Abstract
The universal two-child policy (TCP; 2016) in China has affected many aspects of maternal-neonatal health. A tertiary hospital-based retrospective study (2011–2019) was used to find the association of these policy changes with maternal age and pregnancy outcomes in women with AMA (≥ 35 years) in the Hubei Province, China. The proportion of neonatal births to women with AMA increased by 68.8% from 12.5% in the one-child policy (OCP) period to 21.1% in the universal TCP period [aOR 1.76 (95% CI: 1.60, 1.93)]. In the univariate analysis, the proportion of preterm births (29.4% to 24.1%), low birth weight (LBW) (20.9% to 15.9%), and hypertensive disorders of pregnancy (HDP) (11.5% to 9.2%) significantly (p < 0.05) decreased in women with AMA from the OCP period to universal TCP period. However, the proportion of intrauterine growth restriction (IUGR) (0.2% to 0.7%) and gestational diabetes mellitus (GDM) (1.7% to 15.6%) was significantly (p < 0.05) increased over the policy changes. After adjusting for confounding factors, only the risk of GDM increased [aOR 10.91 (95% CI: 6.05, 19.67)] in women with AMA from the OCP period to the universal TCP period. In conclusion, the risk of GDM increased in women with AMA from the OCP period to the universal TCP period.
Similar content being viewed by others
Introduction
The Chinese government has been implemented an OCP since 1979, to control the rising population growth rate (540 million to 800 million during 1950–1970) and reduce the fertility rate1. This policy encouraged delayed childbearing, longer interpregnancy intervals, and fewer children which have stopped around 4000 million babies, and as a result, the birth rate has dropped significantly between 1.5 and 1.7 births per woman and has remained the same till now2. Meanwhile, the OCP had a profound impact on China’s population, societal, and health consequences, such as imbalance of sex ratio at birth, aging of the population, reduction of the workforce, and rising rate of C-section deliveries3,4,5,6.
In 2013, the Chinese government declared a partial TCP, allowing married couples to have a second child if either parent was a singleton. By easing certain restrictions in the OCP, the National Health and Family Planning Commission declared that the partial TCP would increase the supply of the workforce, reduce the aging population and sex-ratio imbalance. Following this, the Chinese government officially announced a universal TCP in October 2015, the 36-year OCP came to end2. According to hospital surveillance data, the number of live births had increased to 17.86 million per year by 2016, reflecting a 7.9% increase over 20157. After the universal TCP, the number of deliveries with obstetric complications and the number of pregnant women with elder maternal age increased8. However, long-term studies to investigate the maternal and neonatal health consequences especially in women with the AMA after the implementation of TCP are limited.
It has been estimated that after the universal TCP, an additional 90 million women in China will have a second child. Of these pregnant women, 60% are estimated to be older than 35 years, and 50% will be 40 years old9. It is well-established that women aged 35 years or older had a significantly increased risk of preeclampsia (PE), placenta previa, and adverse perinatal outcomes10. A retrospective study revealed that the trend of AMA increased in the Chinese population and was associated with higher odds of C-section, preterm births, low Apgar score, and perinatal mortality11. Moreover, as a result of universal TCP, the expected increasing number of older pregnant women will pose an extra challenge for health caregivers and obstetricians and can further increase maternal-neonatal consequences9.
The policy change has affected many aspects of China’s population and maternal-neonatal health. Several studies have investigated the impact of universal TCP on maternal-neonatal outcomes. For example, the impact of birth policy changes on pregnancy outcomes8, the sex ratio at birth3, maternity care9, maternal risk factors and pregnancy complications12, C-section rate13, women’s reproductive decision14, maternal-neonatal outcomes15, and prevalence of congenital defect7 has been reported. However, limited studies have reported the effect of universal TCP on maternal age pregnancy outcomes in women with AMA7,12. Therefore, we aimed to examine changes in maternal age and adverse pregnancy outcomes in women with AMA after the implementation of a universal TCP in Hubei province, China.
Results
Changes in maternal characteristics and complications
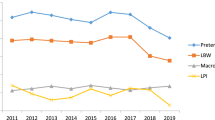
Among the total births (n = 23,051), 5653 births were in the OCP period (2011–2013), 8137 births in the partial TCP period (2014–2016), and 9261 births in the universal TCP period (2017–2019). The proportion of neonatal births to women aged < 30 decreased, whereas the proportion of neonatal births to women aged 30–34 years and women with AMA increased from OCP to universal TCP period. In total, 3956 (17.2%) births were to women with AMA. The proportion of neonatal births to women with AMA increased by 68.8%, from 12.5% in 2011–2013 to 21.1% in 2017–2019. The proportion of births to multiparous women increased from 18.5% in the OCP period to 27.7% in the universal TCP period. Pregnancy complications including HDP, abnormal placentation, and GDM significantly increased over the policy changes (p < 0.05). Moreover, after adjusting for confounding factors, the risk of AMA significantly increased in the universal TCP period relative to the OCP period (Tables 1, and 2).
Changes in neonatal outcomes
The proportion of neonates with preterm births, LBW, low Apgar scores, fetal distress, and congenital defects significantly decreased from 19.2%, 14.2%, 3.3%, 4.2%, and 1.4% in the OCP period to 18.3%, 13.2%, 3.0%, 2.4%, and 1.0% in the universal TCP period, respectively. However, perinatal mortality and neonates with IUGR significantly increased (p < 0.05) from the OCP period to the universal TCP period (Table 3).
Changes in adverse pregnancy outcomes in women with AMA
Among adverse pregnancy outcomes in women with AMA, the proportion of preterm births (from 29.4% to 24.1%), LBW (from 20.9% to 15.9%), low Apgar score (from 4.8% to 3.6%), fetal distress (from 4.5% to 2.2%), HDP (from 11.5% to 9.2%), and C-section (from 73.5% to 71.8%) significantly (p < 0.05) decreased from the OCP period to the universal TCP period. However, the proportion of IUGR (from 0.2% to 0.7%) and GDM (from 1.7% to 15.6%) significantly (p < 0.05) increased over the policy changes. Compared to the OCP period, after adjusting for confounding factors, the risk of GDM increased [aOR 10.91 (95% CI: 6.05, 19.67)] in women with AMA in the universal TCP period (Tables 4 and 5).
Discussion
In the present tertiary hospital-based retrospective study (2011–2019), we found changes in maternal age and adverse pregnancy outcomes in women with AMA after the implementation of the universal TCP. We observed that the proportion of neonatal births to women with AMA increased from the OCP period to the universal TCP period. The risk of AMA significantly increased in the universal TCP period compared with the OCP period. In the univariate analysis, among adverse pregnancy outcomes in women with AMA, the proportion of preterm births, LBW, HDP, and C-sections significantly decreased from the OCP period to the universal TCP period. However, the proportion of IUGR, fetal macrosomia, and GDM significantly increased over the policy changes. After adjusting for confounding factors, relative to the OCP period, the risk of GDM increased in women with AMA in the universal TCP period.
Our finding indicated a sharp increase (68.8%) in the proportion of women with AMA over the birth policy changes (from 12.5% in the OCP period to 21.1% in the universal TCP period). Although delayed childbearing has increased across the globe 16,17, the universal TCP in China might have encouraged the desire for a second child among older women. Based on the expected estimate, the universal TCP will encourage an additional 90 million women to have a second child and among these women, 60% will be older than 35 years 9. In accordance with our findings, some studies in China reported the impact of universal TCP on maternal age. For example, Li et al. 15 found that after implementing the universal TCP, around 5.40 million neonates were born between July 2016 and December 2017. During the study period, 9.1% and 5.8% monthly mean increase was found in multiparous mothers and mothers with AMA, respectively.
In Zhejiang Province, 7 women with AMA increased from 8.52% in 2013 to 15.82% in 2017. A sharp increase was found in births to women with AMA from 2013 to 2017. The new China’s universal TCP may have increased the tendencies toward fertility desires among older women. These findings were also evidenced in the Chinese national surveillance data indicating that after the relaxation of OCP, women with AMA were increased from 7.8 to 10.9% 18.
In Beijing, after the enactment of universal TCP, women of older maternal age (≥ 40 years) increased significantly from 2.2 to 3.6%8. In Hebei province3, the proportion of pregnant women aged ≥ 30 years increased from 24.7% (in the OCP period) to 36.9% (in the universal TCP period). It indicates that the introduction of universal TCP encouraged women of old age to have a second child which was prohibited before the implementation of the birth policy change. We speculate that the increase in AMA could be in multiparous women. The proportion of multiparous women has increased from the OCP period to the universal TCP period, showing that women who previously had no plans to have an additional child during their childbearing age chose to have a second child 8,15.
Based on the evidence, the implementation of universal TCP has caused a significant increase in the proportion of elderly parturient women3,7,8,15. These women of old age are likely to be associated with an increased risk of pregnancy complications such as HDP, abnormal placentation, GDM, C-section, and adverse perinatal outcomes19. In the univariate analysis, we observed that in women with AMA, the proportion of preterm births, LBW, C-section, and HDP were significantly declined from the OCP period to the universal TCP period. Moreover, after adjusting for confounding factors, the risks of these adverse pregnancy outcomes in women with AMA were not significantly increased after the implementation of the universal TCP. Zhang et al.8 reported that HDP, placenta previa, placental implantation, and severe postpartum hemorrhage were significantly increased after the introduction of universal TCP compared with the OCP period. They believed that the increase in pregnancy complications could be due to AMA because a large number of older women became pregnant after the implementation of universal TCP and the proportion of women with AMA increased.
However, our univariate analysis showed that although the proportion of women aged ≥ 35 years increased but, the proportion of some adverse perinatal outcomes (i.e. preterm births, LBW), HDP, and C-sections were significantly decreased in women with AMA after the announcement of the universal TCP. The improvement of these pregnancy outcomes regardless of the impact of AMA could be attributed to improvement in socioeconomic status (SES), health sector initiatives, and investment in health care services. We observed that SES in women with AMA improved from the OCP period to the TCP period (table S1). Women of higher SES status were associated with a lower incidence of LBW in Shaanxi, China20. Similar associations between maternal SES and pregnancy outcomes were reported in many previous studies21,22.
The Chinese government has increased health expenditure per capita from US$ 53 in 1995 to US$ 480 in 2012 and achieved remarkable goals in the last two decades23. To better deliver and manage the basic public health services, the Chinese government issued three editions of National Basic Public Service Specifications in 2009, 2011, and 2017, respectively. These service packages of the program consist of health education, health management of children aged 0–6, and maternal health care24. Therefore, the strengthening and improvement of the three-tier medical and health services network for pregnant women in China has proven to decline the trends of adverse perinatal outcomes25.
In the univariate analysis we showed that after the implementation of universal TCP, the proportion of GDM significantly increased in women with AMA. Moreover, after adjusting for confounding factors the risk of GMD significantly increased by tenfold in women with AMA in the universal TCP period. It is obvious that an increase in maternal age results in a higher incidence of GDM. In our findings, the proportion of GDM in women with AMA increased from 1.7% (in the OCP period) to 15.6% (in the universal TCP period). Zhang et al.8 also found that GDM increased from 23.1% (in the OCP period) to 25.3% (in the universal TCP period). However, their study did not report the proportion of GDM in women with AMA. A retrospective study conducted by Teng et al.12 examined changes in maternal age and pregnancy outcomes after the universal TCP. They reported that the incidence of GDM increased from 18.72% in 2015 to 25.59% in 2017. The proportion of GDM in women with AMA increased from 3.90% in 2015 to 5.48% in 2016 and then decreased to 0.35% in 2017.
AMA is an independent risk factor for GDM26. As maternal age increases, the prevalence of GDM increases simultaneously. The prevalence of GDM in women aged < 25 years, 25–29 years, 30–34 years, 35–39 years and > 40 years, were 6.6%, 7.3%, 8.8%, 16.7%, and 35.2%, respectively 27. After adjusting for potential confounding factors, the risk of GDM increased with maternal age 28. In the Chinese population, AMA increased the risk of GMD by 4.8-fold29. Moreover, in another Chinese population, women with AMA associated with a 3.6-fold increased risk of GDM30. The higher risk of GDM in women with AMA could be explained by the progressive vascular endothelial damage in women of older ages31, reduction in insulin sensitivity, impaired glucose tolerance32, and deterioration of pancreatic β-cell function 33 as maternal age increases.
Moreover, in our findings, the higher risk of GDM in women with AMA could be due to a sedentary lifestyle and higher body mass index (BMI). In general, women of professional services have higher tendencies of a sedentary lifestyle. In our findings, in women with AMA, the trend of professional services (i.e. doctors, nurses, accountants, teachers, lawyers, and actresses) increased from 27.1% in the OCP period to 49.1% in the universal TCP period (table S1). A sedentary lifestyle has become a significant problem across the globe and has been linked with a range of chronic health condition34 including metabolic dysfunction and impaired blood sugar regulation35. In the Brazilian pregnant women population, the sedentary lifestyle was associated with higher odds of GMD after adjusting for several confounding factors (aOR 1.9-fold)36. Similarly, in a population-based cross-sectional study the sedentary lifestyle was associated with a higher risk of GDM among Chinese pregnant women37. The high BMI of pregnant women is associated with an increased risk of GMD38. However, our study lacks data on the BMI of pregnant women which is one of the limitations of our study.
Our study had certain limitations which are worth mentioning. The study design was retrospective. Our data analysis is based on a single-center tertiary hospital, which is the potential selection bias in this study. We also excluded the women with chronic hypertension which could limit the generalizability of our findings. Moreover, we could not distinguish the C-section whether it was an elective or an emergency C-section. As a tertiary-level hospital, many pregnant women with severe pregnancy complications are transferred to our hospital, resulting in a relatively high C-section rate in women with AMA. Therefore, our results cannot be generalized to the whole population and pregnant women living in other regions of China.
Conclusion
In summary, the proportion of neonatal births to women with AMA increased from the OCP period to the universal TCP. The risk of AMA significantly increased in the universal TCP relative to the OCP period. After adjusting for confounding factors, the risk of GDM increased in women with AMA in the universal TCP period compared with the OCP period. As we were working on the impact of TCP on maternal age and adverse pregnancy outcomes in women with AMA, the Chinese government announced the tree-child policy39. Therefore, this study will help obstetricians and clinicians to pay serious attention to the increasing trend of AMA and associated adverse pregnancy outcomes after the three-child policy.
Material and methods
Study population
A tertiary hospital-based retrospective study was conducted in the Wuhan University Renmin Hospital, Department of Obstetrics and Gynecology, Hubei, China from January 2011 to December 2019. The data was collected and documented in the obstetrics register and electronic database by trained nurses during individual examinations in the Gynecology and Obstetrics Department. The study protocol was approved by the Ethical Review Board of Renmin Hospital (ID: WDRY2019–K034) in accordance with the Declaration of Helsinki. The need for informed consent, according to national legislation, was waived by the Ethical Review Board of Renmin Hospital because this was a retrospective cohort study.
Inclusion and exclusion criteria
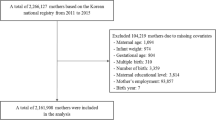
A total of 23,051 singleton pregnant women were selected for the study. We excluded missing data on maternal age, pre-pregnancy body weight, neonatal gender, birth weight, birth length, and gestational age40. Pregnant women aged ≤ 18 years old, with chronic hypertension, and twin neonates were also excluded from the data analysis as shown in Fig. 1.
Collection of data on maternal traits
Data regarding maternal traits were collected from the obstetrics register including maternal age, parity, prepregnancy body weight, gestational age, education, occupation, and pregnancy complications. At the time of delivery, based on age, pregnant women were divided into three groups (i) < 30 years, (ii) 30–34 years, (iii), and ≥ 35 years. Gestational age was calculated by the date of the last known menstrual period and confirmed by ultrasound examination during the first and second trimesters. Based on education, they were classified as ≤ 8 years (low), 9–12 years (middle), and ≥ 13 years (higher). Maternal occupations were categorized as (i) housewives, (ii) professional services (doctors, nurses, accountants, teachers, lawyers, and actresses), and (iii) manual workers (farmers, waitresses, drivers, and factory workers).
Definition of pregnancy complications and perinatal birth outcomes
Gestational hypertension (GH) is defined as having blood pressure greater than 140/90 mmHg without proteinuria after 20th weeks of gestation41. PE is defined as elevated blood pressure 140/90 mmHg with proteinuria (albumin > 0.3 g in 24 h) after the 20th week of gestation42. Sever PE referred to having a blood pressure higher than 160/110 mmHg with proteinuria (albumin > 5 g in 24 h) after the 20th week of gestation43. Placenta previa is defined as suboptimal placental implantation near or over the cervical opening44. Placental abruption referred to the early separation of the placenta before childbirth45. Neonatal birth outcomes were recorded immediately after neonatal birth including birth weight in grams using an electronic infant scale, birth length in centimeter using a standard measuring board for the neonate. Preterm birth is defined as a neonate born before 37 completed weeks or fewer than 259 days from the first date of a woman’s last menstrual period46. Perinatal mortality is defined as the combination of late fetal mortality (stillbirths) and early neonatal mortality (0–6 days of life)47. Fetal macrosomia is defined as birth weight ≥ 4000 g and LBW is defined as birth weight < 2500 g48. IUGR is defined as a condition of fetal growth that is below the 10th percentile for its gestational age and does not reach its genetically predetermined growth potential49. Apgar score was determined by evaluating the newborn baby on five simple criteria on a scale from zero to two, then summing up the five values obtained. Apgar score was recorded at 1 min and 5 min after birth. Apgar score was divided into two categories (i) low Apgar score (< 7), and (ii) normal Apgar score (≥ 7)50. Fetal distress is defined as a pathophysiological condition in which the fetus is suffering from insufficient oxygen supply51. The ponderal index was determined by weight in gm / (length in cm)3 × 100. The ponderal index between 2.5 and 3.0 was considered normal between 2.0 and 2.5 marginal, and a neonate with a ponderal index less than 2.0 was considered a low ponderal index (LPI)52. Congenital defects are defined as abnormalities in the structure of neonatal body parts that occur during intrauterine development53.
Potential confounding factors
Cofounding factors were selected based on previous literature which is associated with both exposure and perinatal birth outcome y42. The confounding factors included in this analysis were maternal education, occupation, pre-pregnancy body weight (≤ 45 kg and ≥ 91 kg), parity, and neonatal gender.
Statistical analysis
The categorical and binary variables are presented as number (n) and percentage (%). We divided the study period into OCP (2011–2013), partial TCP (2014–2016), and universal TCP (2017–2019). Changes in maternal age and maternal-neonatal factors in women of AMA were estimated using chi-square tests. To estimate the effect size, Cramer’s V was used in chi-square tests. Trend analysis (chi-square tests) was used to estimate the change in maternal age over the time period of policy changes. Additionally, we restricted our analysis to women aged ≥ 35 years to know changes in pregnancy complications and adverse perinatal outcomes in women with AMA over the time frame of policy changes. Binary logistic regression analysis was used to calculate odds ratios (ORs) and 95% confidence interval (CI) to examine the association of universal TCP with the risk of changes in maternal age groups and risk of pregnancy complication and adverse perinatal outcomes in women with AMA, while the OCP period being defined as the reference period. P < 0.05 was taken statistically significant. The data were analyzed using SPSS (Statistical Package for Social Sciences) for window version 22 (IBM Corporation, Chicago, USA).
Ethics approval and consent to participate
The study protocol was approved by the Ethical Review Board of Renmin Hospital (ID: WDRY2019–K034) in accordance with the Declaration of Helsinki.
Informed consent
The need for informed consent, according to national legislation, was waived by the Ethical Review Board of Renmin Hospital because this was a retrospective cohort study.
Data availability
All data analyzed during this study are included in this article.
References
Hesketh, T., Lu, L. & Xing, Z. W. The effect of China’s one-child family policy after 25 years. N. Engl. J. Med. 353, 1171–1176 (2005).
Zeng, Y. & Hesketh, T. The effects of China’s universal two-child policy. The Lancet 388, 1930–1938 (2016).
Fan, S. et al. How does the two-child policy affect the sex ratio at birth in China? A cross-sectional study. BMC Public Health 20, 1–11 (2020).
Hesketh, T., Zhou, X. & Wang, Y. The end of the one-child policy: lasting implications for China. JAMA 314, 2619–2620 (2015).
Mu, Y. et al. Prior caesarean section and likelihood of vaginal birth, 2012–2016, China. Bull. World Health Organ. 96, 548 (2018).
Barrows, S. P. China’s one-child policy. JAMA 315, 2349–2350 (2016).
Zhang, X. et al. Changes in maternal age and prevalence of congenital anomalies during the enactment of China’s universal two-child policy (2013–2017) in Zhejiang Province, China: An observational study. PLoS Med. 17, e1003047 (2020).
Zhang, H.-X., Zhao, Y.-Y. & Wang, Y.-Q. Analysis of the characteristics of pregnancy and delivery before and after implementation of the two-child policy. Chin. Med. J. 131, 37 (2018).
Cheng, P. & Duan, T. China’s new two-child policy: maternity care in the new multiparous era. BJOG 123, 7–9 (2016).
Blomberg, M., Tyrberg, R. B. & Kjølhede, P. Impact of maternal age on obstetric and neonatal outcome with emphasis on primiparous adolescents and older women: a Swedish Medical Birth Register Study. BMJ open 4, e005840 (2014).
Liou, J.-D., Hsu, J.-J., Lo, L.-M., Chen, S.-F. & Hung, T.-H. Advanced maternal age and adverse perinatal outcomes in an Asian population. Eur. J. Obstetr. Gynecol. Reproduct. Biol. 148, 21–26 (2010).
Teng, X. & Pan, S. The changing situation about maternal age, risk factors and pregnancy outcomes after the two-child policy: A retrospective cohort study. Ann. Palliat. Med. 9, 824–834 (2020).
Yan, J. et al. The trend of caesarean birth rate changes in China after ‘universal two-child policy’era: A population-based study in 2013–2018. BMC Med. 18, 1–9 (2020).
Shen, Y. & Jiang, L. Reproductive choices of highly educated employed women with two children under the universal two-child policy. J. Fam. Issues 41, 611–635 (2020).
Li, H.-t. et al. Association of China’s universal two child policy with changes in births and birth related health factors: national, descriptive comparative study. BMJ 366, 14680 (2019).
Behboudi-Gandevani, S., Farahani, F. K. & Jasper, M. The perspectives of Iranian women on delayed childbearing: A qualitative study. J. Nursing Res 23, 313–321 (2015).
Goisis, A. & Sigle-Rushton, W. Childbearing postponement and child well-being: A complex and varied relationship?. Demography 51, 1821–1841 (2014).
Liang, J. et al. Relaxation of the one child policy and trends in caesarean section rates and birth outcomes in China between 2012 and 2016: Observational study of nearly seven million health facility births. BMJ 360, k817 (2018).
Li, Q. & Deng, D. New medical risks affecting obstetrics after implementation of the two-child policy in China. Front. Med. 11, 570–575 (2017).
Pei, L., Kang, Y., Zhao, Y., Cheng, Y. & Yan, H. J. M. Changes in socioeconomic inequality of low birth weight and Macrosomia in Shaanxi Province of Northwest China, 2010–2013: A cross-sectional study. Medicine, 95, e2471 (2016).
Madden, D. J. J. O. B. S. The relationship between low birth weight and socioeconomic status in Ireland. J. Biosoc. Sci. 46, 248–265 (2014).
Mortensen, L. H., Diderichsen, F., Smith, G. D., Andersen, A. N. J. J. O. E. & Health, C. Time is on whose side Time trends in the association between maternal social disadvantage and offspring fetal growth. A study of 1 409 339 births in Denmark, 1981–2004. J. Epidemiol. Community. Health. 63, 281–285 (2009).
Ahmed, S. M. et al. Cross-country analysis of strategies for achieving progress towards global goals for women’s and children’s health. 94, 351 (2016).
Wang, L. et al. The development and reform of public health in China from 1949 to 2019. Global. Health 15, 1–21 (2019).
Backman, G. et al. Health systems and the right to health: an assessment of 194 countries. The Lancet 372, 2047–2085 (2008).
Pallasmaa, N., Ekblad, U., Gissler, M. & Alanen, A. The impact of maternal obesity, age, pre-eclampsia and insulin dependent diabetes on severe maternal morbidity by mode of delivery—a register-based cohort study. Arch. Gynecol. Obstet. 291, 311–318 (2015).
Karcaaltincaba, D. et al. Prevalence of gestational diabetes mellitus evaluated by universal screening with a 75-g, 2-hour oral glucose tolerance test and IADPSG criteria. Int. J. Gynecol. Obstet. 138, 148–151 (2017).
Bianco, A. et al. Pregnancy outcome at age 40 and older. Obstet. Gynecol. 87, 917–922 (1996).
Wu, L. et al. Prevalence of gestational diabetes mellitus and associated risk factors in pregnant Chinese women: A cross-sectional study in Huangdao, Qingdao, China. Asia Pac. J. Clin. Nutr. 27, 383 (2018).
Dong, B. et al. The effect of pre-pregnancy body mass index and excessive gestational weight gain on the risk of gestational diabetes in advanced maternal age. Oncotarget 8, 58364 (2017).
Crawford, B. S., Davis, J. & Harrigill, K. Uterine artery atherosclerotic disease: histologic features and clinical correlation. Obstet. Gynecol. 90, 210–215 (1997).
Fulop, T., Larbi, A. & Douziech, N. Insulin receptor and ageing. Pathol. Biol. (Paris) 51, 574–580 (2003).
Szoke, E. et al. Effect of aging on glucose homeostasis: accelerated deterioration of β-cell function in individuals with impaired glucose tolerance. Diab. Care 31, 539–543 (2008).
Chau, J. Y. et al. Daily sitting time and all-cause mortality: A meta-analysis. PLoS ONE 8, e80000 (2013).
Chastin, S. F., Egerton, T., Leask, C. & Stamatakis, E. J. O. Meta-analysis of the relationship between breaks in sedentary behavior and cardiometabolic health. Obesity 23, 1800–1810 (2015).
do Nascimento, G. R., Borges, M. d. C., Figueiroa, J. N., Alves, L. V. & Alves, J. G. J. S. o. m. Physical activity pattern in early pregnancy and gestational diabetes mellitus risk among low-income women: A prospective cross-sectional study. 7, 2050312119875922 (2019).
Leng, J. et al. Physical activity, sedentary behaviors and risk of gestational diabetes mellitus: A population-based cross-sectional study in Tianjin, China. Eur. J. Endocrinol. 174, 763–773 (2016).
Kim, S. Y. et al. Percentage of gestational diabetes mellitus attributable to overweight and obesity. Am. J. Public Health 100, 1047–1052 (2010).
Tatum, M. J. T. L. China’s three-child policy. The Lancet 397, 2238 (2021).
Kang, H. The prevention and handling of the missing data. Korean J. Anesthesiol. 64, 402 (2013).
Program, N. H. B. P. E. Report of the national high blood pressure education program working group on high blood pressure in pregnancy. Am. J. Obstet. Gynecol. 183, s1–s22 (2000).
Xiong, X., Demianczuk, N. N., Saunders, L. D., Wang, F.-L. & Fraser, W. D. Impact of preeclampsia and gestational hypertension on birth weight by gestational age. Am. J. Epidemiol. 155, 203–209 (2002).
Schroeder, B. M. ACOG practice bulletin on diagnosing and managing preeclampsia and eclampsia. Am. Fam. Physician 66, 330 (2002).
Kancherla, V., Räisänen, S., Gissler, M., Kramer, M. R. & Heinonen, S. Placenta previa and risk of major congenital malformations among singleton births in Finland. Birth Defects Res. A 103, 527–535 (2015).
Tikkanen, M. Placental abruption: epidemiology, risk factors and consequences. Acta Obstet. Gynecol. Scand. 90, 140–149 (2011).
Blencowe, H. et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. The Lancet 379, 2162–2172 (2012).
Cartlidge, P. H. & Stewart, J. H. Effect of changing the stillbirth definition on evaluation of perinatal mortality rates. The Lancet 346, 486–488 (1995).
Brown, T. M., Cueto, M. & Fee, E. A transição de saúde pública’internacional’para’global’e a Organização Mundial da Saúde. História, Ciências, Saúde-Manguinhos 13, 623–647 (2006).
Battaglia, F. C. & Lubchenco, L. O. A practical classification of newborn infants by weight and gestational age. J. Pediatr. 71, 159–163 (1967).
Casey, B. M., McIntire, D. D. & Leveno, K. J. The continuing value of the Apgar score for the assessment of newborn infants. N. Engl. J. Med. 344, 467–471 (2001).
Liu, H. et al. Maternal exposure to fine particulate matter and the risk of fetal distress. Ecotoxicol. Environ. Saf. 170, 253–258 (2019).
Landmann, E., Reiss, I., Misselwitz, B. & Gortner, L. Ponderal index for discrimination between symmetric and asymmetric growth restriction: percentiles for neonates from 30 weeks to 43 weeks of gestation. J. Matern. Fetal Neonatal Med. 19, 157–160 (2006).
Yu, M. et al. The survey of birth defects rate based on birth registration system. Chin. Med. J. 128, 7 (2015).
Acknowledgements
We are thankful to the staff of the Obstetrics and Gynecology department of Renmin Hospital, Wuhan for helping in data collection.
Funding
This work is supported by a Henan province science and technology attack plan project (grant no: 212102310044).
Author information
Authors and Affiliations
Contributions
H.L, N & C.F: Conceptualization, Methodology, Software, Writing- Original draft preparation and Formal analysis., S.Y, I.U.H, S.M & G.N, S.K: Methodology, Data curation, Writing- Reviewing, Editing. N, S.Y, H.L: Validation, investigation, Visualization, Supervision.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, H., Nawsherwan, Fan, C. et al. Changes in adverse pregnancy outcomes in women with advanced maternal age (AMA) after the enactment of China’s universal two-child policy. Sci Rep 12, 5048 (2022). https://doi.org/10.1038/s41598-022-08396-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-08396-6
This article is cited by
-
Perceptions of Chinese women with a history of gestational diabetes regarding health behaviors and related factors: a directed qualitative content analysis
BMC Public Health (2024)
-
The effect of China’s many-child policy on the number of births and the prevalence of serious teratogenic and disabling defects in Hunan Province
BMC Public Health (2023)
-
Trimester-specific reference intervals and profile of coagulation parameters for Chinese pregnant women with diverse demographics and obstetric history: a cross-sectional study
BMC Pregnancy and Childbirth (2023)
-
Age-specific effects on adverse pregnancy outcomes vary by maternal characteristics: a population-based retrospective study in Xiamen, China
BMC Public Health (2023)
-
The possible impact of the universal two-child policy on pregnancy outcomes
Archives of Gynecology and Obstetrics (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.