et al. have trained their model on an undiagnosed population, they have reported very low predicted probabilities; likely a direct consequence of the dataset used.
In the current study, we have trained the classifiers on a sufficiently large cohort of subjects with a negative glaucoma diagnosis at the time of enrollment, such that it could be representative of the general population. Some of the subjects subsequently self-reported glaucoma. Different machine learning classifiers were evaluated on their ability to identify these subjects based on a combination of their demographic, systemic, ophthalmic, and comorbidity information taken at the time of enrollment. The goal was to explore the use of easily available data to inform referral decisions to eye care from primary care settings, without the use of expensive and/or time-consuming data such as visual fields or retinal images.
Methods
The National Institutes of Health’s (NIH) Age-Related Eye Disease Study (AREDS) database was used to develop and evaluate the machine learning classifiers. The AREDS was a 12-year, multi-center, prospective study carried out to determine the risk factors associated with age-related macular degeneration (AMD)31. Anonymized natural history data of subjects was made publicly available by the NIH for research purposes. The corresponding author was granted access to the AREDS data by the National Eye Institute Data Access Committee, NIH and the analysis was conducted in agreement with the approved research use statement (data access request no. #89148–1). The AREDS was adherent to the tenets of the Declaration of Helsinki and was compliant with the Health Insurance Portability and Accountability Act32. For the present study, non-genetic data was used, which consisted of demographic, systemic, ocular (IOP), and co-morbidity information for enrolled subjects. Glaucoma was established through self-report, in which subjects were annually queried whether they had been diagnosed with glaucoma by an eye care provider. Subjects with glaucoma were determined based on those who selected ‘Yes’ from a predefined list of answers to the question ‘Has a doctor ever told you that you have glaucoma?’ The earliest diagnosis was recorded within a year of the start and the latest at over 12 years. While limited due to the lack of a “confirmed” diagnosis, the AREDS data provides a unique opportunity to build predictive models using data of non-glaucomatous subjects at the time of enrollment, some of whom subsequently self-reported new onset of glaucoma.
Information was extracted from the AREDS database for subjects who had multiple follow-up visits. The models were based on demographic features (age, gender, and race), systemic features (body mass index (BMI), systolic and diastolic blood pressure), a single ocular feature (IOP in the right and the left eye), and comorbidities (diabetes, arthritis, and AMD). The blood pressure readings were taken by a certified examiner using a mercury sphygmomanometer33. IOP for the AREDS participants was measured using an applanation tonometer or a pneumatonometer by experienced professionals33, which is representative of how IOP is measured during eye exams as part of primary eye care34. There were 7 non-glaucomatous subjects with missing entries for either IOP or BMI. Due to the relatively low number of missing values, imputation was not performed and these cases were removed from the dataset. A statistical quantitative description of the features is shown in Tables 1 and 2. The total number of subjects in the final database was 3,015, all of whom were non-glaucomatous when the information highlighted in Tables 1 and 2 was recorded. In the subsequent follow-up visits, 337 subjects self-reported to have been diagnosed with glaucoma (positive class) which left 2,678 non-glaucomatous (negative class) subjects at the end of the study period.
Further data preprocessing was carried out in the steps highlighted below:
Encoding categorical data
The pandas35,36 library in python was used for initial data processing. Ordinal encoding was used for the AMD categorical variable where the integer values (1–4 in increasing order of severity) had a natural ordered relationship. For all the other categorical variables (gender, race, presence of diabetes and arthritis), since no such ordinal relationship existed, dummy encoding was implemented using the one-hot encoder.
Train test split
To estimate the generalization error of the classifiers, a nested cross-validation strategy was applied. Five randomly generated splits ensured that 80% of the data was used for training and the remaining 20% was used for testing each of the fitted classifiers. The train and test sets were stratified to have a similar ratio of glaucoma to non-glaucoma subjects. Grid search was performed for hyperparameter tuning by using a fivefold cross-validation on the training set. The best hyperparameters identified through the grid search process were then used to evaluate how the classifiers performed on the test set. The model metrics are reported as a mean over all the executions for evaluating and comparing the performance of each classifier.
Class imbalance
The current dataset had 11% positive cases and 89% negative cases, making it an imbalanced dataset. This might result in biased classifiers that have poor predictive capabilities, specifically for the minority class. To address class imbalance, synthetic data was generated using the synthetic minority over-sampling technique (SMOTE)37. The algorithm works by generating new instances of the minority class rather than creating copies of the existing samples. Synthetic examples are introduced along the line segments joining each sample of the minority class and any/all of its nearest neighbors, determined by the Euclidean distance between them.
Model training
The Scikit-learn38 and the Keras39 libraries in Python were used to build the classifiers. The classifiers included a linear method (logistic regression), a non-linear method (support vector machines), and an ensemble method (Adaptive boosting). The performance of different classifiers is usually evaluated using metrics such as accuracy, precision, recall, specificity, F1 score, and area under the curve (AUC) for the receiver operating characteristic (ROC) and precision-recall curves. With imbalanced data, the regular measures of performance such as accuracy are often misleading. Recall (i.e., sensitivity) measures the ability of the model to correctly identify the positive class (i.e., glaucomatous subjects). Precision (i.e., positive predictive value) indicates the proportion of correct positive predictions. Since there is usually a tradeoff between precision and recall, their harmonic mean, called the F1 score is often used. In the current study, the classifiers’ hyperparameters are optimized such that they maximize the F1 score. A grid search technique was used in the inner loop of the nested cross-validation to identify the optimized hyperparameters. A brief description of the setup for each model and the hyperparameters chosen via cross-validation are given below:
Logistic regression
Logistic regression is a linear model for classification that uses the logistic (sigmoid) function to estimate the probability that a sample with given features belongs to the default class (Y = 1). The probability predictions are transformed into a binary output (0 or 1) using a threshold of 0.5 in scikit-learn. The logistic regression classifier was set up using the limited-memory Broyden–Fletcher–Goldfarb–Shanno (LBFGS) solver. L2 regularization was used to prevent overfitting and the inverse regularization coefficient, C, was set at 0.001. The maximum number of iterations for the solver to converge was 10,000. Standardization of the dataset was carried out so that all features are approximately centered around zero and have a unit variance. This ensures that the regularization is applied equally to all the features.
Support vector machines
The support vector machine (SVM) classifier determines a hyperplane that directly classifies samples into one class or the other. A non-linear decision function can be determined using a kernel function that implicitly maps the features into a high-dimensional space. In the present study, a radial basis function kernel was used, and the inverse regularization coefficient, C, was set at 0.001. The kernel coefficient, γ, represents the inverse of the radius of influence of samples selected by the model as support vectors, and was set as 0.0001. Similar to the setup of the logistic regression classifier, the SVM classifier is not scale invariant and the features thus were standardized prior to training.
Adaptive boosting
Adaptive Boosting (AdaBoost) fits a sequence of weak learners such as decision trees, with a single internal node (decision stumps), on data that is repeatedly modified by assigning weights. At each boosting iteration, the examples that are misclassified by the boosted model at the previous step are assigned a higher weight, while the weights for the correctly classified examples are decreased. Each subsequent weak learner thereby focusses more on correctly classifying the examples that are missed by the previous ones. A weighted majority vote is taken from all the weak learners to determine the final classification. 200 decision stumps were used in the current model. The learning rate controls the contribution of the new decision stump to the existing model and is suggested to be set to small values (< 0.1)40. In the current model the learning rate is set as 0.01.
A permutation feature importance technique was used to determine the predictive power of the features used. The technique was set up to calculate the drop in the F1 score when a single feature value was randomly shuffled41. This results in breaking the pattern between the feature and the target class, and the drop in F1 score is indicative of the importance of that feature to the model. If a particular feature is important to the model, randomly shuffling its values will deteriorate the performance of the model, while doing the same to a relatively less important feature would not adversely affect the model’s performance. Permutation feature importance was preferred over the impurity-based ranking technique used in decision tree classifiers, as it is model agnostic and is unbiased towards features exhibiting high cardinality (most numerical features)42.
Results
Table 3 shows the performance of the classifiers based on the primary outcome measures: sensitivity (or recall), specificity, F1 score, accuracy, and area under the precision-recall curve. As mentioned earlier, sensitivity is a measure of the false-negatives, and F1 score is a harmonic mean of the sensitivity and precision. Specificity is a measure of the ability to correctly classify as negative (i.e., non-glaucomatous) those without the disease. As seen in Table 3, all three machine learning classifiers perform similarly. This is highlighted in Fig. 1, which shows the average precision and recall curves for all classifiers relative to one from a dummy classifier that makes random classifications. The precision-recall curve is more informative than the ROC curve when evaluating models with class imbalance43. The area under the precision-recall curve for all three classifiers is greater than the dummy classifier: 0.30, 0.29, and 0.28 for AdaBoost, SVM, and logistic regression, respectively. Classifiers that have a greater area under the precision-recall curve compared to that of the dummy classifier are indicative of their learnt ability to identify patterns in the data.
Traditionally, glaucoma screening programs and referrals for comprehensive eye examination have been made on the basis of IOP, with individuals having IOP > 21 mm Hg considered to be at high risk for glaucoma30,44,45. Table 3 also shows the performance of a similar criterion applied on the current dataset. Subjects with IOP > 21 mm Hg in either eye were predicted to have glaucoma. With the traditional IOP criterion, the sensitivity is very poor when compared to the machine learning classifiers, as reported in Table 3. Based on the sensitivity, machine learning classifiers are likely to identify more than twice as many subjects with glaucoma from the current dataset.
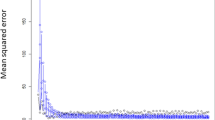
The predictive capabilities for the features used for classification were evaluated using the permutation feature importance technique. Figure 2 shows the drop in the F1 score for the 3 classifiers as each feature was permuted. The features which contribute most to the F1 score are IOP and age. The age of the patient has more predictive capabilities in case of logistic regression and support vector machine as compared to AdaBoost.
Permutation feature importance applied to each classifier: (a) Logistic regression, (b) Support vector machine, and (c) Adaptive boosting (AdaBoost). Mean decrease in F1 score is shown for each feature: age, systolic and diastolic blood pressure, gender (male), body mass index (BMI), intraocular pressure (IOP) in the right eye (RE) and left eye (LE), age-related macular degeneration (AMD) category, race (black, Hispanic, Asian, and other), and presence of diabetes and arthritis.
Discussion
The classifiers were trained and evaluated on the AREDS dataset, which had subjects who were all non-glaucomatous when their baseline features were recorded. Self-reporting of glaucoma diagnosis is a limitation; it may be subject to inaccuracies due to the lack of a widely accepted method of confirming diagnosis, the associated potential for misdiagnosis from a provider, and/or misunderstanding of a diagnosis (or lack thereof) by the patient. However, self-reported glaucoma status has been regularly used in previous studies46,47,48, and its usefulness and performance has been explored49.
The AREDS dataset has certain advantages that address some of the sources of bias that often appear in AI-based studies50. First, the final database has 3,015 subjects, which is a relatively large cohort which results in more realistic performance of the classifiers. Second, unlike other studies where the data is retrieved from glaucoma clinics in which there is a higher proportion of glaucoma cases, the current study has 337 glaucomatous cases and 2,678 non-glaucomatous cases, which represents a more likely real-world scenario. Third, the prevalence of comorbidities such as diabetes, arthritis, and AMD are taken into consideration as some people would most likely present with multiple diseases. AI-based studies that use structural and functional data14,19, generally consider an otherwise-healthy but glaucomatous population, but patients often present with multiple conditions. This approach would likely help the classifiers generalize better to real world data. The classifiers were trained on subjects’ age, gender, race, BMI, systolic and diastolic blood pressures, IOP, and prevalence of comorbidities.
Table 4 summarizes other AI-based glaucoma risk prediction studies that do not use visual field tests, CFPs, and OCT scans, alongside the current one. The model developed by Baxter et al.28 predicts patients at high risk of glaucoma progression as represented by the need for surgical intervention within 6 months. The model was trained on EHR data of patients already diagnosed with glaucoma. Their final dataset was relatively small with 385 total patients, all of whom had glaucoma, and 174 of whom underwent surgery. Therefore, their model would not be appropriate to determine individuals with glaucoma from an undiagnosed population. Mehta et al.29 trained their model on a labeled dataset with healthy and glaucomatous eyes using demographic, systemic, and ocular information. Since there is value in predicting glaucoma in the general population, they also applied the model on a cohort of fifty-five subjects without a glaucoma diagnosis at the time of data collection, all of whom subsequently developed glaucoma. Although their model predicts glaucoma with an accuracy of 75%, a cohort of fifty-five subjects is very small to assess its predictive capabilities. Tielsch et al.30 reported sensitivities and specificities of their logistic regression models for various decision thresholds (0.025, 0.05, 0.1, 0.15). They noted that the range of predicted probabilities from their model were below 0.2, and the sensitivity and specificity, with 0.15 as the probability cut-off, were 35% and 97%, respectively. By contrast, in the current study we used a standard probability threshold of 0.5 for the logistic regression classifier. Their data had 191 glaucoma cases and 5,054 normal cases, making it a highly imbalanced dataset. They have not reported whether any sampling techniques were employed prior to fitting the model to address the imbalance. This might have resulted in a model that is biased toward predicting the more frequently occurring class. As seen in Table 4, the current study mitigates some of the limitations addressed above.
Applying a permutation feature importance technique to the classifiers in the current study showed that IOP and age were the most predictive features in terms of increasing the F1 score. Systemic features, comorbidities, and racial data did not contribute to the predictive capabilities of the classifiers. However, this does not imply that the information is not important in terms of its association with glaucoma. The results of the permutation feature importance are specific to the current dataset and reflect the contribution of the features to the F1 score. Several large prevalence studies have documented African ancestry as a risk-factor for glaucoma with higher levels of IOP51,52,53. The classifiers’ lack of dependency on race is likely due to the very high prevalence of white participants in the AREDS database, which is a limitation of the current study. A more balanced racial distribution within the data may have yielded different results. Vascular conditions such as blood pressure have been investigated as possible risk-factors for glaucoma. However, results have been inconclusive. While the Egna-Neumarkt Study54 found an association between glaucoma and systemic hypertension, the Rotterdam study55 found that blood pressure was associated with high-tension glaucoma but not with normal-tension glaucoma. On the other hand, the Beijing Eye Study56 found that neither the systolic nor the diastolic blood pressures were significantly associated with the prevalence of glaucoma. To truly assess the importance of each feature, the dataset must be highly standardized and balanced across the different features. Additionally, majority of the AREDS participants had AMD, which is not representative of the normal population, and is a limitation of the current approach. While the feature permutation importance technique suggests that AMD may not be an important predictor for glaucoma, stratifying the dataset according to AMD categories may be a suitable approach to extract conclusive information. However, this was not pursued in the current study as it would reduce the number of samples in the dataset, making it prone to overfitting.
The aim of screening is to detect diseases early and treat conditions that have already produced pathological change but have not reached a stage where medical intervention is sought spontaneously57. Unlike diagnostic tools that require high sensitivity and specificity, screening can be relatively less accurate as it does not form the basis for treatment. Individuals identified through a positive screen test must be referred for diagnosis and necessary treatment. The asymptomatic nature of glaucoma results in 50%-90% undetected cases until advanced stages of the disease4,5,6 . The lack of regular visits to an ophthalmologist is one of the major causes of undiagnosed glaucoma58. Although these numbers support the need for glaucoma screening programs, they are not very common due to their high costs59 and the lack of an ideal screening method60,61. The Student Sight Savers Program implemented glaucoma screening for over 41,000 people in the United States44. The screening included a questionnaire to determine family history of glaucoma, IOP measurement, and visual function assessment. Sensitivity and specificity values for a positive screening in the individual tests were 48.6% and 68.6% for a confirmed family history of glaucoma, 22.1% and 78.6% for IOP greater than 21 mm Hg, and 58.1% and 98.6% for three or more abnormal locations on the visual field. As shown in the current study, a multivariable decision function learned through data-based techniques may provide better outcomes as compared to a fixed criterion for screening. Screening techniques must be cost-effective, simple, delivered rapidly, and should cause minimal discomfort to the subject57. With advances in machine learning and the relative simplicity of IOP measurement, there is a potential to address challenges that are specific to glaucoma screening and strongly support the necessity of further research into these technologies62.
In the future, glaucoma-specific AI-based tools will become available to clinicians for improved disease management, including the possibility of standalone or EHR-integrated referral decision support tools for primary care physicians and/or care management service providers. With the expanding power of computational resources, well curated datasets of better quality will likely make these tools highly accurate for screening and, potentially, diagnosis. The results presented here highlight the potential of these tools to play a future role in the early detection of glaucoma. These types of predictive models may make screening programs, referral decisions, and self-monitoring more efficient and effective, thereby increasing the chances of managing glaucoma more effectively, reducing the risk of vision loss, and improving quality of life.
Conclusion
In this study we evaluated multiple machine learning classifiers on their ability to predict future self-reported glaucoma based on data that can be obtained independent of an eye care provider. The goal was to explore the potential for combining readily accessible patient data with simple IOP measurement in a non-eye care setting to inform referral decisions and, thus, increase the number of glaucoma suspects evaluated early by an ophthalmologist. The three classifiers: logistic regression, support vector machine, and adaptive boosting were trained on data recorded when no subjects reported a glaucoma diagnosis. The classifiers were able to predict subjects who subsequently reported a confirmed glaucoma diagnosis, with sensitivities ranging from 52%–60% and specificities from 69%–77%. Further research into identifying more features to improve the predictive performance of such classifiers is necessary. We envision the use of such algorithms in developing tools to be used in primary care settings for advising patients to be evaluated by an eye care provider. We believe that such a tool would add value to the clinical care of patients at risk of glaucoma who might not otherwise visit an eye care provider without a referral and encouragement from their primary care provider.
References
Tham, Y. et al. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology 121, 2081–2090 (2014).
Tatham, A. J., Weinreb, R. N. & Medeiros, F. A. Strategies for improving early detection of glaucoma: the combined structure–function index. Clin. Ophthalmol. (Auckland, NZ) 8, 611 (2014).
Weinreb, R. N., Aung, T. & Medeiros, F. A. The pathophysiology and treatment of glaucoma: a review. JAMA 311, 1901–1911 (2014).
Leite, M. T., Sakata, L. M. & Medeiros, F. A. Managing glaucoma in developing countries. Arq. Bras. Oftalmol. 74, 83–84 (2011).
Hennis, A. et al. Awareness of incident open-angle glaucoma in a population study: the Barbados Eye Studies. Ophthalmology 114, 1816–1821 (2007).
Susanna, R., De Moraes, C. G., Cioffi, G. A. & Ritch, R. Why do people (still) go blind from glaucoma?. Transl. Vis.Sci. Technol. 4, 1 (2015).
Founti, P. et al. Overdiagnosis of open-angle glaucoma in the general population: the Thessaloniki Eye Study. Acta Ophthalmol. 96, e859–e864 (2018).
Gulshan, V. et al. Development and validation of a deep learning algorithm for detection of diabetic retinopathy in retinal fundus photographs. JAMA 316, 2402–2410 (2016).
Rajalakshmi, R., Subashini, R., Anjana, R. M. & Mohan, V. Automated diabetic retinopathy detection in smartphone-based fundus photography using artificial intelligence. Eye 32, 1138–1144 (2018).
Wang, Y., Zhang, Y., Yao, Z., Zhao, R. & Zhou, F. Machine learning based detection of age-related macular degeneration (AMD) and diabetic macular edema (DME) from optical coherence tomography (OCT) images. Biomed. Opt. Express 7, 4928–4940 (2016).
Lee, C. S. et al. Deep-learning based, automated segmentation of macular edema in optical coherence tomography. Biomed. Opt. Express 8, 3440–3448 (2017).
Maeda, N., Klyce, S. D., Smolek, M. K. & Thompson, H. W. Automated keratoconus screening with corneal topography analysis. Invest. Ophthalmol. Vis. Sci. 35, 2749–2757 (1994).
Abràmoff, M. D., Lavin, P. T., Birch, M., Shah, N. & Folk, J. C. Pivotal trial of an autonomous AI-based diagnostic system for detection of diabetic retinopathy in primary care offices. NPJ digital medicine. 1, 1–8 (2018).
Bizios, D., Heijl, A. & Bengtsson, B. Trained artificial neural network for glaucoma diagnosis using visual field data: a comparison with conventional algorithms. J. Glaucoma. 16, 20–28 (2007).
Chan, K. et al. Comparison of machine learning and traditional classifiers in glaucoma diagnosis. IEEE Trans. Biomed. Eng. 49, 963–974 (2002).
Goldbaum, M. H. et al. Comparing machine learning classifiers for diagnosing glaucoma from standard automated perimetry. Invest. Ophthalmol. Vis. Sci. 43, 162–169 (2002).
Sample, P. A. et al. Using machine learning classifiers to identify glaucomatous change earlier in standard visual fields. Invest. Ophthalmol. Vis. Sci. 43, 2660–2665 (2002).
Liu, S. et al. A deep learning-based algorithm identifies glaucomatous discs using monoscopic fundus photographs. Ophthalmol. Glaucoma 1, 15–22 (2018).
Christopher, M. et al. Performance of deep learning architectures and transfer learning for detecting glaucomatous optic neuropathy in fundus photographs. Sci. Rep. 8, 1–13 (2018).
Li, Z. et al. Efficacy of a deep learning system for detecting glaucomatous optic neuropathy based on color fundus photographs. Ophthalmology 125, 1199–1206 (2018).
Shibata, N. et al. Development of a deep residual learning algorithm to screen for glaucoma from fundus photography. Sci. Rep. 8, 1–9 (2018).
Yoo, T. K. & Hong, S. Artificial neural network approach for differentiating open-angle glaucoma from glaucoma suspect without a visual field test. Invest. Ophthalmol. Vis. Sci. 56, 3957–3966 (2015).
Maetschke, S. et al. A feature agnostic approach for glaucoma detection in OCT volumes. PLoS ONE 14, e0219126 (2019).
Medeiros, F. A., Jammal, A. A. & Thompson, A. C. From machine to machine: an OCT-trained deep learning algorithm for objective quantification of glaucomatous damage in fundus photographs. Ophthalmology 126, 513–521 (2019).
Muhammad, H. et al. Hybrid deep learning on single wide-field optical coherence tomography scans accurately classifies glaucoma suspects. J. Glaucoma 26, 1086 (2017).
Devalla, S. K. et al. Glaucoma management in the era of artificial intelligence. Br. J. Ophthalmol. 104, 301–311 (2020).
Fung, S. S., Lemer, C., Russell, R. A., Malik, R. & Crabb, D. P. Are practical recommendations practiced? A national multi-centre cross-sectional study on frequency of visual field testing in glaucoma. Br. J. Ophthalmol. 97, 843–847 (2013).
Baxter, S. L., Marks, C., Kuo, T., Ohno-Machado, L. & Weinreb, R. N. Machine learning-based predictive modeling of surgical intervention in glaucoma using systemic data from electronic health records. Am. J. Ophthalmol. 208, 30–40 (2019).
Mehta, P. et al. Automated detection of glaucoma with interpretable machine learning using clinical data and multi-modal retinal images. BioRxiv. (2020).
Tielsch, J. M. et al. A population-based evaluation of glaucoma screening: the Baltimore Eye Survey. Am. J. Epidemiol. 134, 1102–1110 (1991).
Group, T. The age-related eye disease study (AREDS): design implications AREDS report no 1. Control. Clin. Trials. 20, 573 (1999).
Koo, E. et al. Ten-year incidence rates of age-related cataract in the Age-Related Eye Disease Study (AREDS): AREDS report no. 33. Ophthalmic Epidemiol. 20, 71–81 (2013).
National Eye Institute (NEI) Age-Related Eye Disease Study (AREDS). https://www.ncbi.nlm.nih.gov/projects/gap/cgi-bin/variable.cgi?study_id=phs000001.v3.p1&phv=54046 (2012).
Lazarus, R. Eye Exams. https://www.optometrists.org/general-practice-optometry/guide-to-eye-exams/eye-exams/ (2020).
McKinney W. Data structures for statistical computing in python. In Proceedings of the 9th Python in Science Conference. Vol. 445, 56–61 (Austin, TX, 2010)
The pandas development team. pandas-dev/pandas: Pandas. (2020).
Chawla, N. V., Bowyer, K. W., Hall, L. O. & Kegelmeyer, W. P. SMOTE: synthetic minority over-sampling technique. J. Artif. Intell. Res. 16, 321–357 (2002).
Pedregosa, F. et al. Scikit-learn: Machine learning in Python. J. Mach. Learn. Res. 12, 2825–2830 (2011).
Chollet, F. Keras. https://keras.io (2015).
Friedman, J., Hastie, T. & Tibshirani, R. Additive logistic regression: a statistical view of boosting (with discussion and a rejoinder by the authors). Ann. Stat. 28, 337–407 (2000).
Breiman, L. Random forests. Mach. Learn. 45, 5–32 (2001).
Scikit-learn developers. Permutation feature importance. https://scikit-learn.org/stable/modules/permutation_importance.html#id2 (2020).
Saito, T. & Rehmsmeier, M. The precision-recall plot is more informative than the ROC plot when evaluating binary classifiers on imbalanced datasets. PLoS ONE 10, e0118432 (2015).
Salim, S., Netland, P. A., Fung, K. H., Smith, M. E. & Aldridge, A. Assessment of the student sight savers program methods for glaucoma screening. Ophthalmic Epidemiol. 16, 238–242 (2009).
College of Optometrists. Guidance on the referral of Glaucoma suspects by community optometrists. (2010).
Wilson, M. R. et al. Depression in patients with glaucoma as measured by self-report surveys. Ophthalmology 109, 1018–1022 (2002).
Shweikh, Y. et al. Measures of socioeconomic status and self-reported glaucoma in the UK Biobank cohort. Eye 29, 1360–1367 (2015).
Masís, M., Kakigi, C., Singh, K. & Lin, S. Association between self-reported bupropion use and glaucoma: a population-based study. Br. J. Ophthalmol. 101, 525–529 (2017).
Neustaeter, A., Vehof, J., Snieder, H. & Jansonius, N. M. Glaucoma in large-scale population-based epidemiology: a questionnaire-based proxy. Eye 35, 508–516 (2021).
Girard, M. J. & Schmetterer, L. Artificial intelligence and deep learning in glaucoma: Current state and future prospects. 257, 37–64 (2020).
Tielsch, J. M. et al. Racial variations in the prevalence of primary open-angle glaucoma: the Baltimore Eye Survey. JAMA 266, 369–374 (1991).
Leske, M. C., Connell, A., Schachat, A. P. & Hyman, L. The Barbados Eye Study: prevalence of open angle glaucoma. Arch. Ophthalmol. 112, 821–829 (1994).
Buhrmann, R. R. et al. Prevalence of glaucoma in a rural East African population. Invest. Ophthalmol. Vis. Sci. 41, 40–48 (2000).
Bonomi, L. et al. Vascular risk factors for primary open angle glaucoma: the Egna-Neumarkt Study. Ophthalmology 107, 1287–1293 (2000).
Dielemans, I. et al. Primary open-angle glaucoma, intraocular pressure, and systemic blood pressure in the general elderly population: the Rotterdam Study. Ophthalmology 102, 54–60 (1995).
Xu, L., Wang, Y. X. & Jonas, J. B. Ocular perfusion pressure and glaucoma: the Beijing Eye Study. Eye 23, 734–736 (2009).
Wilson, J. M. G., Jungner, G. & World Health Organization Principles and practice of screening for disease. 14–15 (1968).
Topouzis, F. et al. Factors associated with undiagnosed open-angle glaucoma: the Thessaloniki Eye Study. Am. J. Ophthalmol. 145, 327-335. e1 (2008).
Weinreb, R. N. Glaucoma Screening. (Kugler Publications, 2008).
Quigley, H. A. Current and future approaches to glaucoma screening. J. Glaucoma. 7, 210–220 (1998).
Shields, M. B. The challenge of screening for glaucoma. Am. J. Ophthalmol. 120, 793–795 (1995).
Tan, N. Y., Friedman, D. S., Stalmans, I., Ahmed, I. I. K. & Sng, C. C. Glaucoma screening: where are we and where do we need to go?. Curr. Opin. Ophthalmol. 31, 91–100 (2020).
Acknowledgements
The dataset used for the analyses described in this manuscript were obtained from the Age-Related Eye Disease Study (AREDS) Database found at https://www.ncbi.nlm.nih.gov/gap/ through dbGaP accession number phs000001.v3.p1. Funding support for AREDS was provided by the National Eye Institute (N01-EY-0-2127). We would like to thank the AREDS participants and the AREDS Research Group for their valuable contribution to this research.
Funding
National Eye Institute (Grant number 1R41EY031632-01).
Author information
Authors and Affiliations
Contributions
L.G. was responsible for the design of the study, data acquisition, and revising the manuscript. O.G.K. prepared and cleaned the data, developed the classifiers, and was involved in writing the manuscript. E.W.G. analyzed the data and was a major contributor in developing the classifiers and writing the manuscript. D.F. interpreted the data, provided technical guidance in choosing data to train classifiers, and substantively revised the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
Dr. Grace is a consultant for, and shareholder in, Lumata Health, USA. Dr. Wells-Gray is a full-time employee of Lumata Health, USA. Dr. Fleischman and Omkar G. Kaskar declare no potential conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kaskar, O.G., Wells-Gray, E., Fleischman, D. et al. Evaluating machine learning classifiers for glaucoma referral decision support in primary care settings. Sci Rep 12, 8518 (2022). https://doi.org/10.1038/s41598-022-12270-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-12270-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.